There is hardly a person who has not suffered from tonsillitis at least once in his life. The causative agents of tonsillitis are staphylococci, streptococci and pneumococci. There are acute tonsillitis and chronic tonsillitis.
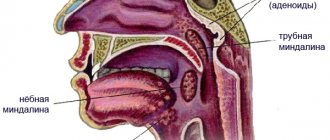
Acute tonsillitis (or tonsillitis) is an infectious disease that affects the palatine tonsils, as well as the lingual, laryngeal and nasopharyngeal tonsils.
In acute tonsillitis, the throat hurts, it is difficult to swallow, the body temperature rises, general weakness, chills, aching joints, and headache appear. With proper treatment and compliance with the instructions of the otorhinolaryngologist, the disease is cured in 5-7 days.
1
Diagnosis of chronic tonsillitis in MedicCity
2 Diagnosis of chronic tonsillitis in MedicCity
3 Diagnosis of chronic tonsillitis in MedicCity
Chronic tonsillitis is a common infectious disease in which the focal infection is in the palatine tonsils. The formation of a chronic inflammatory focus in the tonsils occurs due to prolonged exposure of microbes to the lymphoid tissue of the tonsils.
Chronic tonsillitis is characterized by periodic exacerbations - sore throats, but a non-angina form of the disease also occurs.
Tonsillitis in children
According to statistics, almost half of weakened children fall ill with acute tonsillitis (tonsillitis). The tonsils in children begin to become very inflamed; the enlarged tonsils cease to perform their function - to protect the body and produce active substances that can suppress infection that penetrates from the outside.
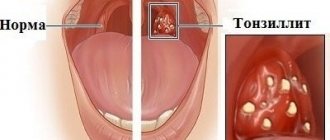
Acute tonsillitis in children leads to fever, headache, weakness, loss of appetite, and inability to swallow food due to severe sore throat as a result of inflammation of the tonsils. Purulent plaque on the tonsils explains the putrid odor from the mouth. With tonsillitis, the tonsils in children decrease or increase in size, plugs appear in the tonsils, scars appear, and the lacunae of the tonsils are enlarged.
EPIDEMIOLOGY
The prevalence of chronic tonsillitis among the population varies widely.
In adults it ranges from 5–6 to 37%, and in children – from 15 to 63%. In the group of frequently ill children, chronic tonsillitis is 40% or higher. It must be borne in mind that between exacerbations, as well as in the nonanginal form of chronic tonsillitis, the symptoms of the disease are largely familiar and little or do not bother the patient at all, which significantly underestimates the actual prevalence of the disease. Often chronic tonsillitis is detected only in connection with the examination of the patient for some other disease, in the development of which chronic tonsillitis plays a large role. In many cases, chronic tonsillitis, remaining unrecognized, has all the negative factors of a tonsillar focal infection, weakens a person’s health, and worsens the quality of life.
ETIOLOGY AND PATHOGENESIS
Etiology
Among the bacterial flora that constantly grows in the palatine tonsils, the causative agents of tonsillitis can be streptococci, staphylococci and their associations, pneumococci, H. influenzeae, M. Catarrhalis.
The main etiological factor in the development of chronic tonsillitis and its complications remains group A beta-hemolytic streptococcus.
According to foreign and domestic researchers, in the etiology of chronic tonsillitis its share is 30% in children and 10–15% in adults. Streptococci of serological groups C and G are less common.
Next in frequency of occurrence are Staphylococcus aureus, hemolytic Staphylococcus and obligate anaerobic microorganisms; intracellular and membrane parasites (chlamydia, mycoplasma), often detected in chronic tonsillitis, deserve special attention.
A lot of data has been accumulated on the frequent connection between two factors in chronic tonsillitis: streptococcal infection and predisposition to it.
In families of patients with chronic tonsillitis, there is a higher frequency of carriage of streptococcal infection and the prevalence of chronic tonsillitis than in the general population.
Risk factors for chemotherapy:
- age;
- climatic and geographical conditions;
- state of local and general immunity;
- the frequency of respiratory diseases that lead to the loss of the normal structure of the lymphoid organ and the development of hypoxic changes;
- childhood infections: measles, scarlet fever, chicken pox;
- malnutrition and poor living conditions;
- state of the environment, including the level of air pollution from industrial waste;
- carious teeth, chronic purulent sinusitis, difficulty nasal breathing (hypertrophic rhinitis, adenoids).
Pathogenesis
According to pathogenesis, two forms are distinguished:
a) chronic tonsillitis as a consequence of repeated sore throats suffered in childhood, which disrupted the mechanisms of tissue immunity and created favorable conditions for the constant vegetation of pathogenic flora in the palatine tonsils;
b) primary developing chronic tonsillitis without acute anginal excesses.
Both forms of development of chronic tonsillitis are caused by a number of external and internal reasons.
In healthy people, various microorganisms are constantly present in the lacunae of the tonsils; this is where the presentation of antigens (AG) and the induction of an immune response occur. In the lacunae, Ags are recognized, phagocytosed and presented to B and T cells of the lymphoid tissue of the tonsils, where antigen-specific T and B cell reactions develop. Under normal conditions, microorganisms (MO) living on the mucous membrane of the oropharynx cannot penetrate into the deep layers of tissue and develop an infectious-inflammatory process.
The introduction of MO is due to the synthesis of invasive enzymes, which is possible during the formation of dysbiosis of the mucous membrane due to various unfavorable factors, the main of which is the inhibition of specific and nonspecific factors of the natural resistance of the macroorganism.
According to many researchers, one of the factors in the occurrence of chronic tonsillitis is the anatomical structure of the palatine tonsils, in particular the presence of deep crypts in which associations of pathogenic flora accumulate, multiply and have a necrobiotic effect on the surrounding lymphadenoid tissue.
An important condition for the development of chronic inflammation in the palatine tonsils is the anatomical conditions in which they are located: covering the lacunae with triangular and semilunar folds, deep niches of the palatine tonsils and their pinching between the anterior and posterior palatine arches, the presence of additional niches in which tonsil tissue is located. Under these conditions, the mucous glands that produce washing and disinfecting mucus cease to perform this important role due to obstruction.
Another factor contributing to the development of chronic tonsillitis is impaired nasal breathing. Inhaling cooled air through the mouth or drinking cold drinks plays a dual pathogenetic role - it directly affects tissue biochemical processes (reduces or even stops them) and causes a number of physiological reactions (cold vascular spasm, reflex disturbance of the autonomic regulation of trophic functions). In the pathogenesis of chronic tonsillitis, a significant role is played by violations of the protective mechanism that delimits the source of inflammation. When the barrier function is partially or completely lost, the focus of inflammation turns into an entrance gate for infection, and damage to a number of other organs and systems becomes possible, which is determined by the reactive properties of the body.
