What is a stump tab
A stump inlay is a microprosthesis, which is a dental abutment made of metal, ceramic or zirconium dioxide. It is used in case of significant destruction of the crown part of the tooth and intact root. The prosthesis fills the resulting void and creates a support on which an artificial crown is applied. Before installing the inlay, the tooth must be cleaned.
A stump inlay on a tooth is one of the reliable methods of prosthetics. Thanks to a well-sealed channel and the choice of high-quality materials (such as gold), it can last up to 15-20 years.
Orthopedic dentistry has a number of requirements for the use of inlays:
- absence of purulent-inflammatory process around the root;
- the dental canals must be well passable along the entire length of the pin;
- the root stump should protrude above the gum, the walls should be of sufficient thickness (at least 2 mm).
The decision on the treatment method is made by the doctor after X-ray diagnostics, taking into account how much the tooth tissue is destroyed, how long it will take to develop the root canals for the pins, what kind of load will be on the tooth, that is, will it serve as a support for the prosthesis or is it a one-time restoration.
Manufacturing technology of stump inlays
- Layering ceramics. After receiving the impressions, a refractory model is made, a ceramic pin is firmly installed in the canal, ceramic is applied and fired. In the process of applying ceramic layers, you can choose different colors and shades of material, dyes and modifiers.
- Production of ceramics by pressing from tablet molds. The liner is modeled from wax, the sprues are installed in the direction of the ceramic flow. Using a silicone ring, a lining material is inserted and a limiter is placed. Pressing takes place in an oven equipped with a microprocessor control system. The resulting product after pressing and casting is a solid single crystal, the abrasion of which is comparable to the natural abrasion of hard tooth tissues.
- Manufacturing using CAD/CAM method. Allows you to create prostheses and parts that match the implant, abutment, and abutment shape. The device is scanned in the oral cavity or on a model, 3D modeling is performed using a special program, the information received is transferred to a drill, which mills the product under computer control. An accurate and sophisticated method that requires high costs for professional training of personnel to operate the equipment.
- Injection molding method. Casting a working model from plaster / polyurethane, choosing an ashless pin according to the type of root canal, applying silicone varnish to the root. The pin is inserted into the canal and an ashless plastic/wax modeling is performed. After a control check, the cast abutment inlay is removed and transferred to a metal casting. The method is technologically advanced, economical, requires a minimum of material costs, but is very sensitive to the quality of the casting. With strict adherence to all norms and rules, reliable and high-quality microprostheses are obtained.
Materials for manufacturing stump inlays
- Metal stump tab. The metal abutment inlay can be made of an alloy of chromium and cobalt, there are also inlays in a silver abutment and inlays in a gold abutment. They are reliable, but not aesthetically pleasing, which is why in modern dentistry gold supporting inlays and silver microprostheses are used quite rarely and only for chewing dentures.
- Metal-ceramic liner. A metal-ceramic abutment inlay is quite durable, but its quality is worse than that of inlays made from other materials due to the difference in the thermal expansion of metal and ceramic. Therefore, such microprostheses often fall out.
- Ceramic inlay. The ceramic abutment insert best preserves the aesthetics of a smile, since ceramics in its properties and appearance are as close as possible to natural tooth enamel. Therefore, the abutment tongue on the front tooth is made from this material.
- Zirconium stump inlay. The advantage of such structures lies not only in their high strength, but also in the white color of the abutment insert made of zirconium dioxide, which is not visible through the crown. Therefore, as an answer to the question “Which abutment inlays are better?” Together with a ceramic inlay, we can safely call an oxide or zirconium dioxide inlay a pin. Therefore, the anterior tooth stump can also be made of zirconium.
- Composite stump inlay. The type of inlay is suitable for a stump with a pin, which adheres better to the tooth tissue than others, but is not strong enough compared to inlays made from other materials.
Anchor pins for tooth restoration
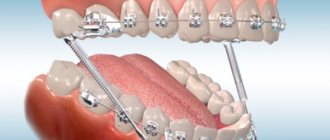
Anchor pins are often used to restore pulpless teeth. Anchor pins are metal pins that are fixed into a canal to build a tooth stump for a future crown or direct restoration.
They are threaded and fixed into the root canal using special cement. At one time they were very widely used in dentistry. However, they soon began to be abandoned, and we tried to figure out why.
