Local swelling of the root zone, compactions of various sizes, throbbing pain, sensitivity to temperature when eating, enlarged lymph nodes may indicate an acute inflammatory process of infectious etiology. In dentistry, there are several types of diseases, among them periapical abscess. It can be caused by advanced caries, chipping of an element of the dental system, overheating of the pulp due to tooth preparation and various pathologies. This can also happen due to poor-quality root canal treatment.
A periapical tooth abscess is an accumulation of pus between the molar and the gums. Purulent exudate can accumulate both in the inner and outer surfaces of the alveolar process of the lower or upper jaw. It most often begins in a tooth with a non-viable pulp, when the nerve dies, causing infection and progressive inflammation. The infection may gradually spread to surrounding tissue. Clinical symptoms are in many ways similar to acute periodontitis. The patient experiences increased sensitivity, acute pain, the mucous membrane may have swelling, there is active hyperemia, and overflow of blood in the vessels of the circulatory system.
Symptoms
- Intense dull throbbing pain.
- Discomfort when chewing food.
- Swelling in this area.
- Painful sensations when swallowing.
- Enlarged lymph nodes.
- Unpleasant sensations when opening the mouth.
- Change in molar color.
Other symptoms also include malaise, fever, weakness, and bleeding. It should be noted that in some cases the inflammatory process can be practically asymptomatic; activation can occur periodically, for example in the case of hypothermia. In this case, immediate assistance from a dentist is required so that he can quickly and accurately diagnose and establish a treatment regimen for effective recovery.
Causes of abscess
Complications associated with the inflammatory-destructive process can occur due to the following reasons:
- Poor quality endodontic treatment.
- Carious formations.
- Injuries to elements of the dentition.
- Unqualified prosthetics.
- Infectious diseases in the maxillofacial area, such as sinusitis.
Treatment of a periapical abscess without a fistula may be required in case of violation of the endodontic therapy protocol or incomplete obturation of the canal system. Provoking factors can be serious infectious diseases, hypothermia, and a reduced level of the body's immune defense. Leukocyte infiltration also often causes the formation of an abscess and microabscess.
Kinds
Based on the nature of the localized accumulation of pus in the elements of the dentition and nearby structures, two groups of abscess are distinguished.
- Periapical abscess without fistula. In this case, transcanal infection of periodontal tissue is observed. The adjacent gum may have swelling, hyperemia is observed, pain is felt when biting on a molar, and the appearance of purulent exudate is recorded. The disease has a pronounced clinical picture.
- Periapical abscess with fistula. With this phenomenon, the inflammatory destructive process spreads to the bone marrow and mucous membrane. The fistula most often opens in the projection of the apex of the root element of the dentition. There may be hyperemia on the mucous membrane, a scar from a fistula, and the gums may be quite sensitive to palpation.
In case of periapical abscess without a cavity and with a cavity, complaints of intense dull throbbing pain, deterioration of general condition, and constant pain are recorded.
Modern strategy for successful periapical surgery
Abstract : Periradicular surgery is often the only way to save an endodontically treated tooth with a chronic focus of periapical infection. Thanks to the introduction of surgical microscopes, ultrasound, and modern filling materials into practice, the result of endodontic surgery has become more predictable. At the present stage, endodontic surgery has made significant progress: determining the position of the apex has become more accurate, osteotomy has become less invasive, resection angles have decreased and the quality of canal filling has improved. Thus, modern endodontic surgery has shown better long-term results compared to traditional periradicular surgery.
Introduction
If endodontic treatment fails, repeated treatment or endodontic surgery is indicated. The method of choice in such situations is canal retreatment. Endodontic surgery is used in cases where canal retreatment did not bring the desired result or was impossible. Nowadays, endodontic surgery makes it possible to save teeth that previously would have had to be removed. New techniques and instruments have contributed to the development of endodontic surgery.
A branch of endodontic surgery is periradicular surgery, which involves a 4-stage system of measures to eliminate chronic infection:
- Surgical removal of the periapical lesion;
- Resection of the apex of the tooth root;
- Preparation of the root stump;
- Retrograde filling.