Speaking about the pathogenesis of chronic tonsillitis, it is also important to note that the natural role of the palatine tonsils in the formation of immunity is completely distorted, because with chronic inflammation in the tonsils, new antigens are formed under the influence of pathological protein complexes (virulent microbes, endo- and exotoxins, products of destruction of tissue and microbial cells, etc.), which causes the formation of autoantibodies against one’s own tissues.
Chronic tonsillitis often causes the development of other diseases or aggravates their course. Numerous studies conducted over the past decades confirm the connection of chronic tonsillitis with rheumatism, polyarthritis, acute and chronic glomerulonephritis. sepsis, systemic diseases, dysfunction of the pituitary gland and adrenal cortex, neurological diseases, acute and chronic diseases of the bronchopulmonary system, etc.
CLASSIFICATION
In domestic medicine, two classifications of chronic tonsillitis that have practical significance are most widespread: I.B. Soldatova (1975) with the division of chronic tonsillitis into compensated and decompensated forms.
The compensated form of chronic tonsillitis is characterized by local signs of chronic inflammation of the tonsils without a pronounced general reaction, a history of periodic acute streptococcal tonsillopharyngitis (no more than once every 1–2 years) or a nonanginal course of inflammation; the decompensated form is characterized by frequent ATP (several times a year), history of paratonsillitis and paratonsillar abscesses, the presence of associated (metatonsillar) diseases.
B.S. Preobrazhensky and V.T. Palchuna (1964) with a division into a simple form and two toxic-allergic forms.
The simple (compensated) form of chronic tonsillitis is characterized by the absence of a visible reaction from the whole organism, exacerbations (repeated tonsillitis) and occurs only with local symptoms, subjective complaints and objective (local) signs of the disease.
Toxic-allergic forms occur with local and general complications.
Toxic-allergic form I (TAF 1) is characterized by a history of periodic sore throats, all the above-mentioned signs of a simple form of chronic tonsillitis in combination with general toxic-allergic phenomena.
Toxic-allergic form II (TAF II) is characterized by more pronounced signs of the first toxic-allergic form.
DIAGNOSIS
Clinical signs and symptoms
Patients with chronic tonsillitis complain of frequent acute streptococcal tonsillopharyngitis, discomfort in the throat, discharge of “purulent” plugs and bad breath.
In chronic tonsillitis, moderate symptoms of general intoxication are observed - such as periodic or constant low-grade body temperature, sweating, increased fatigue, incl. mental, sleep disturbance, moderate dizziness and headache, loss of appetite, etc.
One of the most reliable signs of the disease is the presence of a history of acute streptococcal tonsillopharyngitis. In this case, it is necessary to find out the frequency and severity of ATP from the patient.
Physical examination
There is no pathognomonic symptom of chronic tonsillitis.
The diagnosis of chronic tonsillitis is established based on the presence of several subjective and objective signs of the disease.
Local signs
The most reliable local signs of the disease:
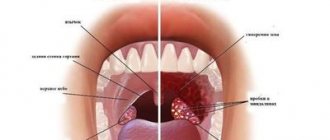
- hyperemia and roller-like thickening of the edges of the palatine arches;
- cicatricial adhesions between the tonsils and palatine arches;
- loosened or scarred and hardened tonsils;
- caseous-purulent plugs or liquid pus in the lacunae of the tonsils;
- regional lymphadenitis – enlargement of the cervical lymph nodes.
General signs:
- low-grade fever (intermittent);
- tonsillogenic intoxication (weakness, weakness, fatigue, etc.);
- joint pain and functional disorders of the heart against the background of tonsillogenic intoxication.
Clinical and diagnostic characteristics of individual forms of chronic tonsillitis are presented in table. 1.
Possible regional diseases caused by chronic tonsillitis:
- paratonsillar, parapharyngeal and retropharyngeal abscesses;
- cervical lymphadenitis;
- mediastenitis;
- inflammation of the middle ear and paranasal sinuses.
Common diseases:
- Acute and chronic tonsillogenic sepsis.
- Rheumatism, the formation of heart defects.
- Glomerulonephritis.
- Infectious nonspecific polyarthritis.
- IgA nephropathy.
- Psoriasis.
- PANDAS – pediatric autoimmune neuropsychiatric associated with streptococcal infection (children's autoimmune neuropsychiatric disorders associated with streptococcal infection).
- Movement disorders (chorea, tics, dystonia, parkinsonism).
- Mental disorders (especially emotional).
- Sleep disorders.
- Infectious and allergic diseases of the urinary system, joints and other organs and systems.
Examples of diagnosis formulation:
- Chronic tonsillitis, simple form.
- Chronic tonsillitis, toxic-allergic form of the II degree, rheumatism in the inactive phase.
Laboratory and instrumental studies
Basic laboratory tests:
- Complete blood count - hypochromic anemia, neutrophilic leukocytosis, monocytopenia, leukopenia, and increased ESR can be detected. However, more often chronic tonsillitis is not accompanied by changes in the peripheral blood.
- Biochemical blood test (rheumatic tests) (SBR, RF, ASLO).
- General urine analysis.
- Bacteriological examination of the contents of tonsil lacunae (detection of pathogenic and opportunistic microorganisms and the most common pathogen - group A beta-hemolytic streptococcus).
Instrumental studies
Pharyngoscopy: the presence of local signs - liquid pus or caseous plugs in the lacunae, Giese's sign - hyperemia of the edges of the anterior arches, Zach's sign - swelling of the edges of the upper parts of the palatine arches, Preobrazhensky's sign - infiltration of the edges of the anterior arches, as well as fusion and adhesions of the tonsils with the arches.
Additional diagnostic measures:
- Cytomorphological study of discharge lacunae.
- Methods for specific diagnosis of infection caused by group A beta-hemolytic streptococcus.
- Immunoserological tests (determination of titers, anti-DNase B, antistreptokinase.
- ECG.
Differential diagnosis
In differential diagnosis, you need to keep in mind that some local and general signs characteristic of chronic tonsillitis can be caused by other foci of infection, for example pharyngitis, gum inflammation, dental caries. With these diseases, inflammation of the palatine arches and regional lymphadenitis can also be observed.