Positive and negative properties of anchor pins
If we talk about the advantages of using anchor pins for restoration, they include:
- strength - such pins do not break
- affordable price
- speed and ease of use
What's wrong then? Let's look at all the shortcomings:
- low connection - there is no chemical connection between the intra-root and coronal parts, so they can easily separate
- poor aesthetics, especially if the work is done on the front teeth
- high risk of root fracture, since when installing an anchor pin, tension occurs inside the tooth root, which leads to a wedging effect, plus necrosis of the tissue around the tooth root, which leads to tooth extraction
The speed of installation of the anchor pin also plays an unpleasant role here. Fast does not mean easy. After all, each anchor pin system has its own installation rules and special auxiliary tools, which, unfortunately, are often neglected.
Types of stump inlays
Collapsible and non-collapsible
Non-separable is a one-piece structure containing one abutment and 1-2 supports in the channels. Unbendable ones are often made by casting, so they are very strong and durable. They are used to restore teeth with one or two canals.
Collapsible - used in multi-rooted teeth with two or three root canals. The design consists of several pins fixed in the channels. The products are used when, due to the complex anatomical structure of the tooth, it is impossible to cast an inlay. The process of creating and pinning folded cards is more complex, but effective. Therefore, structures are widely used to restore teeth that have been destroyed by more than 50%.
Single-channel and multi-channel
Depending on the number of channels, designs are: single-channel, two-channel, three-channel and four-channel. The latter are used quite rarely; often 2-3 pins are enough to restore even a large molar. Products in 1-2 channels are cast structures made of various materials. Tabs with 3-4 channels are often made foldable. They are made from metal alloys.
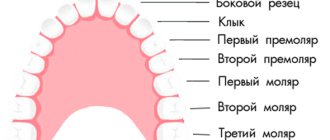
Inlays for front and chewing teeth
In the frontal region, the teeth have a root, so single-rooted teeth are used for treatment. The front teeth are visible when smiling and talking, so aesthetic materials are used to make products - ceramics, fiberglass. They are light or transparent, completely hidden from others. Such tabs do not spoil the appearance, do not shine over time and do not cause inconvenience.
Products for chewing teeth can have a different number of pins - from 1 to 4. A variety of materials are used for their manufacture. The choice of design should be made by a specialist, taking into account the wishes of the patient and the individual characteristics of the clinical situation.
tabs. orthopedics
ORTHOPEDIC TREATMENT OF PATHOLOGY OF DENTAL HARD TISSUE USING INLOTS
Classification of tabs
Tab
- a microprosthesis that fills a defect in the crown of a tooth, restoring its anatomical shape.
The inlay is a filling made in a laboratory. Unlike the therapeutic treatment of defects in the crowns of teeth, when the filling material is introduced into the tooth cavity in a plastic state, the inlay is introduced into the formed cavity in a solid state. Therefore, orthopedic treatment using inlays has obvious advantages and ensures:
• a strong connection of the inlay with the dental tissues due to the precise fit of the mating surfaces;
• the possibility of reliable restoration of interdental contact points, corners and tubercles of tooth crowns, taking into account the age and individual characteristics of natural teeth; • prevention of caries relapse by compensating for the shrinkage of the material during the manufacture of the inlay, constancy of the inlay’s volume and its precise marginal fit; • wear resistance and durability of the insert due to high mechanical strength; • color stability due to the denser structure of materials formed in the laboratory. For these reasons, replacing defects in hard dental tissues with inlays in many cases turns out to be more reliable than filling. Depending on the method of transmitting chewing pressure, microprostheses are classified:
• into restorative
- normalize the chewing pressure exerted on the periodontal tissues through the tooth on which they are applied;
• loading
- used for partial restoration of dentition as a support for bridges and additionally loading abutment teeth;
• distributing
- redistributing chewing pressure when splinting teeth.