Both periradicuary surgery and endodontic treatment are aimed at creating conditions for further healing and restoration of the periapical tissues. This is achieved by removing necrotic tissues and their decay products, bacterial infections from the apical canal system and filling the canals. The outcome of periradicular surgery is influenced by technical, biological factors and their combination. Technical factors include the presence of a crown of the tooth and/or the presence of broken instruments in the canal, which may make it difficult to gain access to the infected tooth canal. Previously, periradicular surgery was considered inappropriate due to high risks and unsatisfactory long-term results. Periradicular surgery was used when canal retreatment was not possible as a last resort for saving the tooth (Fig. 1) .
Fig. 1 Traditional periradicular surgery: A – tooth 2.2 before treatment; B – diagnostic radiograph: the root canal is not sealed along the entire length of the root; in the area of the root apex, a focus of bone tissue destruction is determined; C – intraoperative photograph after apex resection and retrograde filling; D – control radiograph after surgery; E – radiograph 2 years after treatment: a decrease in the periapical lesion is determined; F – radiograph 4 years after treatment: there is no focus of bone tissue destruction.
This article reviews the literature on periapical surgery and makes treatment recommendations based on the latest research.
Are the indications for canal retreatment and periapical surgery the same? Surgical endodontics is an important area of endodontic practice. Periapical surgery may be performed after endodontic treatment has failed or when canal retreatment is contraindicated. Surgical intervention is contraindicated in cases of poor-quality root canal filling, although retreatment is possible. In the long term, canal pretreatment is more successful than periapical surgery. According to previous studies, periapical surgery is successful in 50-90% of cases, which is no higher than the success rate of endodontic treatment. Moreover, periapical surgery will be ineffective without high-quality root canal filling. In such situations, as a result of surgical treatment, the source of infection will take a more coronal position, and the opening of the root apex will become a prerequisite for the penetration of a new infection or the development of a recurrent infection. Therefore, canal retreatment is preferable to peripapical surgery unless nonsurgical treatment is not possible or the risk of canal retreatment is not justified.
Clinical and radiological assessment
In daily practice, a number of clinical signs and symptoms are assessed: loss of function, pain on percussion or palpation, tooth mobility, fistula formation, signs of infection, edema, periodontal pocket formation.
Radiographs are necessary to diagnose apical periodontitis. The success of treatment is assessed by the results of clinical (absence of symptoms) and X-ray examination. Persistence of the disease is diagnosed when the focus of infection is identified on an x-ray 4 years after endodontic treatment. Sometimes an X-ray examination is necessary to confirm the absence of periodontitis. However, it is worth considering that an x-ray is a two-dimensional image of a three-dimensional structure. Often the periapical lesion is localized in the cancellous bone and is not detected by X-ray examination. Cone beam computed tomography (CBCT) in many cases revealed a periapical lesion that was not visible on radiographs. The absence of radiological changes in the area of the root apex on the radiograph may be due to the presence of an initial lesion - in such cases, CBCT allows for a more accurate diagnosis. When preparing for surgical treatment, it is important to know the exact size of the periapical lesion and its location in relation to the root and nearby structures. When planning treatment, CBCT is more informative than two-dimensional SIM.
Evaluation of treatment outcome
To assess the condition of the tooth before and after periapical surgery, a thorough history, examination and high-quality x-ray examination are necessary. The outcome of periapical surgery is assessed based on clinical and radiological studies of periapical tissue healing. Classification of periapical tissue healing:
- Complete healing with restoration of the cortical plate;
- Incomplete healing;
- Questionable healing;
- Poor healing.
The criterion for successful treatment is the absence of clinical symptoms and radiologically confirmed healing (complete or incomplete) of the periapical lesion. If healing is questionable or unsatisfactory and clinical signs and symptoms are present, the treatment is considered ineffective.
Modern surgical measures
Periapical surgery includes removal of pathological periapical tissue, resection of the root apex, preparation of the tooth stump, and retrograde filling to seal the root canal. To achieve a predictable outcome in periapical surgery, localization, cleaning, and sealing of the root canal filling are important. Periapical surgery can be performed using modern and traditional methods. Traditional periapial surgery involves resection at a 45° angle and preparation of the tooth stump with a carbide ball bur. The introduction of surgical microscopes, ultrasound equipment and compatible filling materials has made the outcome of periapical surgery more predictable and the success rate of such procedures has now increased. Modern microsurgical techniques allow endodontic surgical procedures to be performed precisely, thereby eliminating the disadvantages of traditional periapical surgery (Figure 2) . According to a US study, microscope use in endodontic procedures increased from 52% to 90% between 1999 and 2007.