It is also necessary to carry out a differential diagnosis between chronic tonsillitis and non-inflammatory hypertrophy of the palatine tonsils. The size of the tonsils itself does not indicate chronic tonsillitis. In children, the presence of enlarged NM indicates only rapidly occurring processes of the formation of natural immunity. In rare cases, nonspecific chronic tonsillitis requires differential diagnosis with specific processes (tuberculosis, syphilis, etc.). With pronounced (especially unilateral) hypertrophy of the palatine tonsils, we must not forget about the likelihood of oncological and lymphoproliferative diseases (cancer, lymphosarcoma).
Differential diagnostic signs of chronic tonsillitis and chronic pharyngitis are given in table. 2.
TREATMENT
Non-drug treatment
The widespread prevalence and significant impact of tonsillar pathology on many human organs and systems determine the relevance of the problem of chronic tonsillitis. Considering the extremely important role of the palatine tonsils in the processes of immunogenesis, indications for tonsillectomy must be strictly defined. In the absence of absolute indications for tonsil removal, conservative treatment that preserves the immunological functions of the tonsil lymphoid tissue seems most appropriate.
Treatment must begin with sanitation of the mouth, nose and paranasal sinuses, pharynx, etc.
Surgery
Surgical treatment (tonsillectomy) is carried out in case of ineffectiveness of conservative therapy and in case of chronic tonsillitis, toxic-allergic form of the II degree.
With regard to indications for tonsillectomy, all patients can be divided into three groups:
The first, largest group includes patients who periodically experience exacerbations of the disease in the form of ATF, peritonsillar abscesses, which deprive them of their ability to work and gradually worsen their general condition.
The second group consists of patients with various diseases otologically and pathogenetically associated with chronic tonsillitis and its periodic complications. These are toisillogenic rhinitis, sinusitis, conjunctivitis, dacryocystitis, cervical lymphadenitis, pharyngitis, laryngitis, tracheobronchitis, gastroenteritis, appendicitis, colitis, etc.
The third group includes patients with metatonsillar complications that occur “at a distance”, caused by the presence of an infectious-allergic focus of infection in the palatine tonsils (infectious polyarthritis, cardiovascular and renal complications, damage to the nervous system, etc.).
If indicated, there is no alternative to tonsillectomy. In some cases, patients may undergo organ-preserving operations - if conservative treatment is ineffective, with a compensated form of chronic tonsillitis, with contraindications to tonsillectomy, with a decompensated form of chronic tonsillitis, and as a trial treatment for relative indications for tonsillectomy.
Drug treatment
Therapy for chronic tonsillitis, as a rule, includes a whole range of local and systemic therapeutic effects. An effective way is to wash the lacunae of the palatine tonsils (with a syringe, using hardware) with solutions of antimicrobial agents, treatment using the Tonsilor device, and physiotherapy. If the results are effective, courses of conservative therapy are carried out 1–3 times a year.
In addition, immunostimulating agents are used - bacterial lysates (for example, Imudon, lozenges). The use of local immunomodulators promotes faster relief of symptoms.
The inclusion of the drug Imudon® in the treatment regimen in patients with chronic tonsillitis is also characterized by restoration of the function of phagocytosis (decrease in indicators of incomplete phagocytosis) and a tendency to normalize antibody formation. Phagocytosis in the pathogenesis of infectious and infectious-allergic diseases is one of the key links in immune reactions that determine the outcome of diseases - recovery or chronicity.
According to indications, adaptogens, antioxidants, herbal remedies, immunotropic therapy, and homeopathic remedies are used.
The use of immunotropic therapy makes it possible to increase the effectiveness of complex treatment of patients with chronic tonsillitis. Among the wide variety of immunomodulators, one can highlight the drug Galavit (Selvim LLC, Russia), which has a multidisciplinary mechanism of action: immunomodulatory, anti-inflammatory, antioxidant, regenerative. The mechanism of the immunomodulatory action of Galavit is associated with the ability to selectively regulate (increasing or decreasing depending on the initial values) the functional and metabolic activity of innate and adaptive immune cells (monocytes, macrophages, neutrophils, natural killer cells, etc.). By enhancing the phagocytic activity of monocytes and macrophages, the bactericidal activity of neutrophils and the cytotoxic activity of NK cells in case of its initial deficiency, the drug increases the body’s nonspecific resistance to infectious diseases of bacterial, viral and fungal etiology, promotes faster elimination of the pathogen from the body, reduces the frequency, severity and duration infections. In addition, Galavit stimulates the production of endogenous interferons (IFN-α, IFN-γ) by producer cells; normalizes antibody formation, increases the functional activity of antibodies. Anti-inflammatory effect: realized by reversible (6-8 hours) inhibition of the production of pro-inflammatory cytokines (IL-1, IL-6, TNF-α) by hyperactivated monocytes/macrophages, reducing the severity and duration of the intoxication-inflammatory process. The antioxidant effect is realized through direct inactivation of a number of radical compounds, blocking the production of reactive oxygen species by hyperactivated macrophages, regulating the activity of antioxidant enzyme systems, thereby reducing the level of oxidative stress and protecting tissues and organs from the destructive effects of radicals. The drug helps to increase the production of growth factors by monocytes/macrophages at the site of inflammation and thus accelerate regeneration processes.
The results of clinical studies have confirmed the effectiveness of complex treatment of chronic tonsillitis with the inclusion of the immunomodulator Galavit in terms of increasing the efficiency of eliminating the infectious agent from the body, reducing the frequency of relapses, and increasing the duration of clinical remission.
Concomitant therapy
To increase the effectiveness of therapy, accelerate recovery and prevent exacerbations of chronic tonsillitis, the use of the immunomodulatory drug Anaferon/Anaferon for children is recommended. The drug stimulates the humoral and cellular immune response, increases the production of antibodies (including secretory IgA), the functional activity of phagocytes and natural killer cells (NK cells). When treating chemotherapy, Anaferon/Anaferon for children is prescribed as part of complex therapy in a dosage of 1 tablet once a day.
Evaluation of treatment effectiveness
The criteria for the effectiveness of treatment of chronic tonsillitis are: reducing the number of exacerbations, preventing the development of complications and associated diseases.
Complications and side effects of treatment
Complications and side effects of treatment correspond to the adverse side effects of drugs and treatment methods used to treat chronic tonsillitis.
FORECAST
With timely and adequate treatment, the prognosis is favorable. Without treatment, there is a high risk of developing systemic infectious and allergic diseases. It should be noted that pharmacotherapy for chronic tonsillitis TAF degrees I and II cannot guarantee relief from tonsillogenic intoxication and the development of systemic infectious-allergic complications, because the persistence of pathogenic microflora in the tonsils is not eliminated.
Why is tonsillitis dangerous?
