If the dentist asks the patient: “What kind of filling are we going to put in?” - then the patient will find himself in a difficult situation, because usually he has a very poor idea of not only the composition of a dental filling, but also the differences between different types of fillings. To have an idea of how caries is treated and what results to expect from it in the future, it will be useful to learn about the different types and compositions of filling materials.
Cements
Cement fillings come in several types, depending on the composition of the material:
- silicate;
- silicophosphate;
- phosphate;
- glass ionomer.
The first three groups are rather fragile cements, low resistance to abrasion and characterized by not very reliable fixation in the carious cavity. They were installed everywhere in the past, but today such materials are considered obsolete and are used extremely rarely. It is advisable to use them only in the treatment of primary teeth, when special durability of the restoration is not required, but ease of installation and low cost are important.
Glass ionomer cements are a new generation of filling agents, since in this case the tooth filling contains components that can release fluoride and thereby prevent the development of secondary caries. This cement has a high chemical affinity for natural dental tissues and good marginal adhesion. However, glass ionomers have not completely eliminated all the disadvantages of cements, such as low strength, which is why they are also recommended for use mainly in pediatric dentistry. Such fillings are also suitable for treating children because they are relatively inexpensive and can be given different color shades - and colored fillings have become especially popular lately.
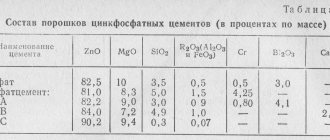
Silico-phosphate cements
They are silicate cements modified with zinc phosphate cements. In terms of their chemical and physicochemical properties, they are superior to silicate cements, but inferior to them in terms of aesthetic indicators. Typically the powder contains 60-90% silicate cement powder and 10-40% phosphate cement. The liquid is a solution of orthophosphoric acid modified with zinc and aluminum oxides.
Silico-phosphate cements are more stable in a humid environment and have better high strength properties than silicate cements. However, there is also an irritating effect on the pulp, so it is mandatory to use an insulating gasket. They have very low aesthetic indicators (they are poorly ground and polished, have no shine, and the color does not match the hard tissues of the tooth). They are used as permanent filling materials for filling premolars, molars, anterior teeth, if the fillings do not extend to the vestibular surface, as well as temporary fillings with a long service life.
Representatives: “Silidont-2” (Medpolymer), “Universalcement” (SPAD), etc.
I especially wanted to highlight the cements “Lactodont” (Medpolymer) and “Infantid” (Dental Spofa), which are used for filling baby teeth. Due to the increased content of zinc oxide, orthophosphoric acid is neutralized relatively quickly and cement has virtually no irritating effect on the pulp. For superficial and medium caries, they can be used without an insulating lining; for deep caries, a lining is necessary.
Positive properties of silicophosphate cements:
- greater mechanical strength than silicine and phosphate cement;
- less irritating effect on the pulp than silicine (due to the content of zinc oxide);
-better adhesion to tooth tissue than silicine;
— ease of use;
- low cost and availability.
Negative properties of silicophosphate cements:
— unsatisfactory aesthetic qualities;
- insufficient strength;
— insufficient resistance to the oral environment;
— toxicity to dental pulp (used with an insulating gasket!).
Indications for the use of silicophosphate cements:
1. Class I cavities (on the incisors - in the area of the blind fossa).
2. Class III cavities (on the lingual surface of the teeth while maintaining the enamel from the vestibular surface).
3. Small class I cavities in molars and premolars.
4. Filling teeth that are planned to be covered with artificial crowns;
5. Filling teeth with III degree of mobility in case of periodontitis.
Plastics and composites
An extensive group that includes:
- Acrylic-containing plastics. They are resistant to abrasion, but at the same time porous and quite toxic, so they have been used less and less in recent years.
- Composites with epoxy resins (chemically cured). Slightly better than plastic, but quite fragile and darken a few years after installation.
- Light-curing composites (photopolymers). Strong, reliable and durable. They polymerize and harden under the influence of ultraviolet radiation. The composition of a photopolymer tooth filling includes porcelain, which gives the material strength and aesthetics. The most popular option today.
Composition, properties
The powder consists of 5 parts silicate and 4 parts phosphate cement, which are made.
The liquid is orthophosphoric acid, which has been partially neutralized with aluminum hydroxide (Al(OH)3) and zinc oxide (ZnO).
- high mechanical strength;
- high chemical resistance;
- sets quickly;
- plastic;
- radiopacity;
- ensures the tightness of the filling, which reduces the risk of complications or relapse;
- bactericidal effect;
- high compatibility with biological tissues.