Fig. 2 Conducting modern periapical surgery using a microscope: A – teeth 1.1 and 1.2 before treatment, the presence of a fistula tract is clinically determined; B – diagnostic radiograph of tooth 1.2: the instrument is broken in the root canal, a periapical defect of the hard tissue is determined; it was decided to perform periapical surgery on teeth 1.1. and 1.2; C – intraoperative photograph after resection of the root apex and retrograde filling of the MTA; D – radiograph immediately after surgery; E – radiograph 1 year after treatment: incomplete healing of the periapical lesion is observed; F – X-ray after 2 years: complete healing.
Flap design
Various flap shapes have been described in the literature. The design of the flap affects the formation of access, visibility of anatomical structures, reposition and suturing, care and possible complications in the postoperative period. If the shape of the flap does not provide the necessary visibility and does not allow high-quality access, then the prognosis of such treatment is questionable. Flaps can be marginal mucoperiosteal with one (triangular flap) or two (rectangular flap) vertical incisions; submarginal mucoperiosteal (Leubke-Ochsenbein flap) with a horizontal incision within the attached gum, as well as its modifications and semilunar flaps. The availability of so many flap designs necessitates careful selection before performing periapical surgery. The clinical conditions of each patient are different, so individual selection of flap design is necessary.
Root apex resection
Periapical surgery is performed under local anesthesia. After detachment of the mucoperiosteal flap, bone is removed from the root apex to create access to the periapical lesion. Removal of compact and cancellous bone is performed with a bur or a sharp excavator. To prevent dehydration, the surgical field is periodically washed with saline throughout the operation. This approach prevents tissue overheating, which avoids bone necrosis and ensures the formation of new bone in a shorter time. Resection of the root apex involves removing the apex and forming a bevel of the root stump. Using a water-cooled diamond bur, approximately 3 mm of the root from the apex is apically resected with minimal bevel. Kim and Kratchman suggest that at least 3 mm of the apical third of the root must be resected to remove 98% of the apical branches and 93% of the lateral canals. After removal of pathological tissue, bone hemostasis must be achieved.
Formation of a root stump
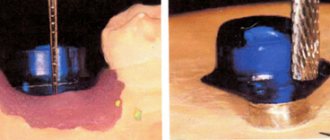
Formation of a root stump is an important procedure in periapical surgery. The root stump is usually treated with a small round bur or reverse-cone bur in a step-down handpiece. The use of ultrasonic tips in the treatment of tooth stumps is currently widespread due to their small size and good handling qualities (Fig. 3). There is minimal or no bevel of the root stump, which reduces the number of exposed dentinal tubules. Stump preparation is less invasive and more accurate, root canal preparation is deeper and provides better retention, and the axis of the prepared root canal coincides with the axis of the unprepared one. The use of ultrasonic instruments reduces the risk of root perforation and provides significant advantages in the treatment of roots with complex anatomy in the presence of a root canal isthmus.
Fig. 3 A – water-cooled ultrasonic tip for retrograde filling; B – ultrasonic tip during preparation.
Materials for retrograde filling
There are many materials for filling root canals. In addition, several new materials are currently being used for periradicular surgery. These are amalgam, ethoxybenzoic acid (Super EBA), temporary restorative material (IRM) and composite. The ideal filling material for retrograde fillings should be biocompatible and bactericidal (or at least bacteriostatic), compatible with adjacent tissues, and provide a good seal. Amalgam was the main filling material until the 90s. Figure 4 shows the result of retrograde root canal filling with amalgam using traditional periapical surgery techniques. However, in recent years, the safety and stability of amalgam as a root canal filling material has been questioned as it has a number of disadvantages, including ion release, mercury toxicity, corrosion and electrolysis, delayed expansion, marginal permeability, and its tendency to stain. fabrics _ Super EBA and IRM performed generally well in animal edge permeability studies and retrospective human studies. A minor drawback of cements based on zinc oxide and eugenol is that their radiopacity is similar to gutta-percha. Ideally, the filling material for retrograde fillings should be easily distinguishable from tooth structure and other filling materials. Torabinejad et al. introduced mineral trioxide aggregate (MTA) as a root end filling material in 1993. It has excellent sealing ability and promotes osteoblast activity. In addition, many studies have shown that it is biocompatible and induces osteo- and odontogenesis. Thus, MTA is the most promising material for use in various clinical procedures, including vital pulp treatment, retrograde dental filling, apexification, root restoration, and furcation perforations. However, long cure times and poor handling characteristics are the main disadvantages of MTA.
