Content
hide
1 Is bleeding normal?
2 Why does pathological bleeding develop?
3 Why does bleeding develop after implantation?
4 What to do if there is bleeding?
5 How to avoid bleeding after implantation?
Dental implantation is a dental procedure that is constantly evolving and is under the close attention of dentists around the world. Implants provide ample opportunities to restore aesthetics, functionality, and replace damaged dentition. After implantation, patients begin to smile again, feel free and confident. Like any surgical procedure, implantation is accompanied by some complications. One of them is bleeding. How to understand how dangerous this situation is and how to generally react to the appearance of blood from the gums?
Is bleeding normal?
Light bleeding immediately after manipulation is normal.
This is due to the invasive nature of the procedure and the peculiarities of the blood supply to the gum tissue. Before treatment, the doctor must warn you that this option is possible and you should not be afraid of the appearance of blood. On the contrary, this should give an understanding that in the first days it is necessary to carefully follow the recommendations and carry out hygiene procedures. Minor, low-intensity bleeding may bother you for several days and should not be alarmed. This situation is especially typical for those who have problems with blood clotting or fragile blood vessels. In addition to bleeding, the following symptoms will persist for several days:
- swelling of the gum tissue (but the entire cheek can also swell);
- hyperemia - redness of the gum mucosa;
- discomfort and pain in the tissues of the jaw, in the area of the installed implant.
If the healing process develops steadily, after 4–8 days the unpleasant symptoms gradually disappear. If the patient continues to experience pain, swelling increases, and the wound does not heal, it is imperative to visit the dentist.
Why is there blood flowing?
If it continues to flow a week after implantation, then this is bad in any case, but the reasons (and ways to eliminate them) may be different. Here's why it's even possible:
- the seams come apart due to the fact that the thread is damaged by a toothbrush;
- the patient has too low blood clotting, which can be caused either by illness or by taking certain medications that tend to reduce blood clotting;
- during implantation, a blood vessel was damaged - accompanying signs of this are particularly heavy bleeding and the occurrence of a hematoma;
- the patient has a history of cardiovascular diseases;
- due to hypertension or fear of surgery, the patient’s blood pressure has increased, which is why the blood cannot clot normally due to the strong pressure.
It also happens that particles of cement simply get into the thickness of the gums, which irritate the soft tissues and cause them to bleed. Excess cement must be removed; for this purpose, repeat radiography is even prescribed after the operation.
Why does pathological bleeding develop?
The appearance of blood in the first hours after dental implantation is normal. The patient sees the saliva turning pink within a few days. Aspirin or similar medications that affect clotting increase the risk of bleeding. In this case, bleeding from the wound may continue for about 10 days.
Intense bleeding from the first days and the formation of a hematoma indicates that during installation of the implant a vessel was damaged and bruising occurred. This is dangerous, since the blood mechanically displaces surrounding tissues, compresses nerve endings and is a breeding ground for microorganisms.
Complications that arise during implantation surgery
The following complications may occur during dental implantation:
- Damage to the nerves of the lower jaw. The mandibular nerve passes through the bone of the lower jaw, in a special canal. When performing surgery in the area of the chewing, lateral teeth of the lower jaw, pinching or even injury to the nerve may occur. This is manifested by loss of sensitivity, a feeling of numbness in the chin area and the corresponding side of the lower jaw.
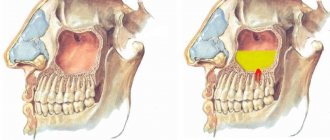
- Damage to the wall of the maxillary sinus. This complication is also associated with the structure of the bone. In the upper jaw there are special sinuses - air cavities in the bones of the skull. The maxillary sinus, the bottom of which borders the area where the roots of the lateral teeth of the upper jaw are located, is at risk of damage during dental implantation. Damage to the floor of the maxillary sinus can lead to sinusitis1, implant rejection due to inflammation, and in the most severe cases, pushing the implant into the sinus cavity.