In this regard, inlays are used:
• as independent structures for restoring the shape, function, and aesthetics of damaged tooth crowns (with IROPZ values from 0.3 to 0.6): - for carious lesions, especially in cases where tooth filling is ineffective ( cavities in the area of the necks of the teeth, chewing tubercles, corners and cutting edges of the front teeth);
— for defects of hard tissues of non-carious origin (wedge-shaped defects, increased abrasion of hard tissues, traumatic defects); • as elements of pinned teeth or an artificial stump with a pin; • as supporting elements of short bridges (no more than 1-2 extracted teeth); • as elements of splinting structures in the treatment of periodontal diseases. Contraindications to the use of inlays:
• small-sized carious cavities (with IROPV values less than 0.3);
• significant destruction of the coronal part of the tooth with IROPV values greater than 0.6; • teeth with defective (fragile, discalcified) hard tissues; • teeth with poorly accessible cavities. It is proposed to classify inlays according to the following criteria:
• topography of the defect;
• designs; • materials; • manufacturing methods. Classification of inlays according to the topography of the defect (classification of cavities for inlays)
The most common cause of defects in the crown of teeth is caries. In this regard, from the point of view of microprosthetics, classification of caries according to topographical criteria is of great importance.
An example of such a classification is the classification of G. Black (1891)
, in which all carious cavities, depending on their location, are divided into 6 classes.
The main advantage of this classification is its ease of use in the work of a dentist. Having established which class the cavity belongs to, it is easy to predetermine the typical formation of this cavity to create the most favorable conditions for fixing the inlay and preventing the possibility of secondary caries. From a practical point of view, it is easier to navigate the localization of cavities if, instead of classes, we use the letter designation of the surfaces on which the cavities are located (Boyanov B., 1960):
•
O
- cavities on the occlusal (chewing surface);
• M
- cavities on the medial surface;
• D
- cavities on the distal surface;
• MO
- cavities that simultaneously cover the medial and occlusal surfaces;
• MOD
- cavities localized on the medial, occlusal and distal surfaces.
Classification of inlays by design
Depending on the degree of destruction of the coronal part of the tooth and the method of placing the microprosthesis in hard tissues, inlays can replace missing tissue to a greater or lesser extent.
There are four main types of inlay designs (Fig. 1-1): • inlay
- a microprosthesis located centrally and not affecting the cusps of the tooth, the least invasive (Fig. 1-1, a);
• onlay
- a microprosthesis that affects the internal slopes of the tubercles in the form of an overlay (Fig. 1-1, b);
• overlay (overlay)
- a microprosthesis covering from 1 to 3 tubercles.
The structure covering 4 tubercles can already be classified as three-quarter crowns (Fig. 1-1, c); • pinlay (pinlay)
- a microprosthesis strengthened in the tooth using pins (pins) located in the hard tissues of the tooth (Fig. 1-1, d). When making such structures on chewing teeth, as a rule, all the tubercles are covered. On the front teeth, it is possible to make a pinlay while preserving the vestibular surface and cutting edge. Thus, pinlay inlays on incisors and canines resemble a half-crown with a pin.
Rice. 1-1. Types of microprostheses: a - inlay - located inside the tooth crown; b - onlay - used when it is necessary to restore most of the chewing surface of the tooth crown; c — overlay — covers the side walls of the tooth crown; g - pinlay - prosthetic tab with a pin
Classification of inlays depending on the material
Depending on what material is used to make inlays, they are divided into:
• metal - made of titanium;
• plastic (acrylic series, polyurethane series, nylon, etc.); • ceramic - from classic porcelain, titanium oxide, zirconium oxide; • composite (keromer); • combined - metal-composite, metal-ceramic.
The type of material for the manufacture of inlays determines the features of the formation of the cavity for the inlay and its design features, the features of the clinical and laboratory stages and the method of manufacturing the inlay. Regardless of the material for making the inlay, its design features, or manufacturing method, at the first clinical stage, after a thorough clinical examination, diagnosis and drawing up a treatment plan, the cavity is prepared for the inlay. Preparing a cavity for an inlay
This is an operation of excision in a certain sequence of hard tissues of the tooth crown to give the cavity the desired shape. Like any surgical intervention, preparation of a cavity in vital teeth under an inlay may be associated with the development of early or delayed complications: • postoperative tooth sensitivity; • opening of the tooth cavity; • acute and chronic pulpitis; • secondary caries. The development of complications may be due to the action of local damaging factors: mechanical trauma, drying, hyperthermia, vibration, microbial invasion. Therefore, to prevent the development of complications, the formation of cavities for inlays in teeth with preserved pulp is performed with adequate pain relief, in compliance with the general rules, principles and preparation regimes.