Chronic tonsillitis is very dangerous: if you do not consult a specialist in a timely manner and self-medicate, complications may develop, among which the most dangerous are diseases of the heart and blood vessels, and rheumatic joint damage.
Tonsillitis in adults often leads to damage to the kidneys ( tonsillorenal syndrome ) and heart ( tonsillocardiac syndrome ). This is due to the fact that infectious and toxic factors that damage internal organs enter the body from the palatine tonsils. Streptococcus, for example, secretes a toxin, the effects of which can cause myocardial dystrophy and heart disease or rheumatism . In addition, purulent contents entering the gastrointestinal tract from the lacunae of the tonsils can provoke dysbacteriosis.
Pus plugs in the throat
The appearance of bad breath, difficulty swallowing, headache and a sore throat indicate the presence of purulent plugs. In addition, patients develop a high temperature, corresponding to the severity of the inflammatory process. Take a close look at the oral cavity: if in the mirror you see whitish neoplasms of a multiple or single nature located on the surface of the tonsils, then these are purulent plugs that need to be removed and the sore throat treated under the supervision of an otolaryngologist.
Causes
Congestion in the throat accompanies a sore throat that has not been completely cured and has become protracted. The appearance of traffic jams is characteristic of the acute period, as well as the manifestation of the chronic form of the disease. Tonsillitis occurs in both children and adults, and almost always it characterizes a worsening of the pathology. Externally, the corks vary in size - there are whitish dots that look like semolina, or corks with a diameter of about one centimeter. They are visible to the naked eye.
The appearance of plugs is possible only on the palatine tonsils, since they have lacunae - special depressions that are obstructed by purulent discharge. The only way to get rid of traffic jams is to remove your tonsils. However, medical doctors also approach this issue selectively. They carefully study each clinical case and suggest removing the tonsils if the disease cannot be cured conservatively. You should not delay your visit - it is more effective to treat any pathology at an early stage, so as not to resort to radical methods.
Factors in the appearance of purulent plugs
It is necessary to distinguish not only the reasons why plugs appear, but also those factors that provoke an exacerbation of chronic tonsillitis and the resumption of purulent plaque in the lacunae. This process is not always associated with hypothermia and the penetration of pathogenic microorganisms. Traffic jams may occur due to:
- lifestyle - poor oral hygiene, incorrect or incomplete treatment of the disease, bad habits, smoking;
- chronic diseases of the nasal sinuses, which provoke an additional source of infection, and because of this, local immunity is reduced, existing pathologies are aggravated, including tonsillitis;
- a sharp decrease in immunity as a result of a previous serious illness, surgery, chemotherapy, stress or hypothermia;
- food addictions, poor diet - for example, eating large amounts of protein foods helps maintain the inflammatory process;
- injuring the tonsils, for example, when removing plugs on your own, which is strictly prohibited, because the slightest cracks or wounds contribute to the penetration of infection into the blood.
Complications
Despite the fact that angina is a common diagnosis and is traditionally considered a “childhood disease,” it carries serious consequences for the body that can affect much later. Complications are especially severe when a sore throat is not completely cured, when the pathology becomes chronic, and the inflammatory process is sluggish, with seasonal exacerbations.
Among the complications are:
- peritonsillar abscess - inflammation of not only the tonsils, but also the tissues around them, while the fiber is involved so quickly that this leads to an exacerbation of the pathology, a sharp rise in temperature and a deterioration in the patient’s condition;
- phlegmon - an exacerbation of the pathological process, which is associated with the involvement of the subcutaneous tissue of the neck, and in the absence of timely assistance, death can occur;
- degeneration of tissue and replacement of lymphatic tissue with connective tissue, which represents scars and cannot perform its previous protective functions;
- sepsis - blood poisoning when pathogenic microorganisms enter the bloodstream, which quickly spread throughout the body and provoke suppuration of other organs and tissues, and the body’s defenses do not have time to cope with the spread of infection;
- kidney damage is also a complication associated with infection, since the kidneys filter the blood and accumulate not only a lot of pathogens, but also decay products and toxins, which significantly affects the production of urine and filtering of the blood;
- inflammation of the joints and heart - often these are delayed complications that do not appear immediately, as the body tries to fight the infection, turns on protective and compensatory forces, but after some time such consequences still make themselves felt.
Self-cleaning of traffic jams
Doctors insist that purulent plugs on the tonsils cannot be removed on their own, because this must be done according to a certain method, and the patients themselves often neglect basic safety rules. This can only worsen the course of the pathology - lead to extensive bleeding when tissue is damaged or the spread of the pathological process deep into the tonsils and onto healthy tissue. Self-medication for sore throat is extremely undesirable.
A relatively safe way is to cleanse the tonsils with the tongue. It is necessary to slightly press the tongue on the plugs, and they can easily come out, after which the throat is gargled to remove the purulent discharge. The tongue does not injure the mucous membrane as much and is not able to push the plugs inside, damaging the delicate tissue of the lacunae. Doctors also do not recommend using cotton swabs or pads to remove accumulated deposits. This is dangerous primarily due to damage. It is best to do the procedure in an office under the supervision of a medical specialist.
However, if you can’t visit a doctor, and the traffic jams have formed quite large and quickly, then two hours after eating you can gargle with an antiseptic and try to remove them with a gauze swab. To do this, soak the tampon in the antiseptic solution and, without applying pressure, try to gently move the plug up. Do not press on it under any circumstances, or point the tampon towards your throat, so as not to swallow the plug. Rinse your mouth every time the discharge is successful. Watch for pain or excessive bleeding. If after two or three attempts the plug does not come out, you should not continue the procedure.
Treatment
Therapy consists primarily of removing purulent discharge and inhibiting the inflammatory process in the tonsils, followed by powerful prevention and restoration of the body's defenses. Treatment begins with washing the tonsils.
Washing
Deposits are removed using a syringe or vacuum method - it depends on the patient’s health condition. If the doctor uses a syringe, then rinsing occurs under the pressure of the liquid with which it is filled. This is usually an antiseptic drug. Using a curved cannula, you can wash out purulent plugs even from hard-to-reach places. Since all the gaps are interconnected by passages, it is enough to act on two or three of the largest of them to wash out all the passages. The procedure is carried out every other day, and the course of treatment takes up to 15 procedures.
Vacuum rinsing is performed under anesthesia. A special device with a nozzle is fixed on the tonsil, which, when creating negative pressure, removes pus from the lacunae. After cleaning with a vacuum, they are washed with an antiseptic. Treatment also requires 10-15 procedures.