- Bleeding. Severe bleeding during surgery can occur as a result of vascular damage or due to the patient taking blood thinning medications (such as aspirin, cardiomagnyl, warfarin). Severe bleeding can lead to the impossibility of implantation and even hospitalization of the patient.
- Overheating of tissues can occur due to the operation of the drill when preparing the cavity for installation of the implant. This can lead to severe pain in the postoperative period and impaired implant survival.
- Mobility of the implant after its installation can occur due to violations of the surgical technology, discrepancy between the size of the prepared cavity and the size of the implant, the presence of inflammatory processes in the bone, and improper preparation of the implantation area. If there is no primary fixation of the implant in the bone, its further engraftment becomes impossible.
- Fracture of the alveolar process and injury to surrounding tissue by the implant. Such complications can arise if the size of the implant is incorrectly selected and the direction of its installation is incorrectly chosen. In this case, the implant will have to be immediately removed and measures taken to repair the bone damage.
- Pain. It is extremely rare that individual characteristics of the body, the presence of inflammatory processes, and violation of the preparation regime for dental implantation (stress, poor sleep, drinking alcohol the day before surgery) can lead to a decrease in the effectiveness of local anesthesia. Naturally, if there is pain, surgery is impossible.
Why does bleeding develop after implantation?
The reasons for this complication vary. Some of them are related to the characteristics of the patient, and some do not depend on him. In the preoperative period, the doctor collects a medical history and recommends undergoing some instrumental and laboratory tests to confirm the patient’s readiness for surgery and eliminate the risk of complications.
Causes of bleeding that do not depend on the patient:
- an error that occurred during the operation, for example, the crown was incorrectly removed, arteries or nerves were damaged. Too tight implant installation, tissue irritation, infection or poor-quality sutures can also cause gums to bleed.
- Before the operation, a thorough diagnosis was not carried out, the protocol was violated and important details regarding the individual characteristics of the patient were missed.
- the patient has intolerance to materials and drugs used during surgery;
- old instruments and low quality materials can also cause gum damage.
Prevention is the best cure
A good dentist must take care to minimize possible abnormal bleeding from the patient's gums after implantation. Although not everything is within his control, he can still take the following steps:
- refer the patient in advance for an examination designed to identify possible contraindications and undesirable conditions;
- study the medical history in detail and assess possible risks;
- examine blood for clotting.
In many ways, the prevention of bleeding after implantation depends on the patient himself. It can do the following:
- as soon as the titanium pin is installed, you need to keep a piece of sterile bandage at the site of the operation, changing it hourly;
- at home, apply cold to the operated area without waiting for bleeding to begin;
- try not to load the operated area at least for the first time after implantation;
- give up solid foods and foods that require intense chewing;
- stop smoking, and ideally, quit completely, because this bad habit is one of the main causes of bleeding, and in addition can cause inflammation and suppuration, up to complete rejection of the implant by the body;
- sleep on a high pillow that keeps your head elevated;
- temporarily stop taking any medications that reduce blood clotting, such as aspirin;
- observing oral hygiene, use the brush in the area of the operation as carefully as possible, trying not to open the wound.
What to do if there is bleeding?
It is not always possible to immediately contact your doctor in case of bleeding, and there are no medical facilities nearby. Self-help in such a situation consists of the following actions:
- wrap the ice in a soft cloth and apply to your cheek for 15–20 minutes;
- You can apply a sterile gauze bandage to the gum at the point where the dental structures are installed for 15–20 minutes;
- take cool, clean water into your mouth and hold for about five minutes, then carefully spit out;
- apply a wet bag of black tea to the painful area on the gum;
- You can also place a cotton swab on the gum, which will collect excess blood and promote blood clotting.
If possible, or if home treatments are ineffective, you should seek medical help. The doctor will examine the site of inflammation and determine the causes of bleeding, which may be different and require different correction methods.