• Preparation of vital teeth for inlays, more than for other types of orthopedic structures, is associated with the risk of damage to the pulp (traumatic pulpitis). Therefore, when preparing a cavity for an inlay, it is necessary to take into account the anatomical and topographical features of the tooth being prepared: the structure and thickness of hard tissues in different areas, the topography of the tooth cavity. Excision of hard tissues should be carried out under X-ray control and taking into account safety zones (Abolmasov N.G., Gavrilov E.I., Klyuev B.S., 1968, 1984), with control of the depth of preparation. • Dissection should be carried out intermittently, with well-centered, sharp instruments, under full air-water cooling (50 ml/min). The water temperature should not exceed 35 °C. • When preparing, it is necessary to observe the speed modes of preparation for enamel and dentin. • To prevent the development of secondary caries, it is necessary to control the quality of removal of infected dentin. • After preparation, the prepared dentin must be protected. • Preparation of a carious cavity consists of the following stages:
— excision of all hard tissues affected by the carious process and complete removal of infected dentin (necrotomy);
— preventive expansion of the cavity; — formation (special preparation) of a cavity of the desired shape. When forming cavities for inlays, carbide and diamond burs of the following shapes are used: spherical, cylindrical, cone-shaped, flame-shaped. By sequentially using diamond and carbide burs of the same shape and size, the most optimal conditions for preparation are created. Removal of infected dentin and preliminary formation of a cavity in dentin is recommended to be carried out using carbide burs with a small number of blades. At the main stage of cavity formation, it is advisable to use diamond burs, at the final stage - carbide burs with a large number of blades (finers) or diamond burs with red markings. General principles of forming cavities for inlays
The main features of preparing teeth for inlays, as opposed to fillings, are the creation of relative parallelism of the side walls for the possibility of introducing the finished structure, as well as the need for preparation to a depth that ensures sufficient strength of the inlay.
To ensure reliable fixation of the inlay while maintaining cavity edges that are resistant to chewing pressure and to prevent relapse of caries during cavity formation, certain principles must be observed.
• The cavity is given the most appropriate shape, such that the insert can be easily removed from it in only one direction. In this case, the vertical walls of the cavity should be parallel or slightly diverge (diverge). The slope of the walls is not a constant value and can vary depending on the depth of the cavity: for superficial cavities the slope should be less, for deep ones it should be greater. • The bottom and walls of the cavity should be able to withstand chewing pressure well, and their relationship should contribute to the stability of the inlay. The design of the angle formed by the outer walls and the bottom of the cavity has a certain significance for stability. The angle of transition of these walls into the bottom should be clearly defined and approach a straight line. • The bottom of the cavity should be parallel to the roof of the tooth cavity and be of sufficient thickness to protect the pulp from external influences. Depending on age, the safe thickness of dentin above the pulp cavity can range from 0.6 mm for teeth whose root formation process has already been completed, and 1.4 mm for teenage and young adult teeth with wide and open dentinal tubules.
• To prevent relapse of caries, it is necessary to carry out preventive expansion of the cavity. • When forming a complex cavity that involves several surfaces of the tooth, retention elements should be created to prevent the inlay from moving in different directions. Additional retention points should be created if at least one outer wall is missing or its height is insignificant. Fixation elements can have different shapes: cross-shaped, T-shaped, dovetail. • The cavity for the inlay must have sufficient depth with mandatory immersion into the dentin. • The formed cavity should be asymmetrical or have additional recesses that serve as guides when inserting it into the cavity. There should be no undercuts that would interfere with the removal and insertion of the inlay. In each specific clinical case, the method of preparing hard dental tissues for an inlay will differ depending on the class of hard tissue defect and the material used to make the inlay. Thus, the peculiarities of cavity formation in the manufacture of metal inlays include the creation of a bevel (rebate) in the enamel with a width of at least 0.5 mm at an angle of 45° relative to the internal walls of the cavity, which ensures an accurate marginal fit of the inlay to the enamel, increasing its retention area ( Fig. 1-2).
Rice. 1-2. The finally formed cavity with the creation of a bevel (rebate) in the manufacture of a metal inlay
When making metal-free inlays, creating bevels in the enamel is contraindicated due to the properties of the materials - their fragility in the presence of a thin layer in the area of the transition to the tooth enamel. In addition, when making metal-free inlays, the internal corners of the cavity should be slightly rounded, the outer boundary of the cavity should be within the enamel (Fig. 1-3). When forming a cavity for composite, ceramic inlays, the edges of the cavity are not finished to ensure a high degree of fixation.