Physiotherapy
To assist with the main therapy, doctors also include physiotherapeutic procedures in the treatment regimen, which are aimed at reducing the inflammatory process and speedy regeneration of tonsil tissue. Physiotherapy is prescribed only in those moments when the pathology is not in an acute stage. Treatment methods include:
- ultraviolet irradiation;
- laser irradiation;
- ultrasonic aerosols.
The number of procedures, prescription of drugs and duration of sessions are strictly regulated by the doctor. It depends on the severity of the disease and the extent of tissue damage.
Laser treatment
The procedure does not require anesthesia and causes only minor discomfort. The laser burns out pathologically altered tissues, and the scars tightly close the lacunae, preventing further accumulation of purulent discharge. In most cases, one session is enough, but for advanced disease with frequent relapses, three sessions are required. You may experience a sore throat for some time after laser treatment.
Treatment of purulent plugs in medical settings is carried out conservatively, and only if it is impossible to help patients in other ways, doctors resort to removing the tonsils.
Prevention
Prevention of purulent plugs should primarily consist of proper treatment of sore throat and prevention of its recurrence, manifestation of the disease during a latent course. Proper prevention will help prevent exacerbation and get rid of purulent plugs. To do this you need the following:
- thorough oral hygiene, proper cleaning, elimination of carious lesions;
- rinsing your mouth after eating;
- drinking enough water;
- to give up smoking;
- proper and varied nutrition;
- refusal of alcoholic beverages;
- complete treatment of pathologies of the throat and nose.
Remember that tonsillitis requires long-term treatment, the use of antibiotics, and physiotherapeutic measures. Therefore, all doctor’s recommendations must be followed in full so that plugs on the tonsils do not appear later.
Author
Yampolsky Sergey Zigfridovich
otorhinolaryngologist (ENT)
Candidate of Medical Sciences
40 years of experience
+7
Prerequisites for the development of tonsillitis
The palatine tonsils, nasopharyngeal tonsil, lingual and tubal tonsils form a protective ring (lymphoepithelial ring of Pirogov) - a powerful barrier to the air and food entering the body. The tonsils do a great job - they recognize dangerous viruses and bacteria in the air and food and trigger an immune reaction.
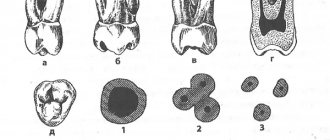
When examining the tonsil on its surface, you can see depressions and openings with narrow, winding and deep passages (the so-called tonsil lacunae).
| 1 - crypt (lacuna); 2 - lymphoid follicles; 3 - connective tissue capsule; 4 - mouth of the lacuna (crypt). | |
The existence of deep lacunae creates the prerequisites for the development of chronic inflammation of the tonsils. Remains of food, dead immune cells, etc. settle in the gaps, which are an excellent breeding ground for the proliferation of pathogenic microorganisms.
Classification of tonsillitis
The disease can be acute or chronic. In the first case, signs of infection disappear within 7 to 10 days. In a chronic course, pathogens remain in the tissues of the tonsils, causing periodic exacerbations. Treatment of chronic tonsillitis is a complex task that only experienced otolaryngologists can handle.
Chronic tonsillitis has 2 forms - simple and toxic-allergic. In the latter case, there are 2 degrees of severity of pathological changes.
The simple form is characterized by only local symptoms. With the toxic-allergic variant, the following pathological processes occur:
- microbial toxins that enter the blood cause sensitization (altered reactivity) of the body;
- they act directly on the tissues of internal organs;
- toxins also lead to the development of allergic and autoimmune reactions.
To treat tonsillitis in this case, a complex effect on the entire body is necessary.
Symptoms of tonsillitis
There are simple and toxic-allergic forms of tonsillitis. The simple form is characterized by only slight chronic inflammation of the tonsils, without a pronounced general reaction of the body.
In the toxic-allergic form, there are not only local signs of chronic inflammation, but sore throats, paratonsillitis, paratonsillar abscesses, as well as disorders in other systems (cardiovascular, genitourinary, etc.) develop.
General manifestations:
- fast fatiguability;
- lethargy;
- headache;
- elevated body temperature.
Local manifestations:
- discomfort in the throat when swallowing;
- sore throat;
- putrid odor from the mouth;
- formation of purulent-caseous “plugs” in the lacunae of the tonsils;
- dry cough;
- frequent sore throats;
- enlarged and painful regional lymph nodes.
Chronic form of tonsillitis, why the tonsils become inflamed
Infection is the main cause of inflammation of the tonsils. The acute form of the disease in 70% of cases is caused by viruses, the remaining 30% is caused by bacterial and fungal flora. Therefore, sore throats most often accompany acute respiratory infections and are seasonal.
Damage to the tonsils in chronic tonsillitis in 80% of cases is of a bacterial nature. The main causative agents of the disease:
- β-hemolytic streptococcus.
- Group A streptococcus.
- Staphylococcus aureus.
- Haemophilus influenzae.
- Rarely encountered bacteria: mycoplasma, chlamydia, etc.
Viruses in the chronic form of the disease have a predominantly provocative, destabilizing effect. Acute and chronic recurrent viral infections weaken the immune defense, which creates conditions for the activation of bacterial flora. Hypothermia, acute intoxication, and ingestion of cold or irritating food lead to the same result.
Diagnostics
Diagnosis of tonsillitis in children, as well as tonsillitis in adults, is carried out using the following methods:
- examination by an ENT doctor, collecting an anamnesis of the disease;
- throat swab for flora with determination of sensitivity to antibiotics and bacteriophages;
- general blood test, general urinalysis;
- blood test for antistreptolysin-O, rheumatoid factor, C-reactive protein;
- ECG;
- According to indications, ultrasound of the kidneys, Echo-CG, consultation with a cardiologist, urologist.
Angina
CAUSES OF SOLISH
The cause of sore throat is pathogenic bacteria, usually streptococci, which are present in the pharynx in a conditionally pathogenic state and usually do not cause disease, but under unfavorable conditions (hypothermia in autumn-winter and spring, temperature changes) are activated and become pathogenic , as a result, an inflammatory process develops.
THE FOLLOWING MOMENTS CONTRIBUTE TO THE ACTIVATION OF SOLISH CAUSES ON THE MUCOSA:
- Past influenza or other acute respiratory infections;
- Predisposition of the body to sore throat;
- The presence of a purulent inflammatory process in the nasal cavity, paranasal sinuses, oral cavity or pharynx (rotten teeth affected by caries).