A significant advantage of the product is its low cost and the ability to purchase at any pharmacy chain.
Metals
Metal filling materials belong to the class of amalgams - alloys of various metals with mercury. Usually, upon learning that a dental filling contains mercury, the patient begins to fear its toxic effects. In fact, although there are many publications about the dangers of amalgams, the harm from them is much less than, for example, from smoking - a smoker receives more mercury from cigarette smoke than can, in principle, be released from a filling.
These are extremely strong and durable filling bases that can last for decades. Their main disadvantages are their unaesthetic appearance (they can only be installed on chewing teeth, which are not visible to others), a long curing period (2-3 hours) and difficulties in installation. The difficulty of installation lies in the fact that when hardening the material slightly increases in volume and, if the dentist does not calculate correctly, it can break the tooth wall.
Usually, when choosing, the patient pays special attention to cost. In fact, it is necessary to take into account both the service life and the “behavior” of the material in the mouth. After all, if you install a cement restoration and then change it every year, in the end the treatment will cost much more than installing a photopolymer.
Silidont cement for fillings
Silicophosphate cement (silidont) is a mixture of powders of two cements: 20% visphate powder and 80% silicine.
For 1 g of silidont powder, 0.25 - 0.30 ml of liquid is required. The quality of silydont is determined by the positive and negative properties of phosphate and silicate cements.
In silydont, the binding of phosphoric acid occurs more vigorously and completely than in ordinary silicate cement, due to the content of zinc oxide in sufficient quantities. However, when applying a silidont filling to a tooth with living pulp with a diagnosis of “deep caries,” a phosphate cement lining is also required, which protects the pulp from the action of incompletely bound phosphoric acid.
The optimal temperature for mixing is 18 - 20 °C. When working in a cold room (below 16 °C), in order to achieve the hardening time of cements, an excess of powder should be used when mixing compared to the recommended ratio. If the room temperature is above 20 °C, the glass plate must be cooled with a cotton swab soaked in ether before mixing. The glass plate for mixing the filling mass must be clean and dry. Do not mix on a warm or hot plate removed from the sterilizer. Mixing silicate cement (silicin) and silydont should be done with a plastic spatula. It is not recommended to use a metal spatula due to possible staining of the filling material.
12. Silicate phosphate cements. Compound. Principle of use and scope of application in dentistry.
Silica phosphate cements are a combination of zinc phosphate and silicate cement.
In terms of physical and chemical properties, it occupies an intermediate position between them. Silicate cement 95-60%, phosphate cement 5-40%.
1) mechanical strength; 2) less fragility than silicate cements; 3) better adhesion than silicate cements; 4) plasticity; 5) availability, low cost; 6) radiopacity; 7) coefficient of thermal expansion is close to dental tissues.
Negative: 1) discrepancy with the color of the tooth tissue;
2) toxicity (used with a gasket);
3) solubility and instability to saliva.
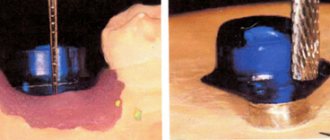
Technique for mixing silica phosphate cement
It is produced in the same way as for silicate cement, with the only difference that it is necessary to apply a little force to overcome the viscosity of the cement paste. In addition, it is necessary to add smaller portions of the powder so that the ingredients fully react with each other. The hardened mass of silico-phosphate cement is mainly a conglomerate of silicic acid gel and a crystalline mass of the hardening products of phosphate cement.
Due to this, silica phosphate cements are radiopaque.
Indications for use
• filling cavities of classes I, II, V premolars and molars (in the absence of more
modern materials or the presence of contraindications to their use);
• filling of temporary teeth in children.
Silico-phosphate cements are introduced into the cavity in several portions with careful
condensation. Previously, a gasket made of
The group of silico-phosphate cements includes:
• Silicap (Vivadent, Liechtenstein) in capsules;
• Infantid (Spofa Dental, Czech Republic);
• Lumikolor Cement (GC, Japan);
• Posterit Cement (GC, Japan)
Choosing temporary filling material: proceed without mistakes
- Login Registration
- Home →
- News and articles on dentistry →
- Therapy →
- Choosing temporary filling material: proceed without mistakes
Every practicing dentist knows how important the correct selection of filling material is for effective treatment. Modern dentistry offers a huge selection of materials, which are divided into classifications depending on composition, properties, time of use, purpose, etc. A fairly large place among them is occupied by a group of filling materials for temporary fillings, as well as insulating and therapeutic pads.