Rice. 1-3. The final formed cavity for the manufacture of a non-metallic (ceramic, composite) inlay
Preparation of cavities of the 1st class according to Black
Class 1 cavities (Fig. 1-4) are characterized by the preservation of all outer walls, which, if the cavity is formed correctly, prevent displacement of the inlay. The stability of the inlay is ensured by the depth of the cavity and the angle between the bottom of the cavity and its walls.
Rice. 1-4. View of a mandibular molar after completion of the formation of a class 1 cavity under an inlay
Class 1 cavities, located on the chewing surfaces of molars and premolars, are formed at the locations of fissures and intercuspal fossae. The cavities are given a typical shape: they should follow the fissure pattern without the formation of sharp corners (see Fig. 1-4). When forming a cavity, elements are created (bottom, walls of the cavity, bevels, etc.) that have a certain functional significance. The main wall of the cavity, which takes on most of the chewing pressure, is the bottom. It is formed parallel to the chewing surface and perpendicular to the long axis of the tooth. The tilt of this cavity wall is permissible only towards the strong outer wall. The tilt of the cavity bottom towards the weakened wall can cause a fracture of the tooth crown. When forming deep cavities to prevent perforation, one should not strive to form a flat bottom by grinding off the hard tissues of the tooth. If the bottom of the cavity is concave, it is subsequently leveled with lining material. To prevent recurrence of caries during the formation of class 1 cavities, enamel prisms that have lost contact with dentin must be ground off. For this purpose, the enamel wall must be given the most favorable slope, taking into account the radial direction of the enamel prisms along the edge of the tooth defect.
When forming cavities of the 1st class, you should not make them with symmetrical contours (round, oval) - this will complicate the fit and may cause incorrect fixation of the inlay in the tooth crown. To add asymmetry, the cavity is slightly lengthened or expanded towards one of the fissures. If there are two or more cavities on the occlusal surface, they are combined into one. Preparation of class 2 cavities
Class 2 cavities are characterized by destruction of the contact surfaces of the chewing teeth. The preparation of a 2nd class cavity begins with separation, which is carried out with a thin diamond head to the level of the tooth neck. The separation plane must be strictly vertical or slightly inclined towards the center of the tooth crown. Then, using a fissure bur, a cavity is formed on the contact surface to create a ledge and an additional area on the chewing surface (Fig. 1-5). The gingival wall of the cavity should be located at the level of the gingival margin. An additional area on the occlusal surface is intended both for preventive expansion of the cavity and to prevent displacement of the inlay towards the missing wall. On the chewing surface, hard tissues are excised, bypassing the intact slopes of the tubercles, and the cavity acquires a complex shape, which ensures good fixation of the inlay. If both contact surfaces of the tooth crown are affected, it is necessary to form a three-sided cavity (both contact and chewing surfaces are prepared) even if there is a filling on one of the contact surfaces. In this case, separation is carried out and, according to general rules, cavities are formed on both contact surfaces, which are then connected to each other by the cavity formed during excision of the chewing groove. To prevent chipping of the vestibular or oral walls of the cavity, which are under load during chewing, it is often necessary to grind off the tubercles, then restoring them with the inlay material.
Preparation of class 3 cavities
There are three degrees of destruction of the tooth crown with caries of the contact surface:
• without disruption of the labial or oral surface;
• with damage to one of them; • with simultaneous destruction of the labial, contact and oral surfaces. Depending on the degree of destruction of the crown, the method of forming cavities changes.
When only the contact surface is affected, the cavity is formed in the form of a triangle with the apex facing the cutting edge and the base parallel to the gingival edge. The bottom of the cavity should be convex, repeating the contours of the contact surface of the crown. The formation of such a cavity is possible in the absence of adjacent teeth.