CLASSIFICATION OF ENGINES (PHARINGOSCOPIC SIGNS ACCORDING TO B.S. PREOBRAZHENSKY):
- Catarrhal tonsillitis (there is hyperemia of the palatine tonsils, the edges of the arches and the soft palate; the tongue is coated, dry);
- Follicular tonsillitis (inflammation occurs in the area of lymphadenoid follicles with their suppuration and subsequent opening);
- Lacunar tonsillitis (appearance of exudate or plaque at the mouths of lacunae);
- Fibrinous tonsillitis (plaques take on a fibrinoid character and completely cover the tonsil);
- Herpetic sore throat is characterized by herpetic rashes on the tonsils, soft palate and arches;
- Phlegmonous tonsillitis develops when pyogenic bacteria penetrate into the tissue behind the tonsil with the formation of an abscess, both in the tonsil itself and behind it;
- Mixed forms.
To select the correct treatment tactics, an otolaryngologist needs a routine examination, but in some cases laboratory tests are required.
DIAGNOSIS OF SOLISH. METHODS.
- Clinical examination. Includes a survey and examination of the patient with palpation of the lymph nodes, examination of the oropharynx and tonsils, and listening to the lungs. Based on the data obtained, a preliminary diagnosis is made.
- Pharyngoscopy (examination of the oropharynx using a spatula under artificial bright light.
- Bacteriological analysis.
- Nasal cavity test.
- General blood analysis.
When a sore throat becomes chronic or severe, complications are diagnosed:
- Laboratory blood test.
- Echocardiogram.
- Radiography.
CLINIC OF SOLISH
Sore throat, as a rule, begins acutely.
SYMPTOMS OF SOLISH
- General symptoms: weakness, malaise, “heavy” head, increased body temperature to 39-40°C, chills, a feeling of weakness in the body with joint pain and pain in the muscles of the extremities;
- Dryness, rawness, soreness, burning in the throat and pharynx;
- A feeling of narrowing, tightness, squeezing in the throat, making breathing difficult;
- Hoarseness;
- Pain when swallowing (may radiate to the ear, temple);
- Redness of the tonsils, with severe damage, the appearance of purulent plaque on them.
COMPLICATIONS OF SOLISH
With incorrect diagnosis and inadequate treatment of angina, serious complications are possible, such as peritonsillar abscess, retropharyngeal abscess, neck phlegmon, postanginal sepsis (Lemierre's syndrome), streptococcal meningitis, acute rheumatic fever, glomerulonephritis, pyelonephritis, polyarthritis, etc.
TREATMENT OF SOLISH AT THE CLINIC ENT CENTER
Mainly local and systemic antibacterial therapy, anti-inflammatory therapy are carried out, in severe cases - steroid, detoxification therapy, etc.
A frivolous attitude towards sore throat is unacceptable, especially independent treatment. Treatment must be carried out under the supervision of an otolaryngologist. Only timely and correct comprehensive treatment of sore throat will protect the patient from serious complications.
PREVENTION OF SOLISH
- Indoor air humidification. The humidity of the air in which a person is located must be at least 45%, otherwise the mucous membranes dry out and become susceptible to inflammation.
- To give up smoking. Cigarette smoke impairs blood circulation in the mucous membranes and destroys the protective mechanisms of the upper respiratory tract.
- Breathing is not through the mouth (with cooling and drying of the mucous membrane of the oropharynx), but through the nose. The nasal mucosa absorbs many foreign bodies before they enter the throat, warms and humidifies the air.
- Maintaining a gentle voice regime.
- Hardening the body.
Treatment of chronic tonsillitis
Many people wonder: how to treat tonsillitis and is it really necessary to remove tonsils? The therapeutic tactics on which the treatment of tonsils depends depends on the form of the disease, the degree of dysfunction of the palatine tonsils and the presence of diseases associated with chronic tonsillitis.
Conservative treatment of tonsils
Conservative therapy consists of the following measures:
- sanitation of the upper respiratory tract (removal of adenoids, hypertrophic rhinitis, deviated nasal septum, sinusitis) and oral cavity (treatment of caries, gingivitis, etc.);
- prescription of means that help increase the body's defenses: (hardening procedures, daily routine, balanced nutrition, vitamin therapy, physical activity, spa treatment);
- prescription of hyposensitizing drugs;
- prescription of immunocorrectors;
- the use of reflex effects: acupuncture, manual therapy of the cervical spine;
- washing the tonsils with antiseptic solutions to remove the pathological contents of the tonsils (plugs in the tonsils, purulent masses);
- treatment with the “Tonsilor” device;
- introduction of medicinal substances into the lacunae (various emulsions, pastes, ointments, oil suspensions are introduced using a syringe with a cannula);
- lubrication of the tonsils (with solutions of protargol, collargol, oil solution of chlorophyllipt, Lugol, etc.);
- gargling with antiseptic solutions (performed independently by the patient);
- use of physiotherapeutic treatment methods.
1 Sanitation of the upper respiratory tract in MedicCity
2 Acupuncture of the cervical spine in MedicCity
3 Manual therapy of the cervical spine in MedicCity
Very effective in the complex treatment of tonsillitis is washing the lacunae of the palatine tonsils using vacuum aspiration. A similar device is equipped with a specialized ENT unit in the MedikCity otolaryngologist’s office. The essence of the procedure is mechanical cleansing with the help of a special nozzle under the influence of vacuum from the lacunae of the tonsils from caseous plugs and purulent discharge and subsequent treatment of the tonsils with an antiseptic. This procedure is not performed during periods of exacerbation of sore throat and other infectious diseases of the respiratory tract, as well as during acute toothache. Carrying out courses of 5-10 procedures twice a year allows patients to forget about relapses. If there is no effect after 2-3 courses, the issue should be resolved radically (tonsil removal).
Conservative treatment is carried out in courses and includes a combination of the methods listed above, which are selected individually.
Usually, to fully consolidate the result, 2-3 courses of treatment of 10 sessions each with an interval of 6-12 months are sufficient.
Chronic tonsillitis and related diseases
A. Yu. Ovchinnikov, A. N. Slavsky, I. S. Fetisov
Department of Otorhinolaryngology MMA named after. I. M. Sechenova
Currently, about 100 different diseases are known, largely due to chronic tonsillitis. The lack of a therapeutic effect or short-term remission in such diseases is often due to the fact that doctors do not take into account the pathology of the pharynx as a possible cause that provokes and maintains associated painful conditions in other organs and systems of the body.
The purpose of this publication is to draw the attention of practitioners to a fairly large number of diseases that develop against the background of pharyngeal pathology, but are often not considered in the context of this relationship. The changes in internal organs are most pronounced in the decompensated form of chronic tonsillitis. They are caused by the influence of neuro-reflex, bacteremic, toxicemic and allergic factors.