Materials for temporary fillings
Based on the time of action, they are divided into bandages and temporary fillings. Inexpensive materials are used for dressings. The most common option: water-based dentin or dentin-paste. The period of use of these materials should not exceed 14 days. At the same time, the bandages do not differ in aesthetics and durability. All temporary fillings are cements : zinc phosphate, zinc eugenol, polycarboxylate, glass ionomer, etc. The period of their use in the patient’s oral cavity ranges from several weeks to six months.
1) Zinc sulfate cements (“artificial dentin”)
The main components of the composition are zinc sulfate and zinc oxide. Adding water helps the mass harden. The most famous materials of this group: “Dentin for dressings”, Dentine paste, Vinoxol, etc.
The basis of the composition is zinc oxide and eugenol. According to Smith's classification (1996), this subgroup includes three main types of cements: simple zinc oxide eugenol; reinforced zinc oxide eugenol with filler and cements based on orthoethoxybenzoic acid (EBA). The materials consist of zinc oxide powder, into which 1-2% zinc acetate, acetic anhydride or rosin are added, which accelerate hardening. Purified eugenol or clove oil is used as a solvent. Additionally, to speed up the hardening process of cement, acetic acid or 1% ethyl alcohol, as well as a small amount of water, can sometimes be added. The most popular representative of this group is Cariosan. Zinc-eugenol cements are used not only for temporary fillings , but also for therapeutic linings. It is important to take into account that eugenol disrupts the polymerization process of composites, so experts do not recommend using this type of cement in combination with them. That is why today zinc-eugenol cements are practically not used for therapeutic linings in commercial clinics, but they are still in demand in pediatric dentistry and in municipal clinics for the treatment of deep caries in two visits.
75-90% of the cement base is zinc oxide with the addition of other modifying oxides. The liquid part is an aqueous solution of 38-44% orthophosphoric acid containing phosphates of zinc, aluminum, magnesium, etc. Among the most famous zinc-phosphate cements presented on the Russian market are: Phosphate cement from Raduga-R, Uniface ( “Medpolymer”), Adgesor (“Dental Spofa”), DeTreyZinc from “DeTrey/Dentsply”, etc. As a rule, metals containing silver are added to these compositions to impart a bactericidal effect. As an example, we can o), Phosphate with silver and bactericidal Foscin (“Rainbow-R”), as well as cements containing bismuth oxides: Visphate cement and Dioxyphosphate (Medpolymer).
The undoubted positive properties of these cements are: ease of use, low thermal conductivity, good X-ray contrast, and impermeability to acids and monomers. However, they have quite a lot of negative characteristics. Among them: weak adhesion, low resistance to the aggressive effects of saliva, shrinkage, low mechanical strength, the presence of free acid and lack of aesthetics.
Most often, zinc-phosphate cements are used as an insulating spacer for filling baby teeth and permanent crowns, fixing cast stump inlays, pins, crowns and bridges.
The basis of cement is thermochemically treated zinc oxide with the addition of magnesium oxide, which reduces the reactivity of the first component. Aluminum is also often added to powders. The solvent is represented by a 32-42% aqueous solution of polyacrylic acid. During the hardening process, cement turns into an amorphous zinc-polyacrylate gel, which contains zinc oxide particles.
The positive properties of these cements include: satisfactory chemical adhesion to enamel and dentin, strong bond with metals, weak toxicity to the pulp compared to phosphate cement and high biocompatibility with tooth tissues. Negative properties: high solubility under the influence of saliva, short formation time in the oral cavity and insufficient fluoride adhesion.
Polycarboxylate cements are used as insulating spacers when filling teeth under artificial crowns, for fixing orthopedic and orthodontic structures, and in the treatment of baby teeth (1-2 years before their replacement).
All materials for temporary fillings must be:
- harmless to the pulp;
- have high plasticity;
- inactive for other drugs;
- insoluble under the influence of saliva;
- sealed for at least two weeks;
- have a certain strength;
- easily removed from the dental cavity using an excavator, probe or drilling.
Insulating and healing pads
The purpose of these materials follows from their name. Despite the fact that they can be conditionally classified as filling materials, the application of gaskets is an integral step in the treatment of medium and deep caries. spacers when treating medium and deep caries . They contain calcium hydroxide, which has an anti-inflammatory effect on the pulp and stimulates the deposition of replacement dentin. Among the most popular materials are: “Calmecin”, “Dycal”, “Calcimol” and “Alcaliner”, as well as modern insulating gaskets made from glass ionomer cements, such as: “Fuji 2”, “Chelon Fil”, “Base Line” and etc.