Fig. 4 A – diagnostic radiograph of the maxillary incisor after unsuccessful peripaic surgery; B – 15 years after repeated periapical surgery with retrograde filling with amalgam; X-ray shows incomplete periapical healing; C – complete healing 25 years after treatment.
Thus, modern periradicular surgery ensures the healing of periapical lesions that persist after endodontic treatment. Periradicular surgery may be performed after failure of endodontic treatment or when root canal retreatment is contraindicated.
Source: Journal of Oral Science
Translation from English by Ekaterina Vladimirovna Stankevich for the portal
Diagnostics
Diagnosis of an acute inflammatory process of infectious etiology with localization in the hilar region includes a visual examination and radiographic examination. In some cases, thermography may be performed. The dentist assesses the condition of the mucous membrane, hyperemia of the tissue, and changes in tooth color. X-ray examination helps to assess the location of the pus. At the diagnostic stage, the specialist determines the viability of the pulp.
A clinical study allows us to determine the degree of pathology and select the correct endodontic treatment or surgical intervention. If necessary, additional examination methods may be required to determine the condition of the periapical tissues. In each specific case, the treatment method is selected individually depending on the history and clinical examination. The patient’s age, local symptoms, and the presence of general diseases are also taken into account. Additionally, microbiological diagnostics can be performed to identify various types of microbial pathogens.
Decompression technique in the treatment of periapical cysts
D. V. Korotkikh
dental surgeon, chief physician of the Dent and K clinic
Quite often in the daily practice of a dentist there are cases of large periapical defects. Treatment tactics in such cases may vary.
When we make a diagnosis of “periapical cyst” based on a clinical examination and additional research methods, it becomes necessary to choose a treatment method. Since the cause of this phenomenon is odontogenic, there is a need to carry out endodontic treatment of the tooth, and in case of failure, its extraction. However, despite treatment, in the case of large periapical cysts, additional surgical intervention may be required. If this does not happen, an exacerbation of the disease occurs .
There is a need for additional therapeutic effects.
Treatment options in such cases are cystotomy, cystectomy, apex resection, and cyst decompression.
The advantage of using these methods is the ability to minimize the pathological focus, but the disadvantage is the high probability of a large bone defect, which can greatly complicate the patient’s further rehabilitation, especially with the use of implantation.
An alternative treatment option is decompression, which has the advantage of being the most conservative treatment option available; At the same time, maximum preservation of bone structures is achieved, and high clinical success is achieved. The purpose of decompression is to create a permanent drainage, which helps to reduce the size of the cyst and further healing of the pathological focus.
So, decompression.
The indication for decompression is the presence of a large periapical cyst, the affected area exceeding 200 mm2. The final diagnosis can be established only after examining the exudate, however, such a diagnosis can be made quite accurately if the following symptoms are present.
1. The periapical lesion is located in the area of one or more non-vital teeth.
2. The affected area exceeds 200 mm2.
3. The x-ray image will reveal an area of clearing with clear boundaries.
4. When aspirating from the lesion, a straw-yellow liquid is obtained.
Now directly about the decompression technique using the example of a clinical case. A patient came to the clinic with complaints of a fistula in the area of the 36th tooth. From the anamnesis it turned out that 4 years ago the 36th tooth was subjected to endodontic treatment; a month ago, the patient went to the clinic with complaints of pain when biting; an attempt to unfill the canals was unsuccessful, and the tooth was removed. Orthopantomography in the area of the missing 36th tooth revealed a large periapical lesion measuring 11x6 mm (Fig. 1). An objective examination revealed the presence of a fistula in the area of the extracted tooth socket. A decision was made to undergo surgical treatment using decompression techniques.