An imbalance in the immune status is also determined - redistribution in the content of T- and B-lymphocytes and their subpopulations, the presence of circulating immune complexes, sensitization of granulocytes to bacterial allergens.
Circulating antigen-antibody immune complexes have chemotoxic activity and increase the proteolytic ability of macrophage enzymes, which leads to lysis of tonsil tissue and denaturation of tissue proteins, which as a result acquire antigenic properties. Once in the blood, they cause the formation of autoantibodies. Thus, the palatine tonsils become a site of permanent delayed-type sensitization to the antigens of streptococcus and staphylococcus - microflora that most often grows in the lacunae of the palatine tonsils.
The neuro-reflex mechanism of the influence of chronic tonsillitis on the formation of associated pathology is also described. A.M. Monaenkov was the first to discover and study the afferent connections of the palatine tonsils with the most important subcortical formations, in particular with the co-structures of the posterior section of the subtubercular region of the hypothalamus. It is these nerve structures that are involved in the regulation of natural active immunity, which determines the central determination of disturbances in immunological reactivity in chronic tonsillitis.
It has been established that under the influence of the flow of afferent signals from the tonsillar region, the functional state of the nuclei of the subthalamic region is disrupted and adrenergic receptors of neurons are excited. This serves as a trigger for the development of disruption of autonomic synergism and subsequent chain disorganization of other nervous structures. Such disturbances of neurodynamic processes in certain subcortical and cortical parts of the brain are called a “tonsillogenic” neurodystrophic process and are assessed as an obligatory component in the pathogenesis of any metatonsillar lesions.
It is also possible to have a toxic effect on the body during chronic inflammation of the tonsils due to the dissemination of toxins by the hematogenous or lymphogenous route.
It is now known that, along with the well-studied and thoroughly described influence of chronic tonsillitis on the formation of pathology of the heart, joints and kidneys, there are a large number of other associated painful manifestations. Thus, chronic tonsillitis creates real preconditions for the development of dermatoses. This, in particular, is confirmed by the rather high frequency of detection of chronic tonsillitis in patients with psoriasis and the presence in them of a clear relationship between the activity of the clinical course of this disease and the exacerbation of chronic tonsillitis. Many researchers consider tonsillectomy one of the most important components of treatment for patients with psoriasis. Sanitation of the focus of chronic infection normalizes altered reactivity and reduces allergenicity of the body, eliminates the pathological reflex effect on the central nervous system. It is advisable to perform tonsillectomy in the earliest stages of development of dermatosis. Conservative treatment should not be abandoned, since isolated cases of exacerbation of psoriasis after tonsillectomy have been described. A positive result is manifested in stable remission or mitigation of the clinical picture of exacerbations.
Neurodermatitis is often combined with chronic tonsillitis, which in this case quickly becomes widespread with frequent relapses complicated by pyoderma.
Treatment of neurodermatitis without sanitation of the source of chronic infection is ineffective.
Chronic tonsillitis plays a role in the occurrence and course of collagen diseases (systemic lupus erythematosus, scleroderma, hemorrhagic vasculitis, periarthritis nodosa, dermatomyositis, polyarthritis). A similar antigenic structure of some collagenoses and chronic tonsillitis has been proven; for example, hemorrhagic vasculitis and chronic tonsillitis have common antigens - B 27, Cw2, Cw6.
Chronic tonsillitis can lead to eye diseases.
Thus, tonsillogenic intoxication can significantly weaken the accommodative apparatus of the eye. Therefore, an important measure to prevent myopia is early sanitation of the source of chronic infection. Behcet's disease, which causes eye lesions, is also provoked by a focus of chronic streptococcal infection during tonsillitis.
A combination of nonspecific lung diseases and pathology of the palatine tonsils is often noted. Thus, endogenous peribronchitis is provoked by inflammatory processes of the nose, paranasal sinuses and lymphoid pharyngeal ring. Sometimes chronic tonsillitis can contribute to the exacerbation of chronic pneumonia, and also lead to a more severe course of this disease. Pulmonologists note that timely sanitation of a focal infection in the palatine tonsils reduces the number of complications in chronic lung diseases by 2.3 times.
The infectious-toxic mechanism of liver damage in chronic tonsillitis is described. The streptococcal toxin streptolysin O is capable of disrupting the process of oxidative phosphorylation in hepatocyte mitochondria. As a result, existing liver diseases worsen. Thus, with viral hepatitis A, severe and protracted forms are more often observed, and with viral hepatitis B there is a tendency for the process to become chronic. There are known cases of development of damage to the biliary system in chronic tonsillitis.
Cerebral complications in chronic tonsillitis arise as a result of vascular-circulatory disorders and toxic effects from the source of inflammation. The course of cerebrovascular disorders and toxic-infectious encephalopathy occurs in the form of a chronic process or crises. In this case, there are several forms of hypothalamic syndrome. The most common form is the vegetative-vascular form, then the neuroendocrine-metabolic form, and the least common is the neurotrophic form.
A constant and early symptom is cerebral vascular insufficiency due to damage to the cardiovascular system. Hypothalamic angioedema is manifested by a persistent decrease in peripheral blood pressure and signs of peripheral angioneurosis (Raynaud's syndrome). Possible manifestation of cerebral angioedema in the form of migraine or Meniere's syndrome. These paroxysms are superimposed on chronic cerebrovascular insufficiency and are clinically manifested by neurotic conditions. Such “neurasthenia” is accompanied by general weakness and increased fatigue during mental and physical stress. With functional insufficiency of the hypothalamus, patients become sensitive to adverse meteorological factors.
Sometimes neuro-endocrine disorders occur: obesity or weight loss, loss of appetite, thirst, hyperhidrosis, menstrual irregularities, decreased sexual potency. Due to damage to the nuclear stem structures, paroxysms of loss of skeletal muscle tone appear. Smooth muscle tone also decreases. Stem disorders are a consequence of chronic circulatory insufficiency, toxic-infectious and autoallergic processes that occur during chronic tonsillitis. Hypoxia of the respiratory center is manifested by irresistible yawning at the slightest mental or physical fatigue.
It has been proven that women suffer from such disorders more often, since their hypothalamus is subjected to greater physiological stress.
Chronic tonsillitis aggravates the course of schizophrenia. As a result of autointoxication, the disease becomes progradient or malignant.
In the early stages of development of chronic tonsillitis, there is a compensatory increase in the level of androgens and glucocorticoids. As the disease develops, there is a gradual depletion of the function of the adrenal cortex with all the ensuing consequences for the body.