Risks when installing lower dental implants
When installing implants on the lower jaw, there is a risk of damage to the mandibular nerve.
Distortion of the vertical dimension of the mandible on an orthopantomogram (OPTG) increases the risk of incorrect determination of implant size. As a result, the walls of the mandibular canal are injured, an intracanal hematoma and nerve entrapment are formed. There is a decrease in the sensitivity of the innervation zone for 2-3 weeks until the blood masses resolve. Therefore, it is important to calculate implant sizes not using OPTG, but using three-dimensional CT.
In patients with osteoporosis, the wall of the alveolar process may be defective or completely absent. Then the nerve is compressed due to hemorrhage into the medullary space and tissue swelling. Partial loss of sensation appears the next day and lasts about a week. If paresthesia continues, the implant must be removed and therapy performed.
How to avoid bleeding after implantation?
To minimize the risk of this unpleasant complication, you should adhere to the following recommendations:
- it is necessary to reduce the mechanical impact on installed implants at the first stage after implantation.
- Upon completion of the operation, you should clamp the gauze bandage with your teeth and keep it there for an hour, and then replace it with a new one. This will help the vessels thrombose and a blood clot will form, which will stop the bleeding.
- Immediately after surgery, you can drink a little water and other drinks, but they should be cool.
- Eating after surgery is prohibited in the first two hours. After this, soft, gentle food is allowed, but not too hot or cold, but slightly warm.
- You cannot eat while the anesthesia is in effect.
- In the first days after the procedure, ice wrapped in soft tissue must be applied to the cheek on which the implantation was performed. This will relieve inflammation, normalize the diameter of blood vessels, reduce swelling and pain, and also speed up recovery.
- You must brush your teeth around the denture very carefully so as not to damage the soft tissues or cause bleeding.
- For the first ten days, it is forbidden to clean the implants, chew food with them, smoke or spit. When rinsing your mouth, be very careful and don't do it too vigorously.
- Avoid strenuous physical activity in the first three days after installation.
- Air travel, sudden changes in altitude and ambient pressure are prohibited. This provokes the risk of bleeding, since the wounds have not yet completely healed.
- When you sleep, use a high pillow or several to keep your head elevated relative to your body.
- It is necessary to stop taking medications that affect blood clotting. Please consult with your dentist and the doctor who prescribed these medications. It is necessary to assess the risks that accompany their use and withdrawal and compare which condition will be more stable.
- Consult your dentist regarding the choice of toothbrush.
- Avoid general overheating or hypothermia of the body, sudden changes in blood pressure.
Symptoms of gum inflammation that should alert the patient
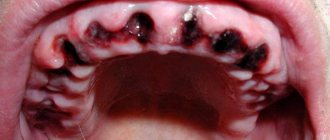
If after installation of implants there is some swelling, bleeding and soreness of the gums, this is not considered a pathology. Because it is a natural reaction of the body to soft tissue injury. These symptoms ideally go away on their own within 3-5 days after surgery. When pain and swelling persist for a longer period and tend to increase, this indicates the onset of gum inflammation - peri-implantitis. His symptoms look like this:
- Acute pain, swelling, redness of the gums, which persist, does not decrease or increases 3-4 days after implantation;
- Bleeding or discharge of ichor from the gums for more than 5-7 days after surgery;
- When pressing on the implant, there is pain - this indicates a violation of osseointegration;
- Mobility of the dental structure;
- Enlargement and tenderness of the submandibular lymph nodes;
- Purulent discharge from the gums, formation of a fistulous tract;
- Bad breath; when examining the structure, the doctor discovers the source of the odor under the plug or abutment;
- Increased body temperature, fatigue and drowsiness one day after surgery.
IMPORTANT! Gum inflammation after dental implantation can begin several months or even years after surgery. Although immediately after the installation of the implant, healing took place on time and without complications. After a lot of time, the patient may lose sight of the subtle redness of the gums. And during this period, the process of bone destruction will begin, which will lead to rejection of the implant rod.