Rice. 1-5. View of a mandibular molar after preparation of a class 2 cavity for making an inlay
Rice. 1-6. View of the maxillary canine after completion of the formation of a class 3 cavity under the inlay
In case of combined lesions of the contact and oral (or labial) surfaces, the cavity is formed taking into account the insertion path of the inlay and the creation of an additional fixation platform (usually in the form of a “dovetail”). An additional cavity is created in proportion to the main one, immersing it in dentin. The transition from one cavity to another is designed in the form of a step. When forming a cavity under the inlay, cavity elements are formed, each of which carries a certain functional load (Fig. 1-6). With the simultaneous destruction of the contact, oral and vestibular surfaces, additional depressions are created in the dentin from the labial and oral surfaces to hold the inlay. At the same time, the axial wall of the cavity is preserved in the form of a roller, which will protect the pulp chamber. If there are cavities on both contact surfaces, they are connected by a fairly wide groove passing through the blind fossa.
Preparation of class 4 cavities
The nature of the formation of cavities of the 4th class depends on the structural features of the cutting edge. Teeth with destruction of the cutting edge are divided into two groups depending on its width. As a rule, teeth with a wide cutting edge are found in older people, in patients with increased wear of hard dental tissues. In such teeth, between the layers of enamel there is a fairly thick layer of dentin, which makes it possible to create a cavity or an additional fixing platform in it. In this regard, the need to prepare the palatal surface of the tooth crown is eliminated, and the inlay located on the cutting edge protects the tooth from further abrasion. The shape of the prepared main cavity located on the contact surface must be such that the path of insertion and removal of the inlay coincides with the long axis of the tooth, and the gingival wall is perpendicular to the long axis of the tooth. In addition to the main cavity, an additional platform is created in the cutting edge in the form of a groove, commensurate with the main cavity and the width of the cutting edge. This groove may end with a recess in the form of a channel, into which a pin fixed in the inlay will subsequently enter, improving its fixation, or it may move into a cavity on the other contact surface (in case of damage to both contact walls of the tooth). In teeth with a thin cutting edge, the formation of the main cavity is carried out in the middle third of the tooth crown, perpendicular to the palatal surface. This direction determines the insertion path of the tab. The bottom of the main cavity becomes the labial wall of the tooth crown. To ensure fixation of the inlay, an additional platform is formed in the area of the blind fossa at the base of the dental tubercle with immersion in the dentin. If both contact surfaces are affected with a violation of the angles of the cutting edge, the latter is used to form a step and create a saddle-shaped connection of the proximal cavities. When the cutting edge is chipped, it is ground off, creating a bevel from the oral surface. Then a cavity is formed taking into account the topography of the tooth cavity with the creation of vertical channels for the pins. The canals should run midway from the pulp to the enamel edge.
Class 5 Cavity Preparation
When forming cavities in the cervical region, it is necessary to take into account the proximity of the cavity to the equator and the danger of opening the pulp chamber located close to the surface of the tooth.
The expansion of the cavity is carried out to the greatest curvature of the tooth crown in the area of the equator and contact surfaces. The bottom of the cavity is formed convex, especially on the front group of teeth. The gingival wall is formed at the level of the gingival margin, except for those cases when there remains a section of intact hard tissue at least 2 mm wide between the edge of the cavity and the gum. The mesial and distal walls of the cavity must be at a certain angle to each other, and the wall facing the cutting edge (or occlusal surface) and the gingival wall must be parallel. This ensures retention of the tab. Protection of prepared dentin
After preparation, to protect dentin from irritating factors, its dentinal tubules are sealed using desensitizers - materials whose operating principle is based on sealing dentinal tubules in various ways. The main effect of using desensitizers is to reduce the sensitivity of prepared dentin. During the production of the inlay, the cavity formed in the tooth must be closed with a temporary filling, which protects the tooth from thermal, chemical, mechanical and microbial influences in the postoperative period.
Why core inlays are better than fillings and pins
Fillings and pins are only applicable if the tooth has a sufficient amount of healthy tissue. If only the root or thin walls of the tooth remain, it will not be possible to restore it with a pin, since this restoration method will not differ in either quality or reliability.
Firstly, under load, the pin can break and damage the tooth root. Trauma to the root of a tooth is a direct indication for its removal; In case of damage to the root system, no technique will help save the tooth.
Secondly, dentures installed on large fillings and pins are more likely to fall out some time after prosthetics. In this case, the treatment will have to be repeated, and this entails new significant financial costs.
Important: Some dentists try to cement a fallen crown and post using cement. But this is useless - the structure will not hold firmly and, moreover, an inflammatory process can begin under it, which leads to caries.