Focal infection in the palatine tonsils can lead to weakening of the islet tissue of the pancreas and the release of a proteolytic enzyme that destroys endogenous and exogenous insulin. As a result, chronic tonsillitis can contribute to the decompensation of carbohydrate metabolism disorders already existing in the body, leading to an increase in hyperglycemia and glycosuria. In turn, metabolic disorders in diabetes form favorable conditions for exacerbations of chronic tonsillitis. Sanitation of the pharyngeal source of infection improves carbohydrate metabolism, which confirms the pathogenetic relationship of these diseases. Some researchers believe that conservative treatment of tonsillitis with this combination is ineffective and a tonsillectomy is necessary after a year. Follow-up data indicate that in patients with diabetes mellitus, surgery contributes to stable compensation, and in some cases allows to reduce the dose of insulin.
With chronic tonsillitis, the thyroid gland suffers. Most often, there is an increase in hormone-forming function.
This disorder is associated with hyperstimulation of the thyroid gland by thyroid-stimulating hormone from the pituitary gland. The consequence of this will be an increase in the concentration of thyroxine in the blood. This process is explained by the effect of pathologically altered palatine tonsils on the hypothalamic-pituitary system. Another possible mechanism for damage to the thyroid gland is associated with disorders of the immune system. Thus, in individuals with a genetically determined predisposition to autoimmune thyroid diseases, diseases such as autoimmune Hashimoto's thyroiditis, subacute de Quervain's thyroiditis, Riedel's fibrous thyroiditis, and acute thyroiditis may occur. It has been noted that the severity of pathological changes in the thyroid gland depends on the duration of chronic tonsillitis and the frequency of its exacerbations. As a result of successful treatment of the pathology of the palatine tonsils, one can observe an improvement in the condition of the thyroid gland and normalization of its hormonal synthetic function.
There is evidence of a high incidence of chronic tonsillitis in obesity, which may be due to damage to the ventromedial and ventrolateral nuclei of the hypothalamus. In the decompensated form of chronic tonsillitis in combination with obesity, there are significant disturbances in the hormonal status (decrease in the level of testosterone and follicle-stimulating hormone and increase in luteonizing hormone). Children with such disorders have clinical signs of delayed sexual development (adiposogenital dystrophy). Chronic tonsillitis aggravates changes in the hypothalamic-pituitary regulation of the testes and delays the onset of puberty.
Modern studies have proven the pathogenetic role of tonsil apudocytes in the development of immunodeficiency states.
In chronic tonsillitis, a threefold increase in cells of the APUD system is recorded, cells producing serotonin and somatostatin appear, and the number of mast cells increases. Such changes may also be one of the reasons for the development of pathological changes in other organs.
It has been proven that chronic tonsillitis has an adverse effect on the formation of the reproductive system in girls.
Exacerbation of chronic tonsillitis and the transition of its compensated to decompensated form are more often observed at the age of 8-10 years (adrenarche period) and 12-14 years (menarche period), i.e. during activation of the endocrine function of the pituitary-adrenal system (adrenarche) and the entire reproductive system (menarche).
Our studies have shown the presence of a direct relationship between chronic tonsillitis, especially its decompensated form, and disorders in the reproductive system in women of fertile age. These changes are characterized by disruption of the production of hormones such as follicle-stimulating, luteinizing, luteotropic, somatotropic, adrenocorticotropic and thyroid-stimulating, the appearance of uterine bleeding, hypomenstrual syndrome and amenorrhea of central origin. Such disorders in patients with chronic tonsillitis can be considered a manifestation of hypothalamic-tonsillar syndrome. Damage to the hypothalamic region is indicated by characteristic changes in the electroencephalogram. Changes in hormonal levels can provoke diseases such as endometriosis, adenomatosis and uterine fibroids.
With chronic tonsillitis, the development of pregnancy pathology is often observed, since it contributes to a significant decrease in the body's adaptive capabilities and is a predisposing factor for the formation of toxicosis. There is often a threat of early or late miscarriage or premature birth. Deviations of labor may develop, such as premature rupture of amniotic fluid, weakness of labor.
Often chronic tonsillitis leads to hypogalactia due to hypothalamic-pituitary disorders.
We believe that patients with combined pathology of the tonsils and reproductive system should be under constant medical supervision by an otolaryngologist and gynecologist.
There is a tendency to normalize hormonal synthetic function and clinical signs of reproductive disorders as a result of successful treatment of chronic tonsillitis.
Most patients with a decompensated form of chronic tonsillitis have abnormalities in the morphogram (intersex physique). A characteristic set of symptoms is disproportionate, inharmonious, asynchronous development. False acceleration syndrome often occurs, which can be considered a variant of sexual infantilism.
All of the above allows us to conclude that patients with chronic tonsillitis form a large risk group for many severe somatic disorders and require increased attention from both an otolaryngologist and doctors of other specialties. Only such an integrated approach can reduce the number of complications in patients with chronic tonsillitis.
Published with permission from the administration of the Russian Medical Journal.
Treatment of tonsillitis
The form of tonsillitis and the current stage of the disease directly affect the tactics of treating tonsillitis. Treatment will be based on an integrated approach aimed at relieving acute symptoms of the disease and eliminating the previously identified pathogen:
- Antiseptic solutions for gargling.
- Pain relievers in the form of tablets, sprays or lozenges.
- Solutions for washing tonsils. If there is an accumulation of purulent contents, the plaque should be removed using a special syringe.
- Use of local immunomodulators.
- Taking antipyretics if necessary.
- Antibiotics. During treatment, it is very important to follow the regimen and not stop taking the medications, even if you feel better. The disease can be treated and bacteria can be completely eliminated only by completing the full course prescribed by the doctor. Complete treatment is necessary not only to relieve symptoms, but also to suppress the pathogen.
Physiotherapeutic treatment can help improve your well-being and eliminate the characteristic signs of the disease. The procedures help normalize blood circulation and stimulate the production of antibodies to tonsillitis. The patient is offered to treat the disease using ultraviolet light therapy or UHF. To wash the tonsils, the attending physician may prescribe vacuum hydrotherapy.
During treatment, it is very important to provide the patient with gentle nutrition: boiled or steamed foods will not further injure the throat. Drinking plenty of fluids will also promote a speedy recovery from tonsillitis.
The decision regarding the removal of tonsils is made by the doctor after a full diagnostic examination and the absence of a visible effect from treatment for tonsillitis, accompanied by the development of complications (toxic-allergic form). In this case, the tonsils are removed as the source of the main threat.