Therefore, in the case of severe caries, only an abutment inlay can provide high-quality and durable prosthetic results.
Ceramic inlay e max: main indications
Many people mistakenly believe that ceramic inlays are a type of regular filling. In fact, they belong to the category of high-tech microprostheses. Its parameters and characteristics significantly exceed any, even the most modern and high-quality filling material. Among the main indications for installing ceramic inlays are:
- destruction of the coronal part by 30% or more;
- preparing a molar or premolar for the installation of permanent orthopedic structures, for example, bridges;
- increased abrasion of enamel;
- the presence of a large cavity that was formed as a result of an advanced carious process;
- increased sensitivity of molars or premolars to external factors;
- mechanical damage.
If, after fixing the orthopedic structure, pronounced painful sensations occur, you should not delay your visit to the dentist. Most often, pain and discomfort are a sign that the product was installed incorrectly. To avoid such situations, treatment should be carried out only in trusted dental clinics.
Indications and contraindications for the installation of stump inlays
Installation of dental inlays is indicated in the following cases:
- crown inlay for prosthetics;
- fracture of the crown of the tooth;
- carious destruction of the crown;
- abnormalities in the position, shape or size of the tooth;
- low dental crown;
- production of a bridge prosthesis, when the stump inlay for the tooth is used as a supporting element;
- need for splinting.
The strength of fixation, quality of construction and durability of the product depend on the condition of the tooth root when a microprosthesis is installed into it. The root should not wobble, it should be free of curvature in the upper third, with passable and well-sealed canals and walls of sufficient thickness for prosthetics. The use of an abutment design is not recommended in the following cases:
- circular ligament damaged;
- resection of the root apex (temporary relative contraindication), as well as inflammatory processes that can injure the gums or root tissues;
- poor hygiene;
- incomplete obturation of the canals;
- mobility 3 degrees.
In each clinical case, the decision to place an abutment design is made by the treating orthopedic surgeon together with the relevant specialists, taking into account all the advantages and disadvantages of using this reconstruction. If there are relative (temporary) contraindications, therapeutic or corrective surgical treatment, as well as replacement of incompetent orthopedic structures, can be performed before prosthetics.
The procedure for manufacturing and installing the stump tab
Production and installation take place in several stages:
Preparation
It includes an examination, consultation, treatment plan and selection of an appropriate design. At this stage, the oral cavity is disinfected and the roots are prepared for dentures. Next, the doctor takes impressions of the tooth, since the pins of the structure must accurately follow the shape of the root canals. The impressions are sent to a dental laboratory for subsequent production.
Production
A dental technician makes plaster and wax models. Based on the models, make an insert insert from the selected material, taking into account the specifics of the manufacturing technology.
Installing a tab
During the follow-up examination, the doctor prepares the root canals and fills them with dental cement. For better fastening, the studs of the structure are pressed forcefully into the solution.
Preparation for prosthetics
The specialist makes repeated impressions for the subsequent production of the crown.
How stump inlays are made: an overview of the main stages
Stump inlays are made individually for each patient. Treatment begins with an examination of the patient and consultation with two specialists – a general dentist and an orthopedic dentist.
Before an impression is taken from the tooth, according to which a stump insert will be made, high-quality sanitation of the oral cavity is carried out, and all diseases of the teeth and gums diagnosed during the examination are treated. The damaged tooth is treated: the nerve (pulp) is removed from it, and the canals are filled. This is where the work of the dentist-therapist ends and the orthopedist begins to care for the patient.
Further treatment will proceed according to the following scheme:
- The prosthetist will correctly prepare the tooth for installation of the stump inlay and select its type.
- When choosing the type of stump tab, the material of its manufacture and the type of tab (single-root or multi-root, cast or collapsible stump tab) are determined.
- Then the doctor will make an impression of the patient’s jaws, which will be sent to the dental laboratory, where a stump inlay will be made from the impression taken.
- Based on the impression, a model of the stump inlay is first made, and then a permanent structure is made from the selected material.
- The dental technician passes the finished stump inlay to the orthopedist.
After the stump inlay is ready, the patient is invited to the prosthetist’s office and the doctor installs the stump inlay in the tooth canals. A temporary prosthesis is put on the tab and a break is taken in the treatment until the crown is made, which the doctor fixes on the stump tab.