Rice. 1.
Anesthesia.
After regional anesthesia (Fig. 2), aspiration of the contents of the lesion was performed, during which a straw-yellow liquid with hemorrhagic inclusions was obtained. The nature of the exudate confirms the preliminary diagnosis of periapical cyst.
Rice. 2.
Creation of drainage for decompression.
A decompression tube is created to provide continuous drainage of the pathological focus and repeated irrigation. To do this, you will need a standard infusion system (dropper), which can be purchased at any pharmacy (Fig. 3–4). The advantage of using such a tube is that it has a sufficient diameter, which prevents the formation of various clots; in addition, it can be easily installed and just as easily removed (Fig. 5). One of the ends of the tube, which will be inserted into the pathological focus, should be cut at an angle of 45° (Fig. 6). Since it is inserted all the way, this will facilitate constant drainage of the lesion.
Rice. 3. Fig. 4. Fig. 5. Fig. 6.
How to make it?
A piece of tube is cut, longer than necessary, and one end of it is leaned against a hot spatula (Fig. 7). In this case, a so-called button is formed (Fig. 8). Since the plastic will melt not only outward, but also inward, after the tube has cooled, it makes sense to trim off the excess plastic (Fig. 9).
Rice. 7. Fig. 8. Fig. 9.
Incision.
When making an incision, it is optimal to use incision No. 15 or its mini version Martin No. 15 (Fig. 10). The incision is made down to the level of the bone, and the blade usually penetrates immediately into the defect. In rare cases, perforation of the cortical wall with a ball bur is necessary before insertion of a decompression tube. After the incision, primary drainage occurs and we can observe the release of exudate.
Rice. 10.
Insertion of a decompression tube.
The beveled end of the tube is inserted into the defect using rotating movements, while the tube is directed into the deepest part of the defect until it stops at the rear wall of the lesion (Fig. 11). Moreover, if the tube was too long, part of it will stick out above the mucosa. We need to visually remember the distance that extends above the surface. The tube is removed and the excess is cut off so that it completely enters the defect and the “button” is located on the surface of the mucosa (Fig. 12). No stitches are required.
Rice. eleven.
Rice. 12.
Irrigation of the solution.
A 10 cc syringe with saline solution is inserted into the drainage tube until it stops, and irrigation is carried out (Fig. 13). In this case, the remaining exudate is removed along with the solution. After this, the patient is taught to self-irrigate with saline 3 times a day in combination with normal hygiene. The patient is monitored every week. The course of treatment lasts 2–4 weeks until there is complete absence of discharged exudate from the drainage. During this time, if the causative tooth is preserved, endodontic treatment is carried out.
Rice. 13.
Removing the decompression tube.
After the discharge is complete, the tube is removed. The remaining soft tissue defect heals in a few days to a week.
Some features.
Care should be taken to decompress the area of the maxillary molars due to the presence of the maxillary sinus, which, if perforated, can cause a nasal fistula. Therefore, it makes sense to take panoramic and angled photographs so that the projection of the maxillary sinus does not overlap the pathological focus.
After removal of the decompression tube, the patient is observed every 3 months and X-ray monitoring is carried out, monitoring the restoration of bone in the area of the defect and the reduction in the size of the pathological lesion.
Let's return to the clinical case. The patient had the drainage tube removed after 3 months and was monitored every 4 months. In the image taken after 5 months (Fig. 14), we note a decrease in the boundaries of the defect; no complaints. Image after 8 months: also a decrease in the boundaries of the pathological focus (Fig. 15). A month later, implantation was performed in the area of the 36th tooth. The implant length is 11.5 mm, diameter is 3.75 mm (Fig. 16).
Rice. 14. Fig. 15. Fig. 16.
Let's summarize. Sometimes in clinical practice there are cases when the usual endodontic treatment protocol is insufficient to cure a large periapical defect and additional surgical treatment is required along with it. The method of choice in such situations is decompression, as the most conservative method, requiring minimal invasiveness, causing virtually no complications and maximally preserving bone structures.
Treatment of periapical abscess
Depending on the stage and form of the pathology, the specialist selects a therapeutic or surgical method of treatment. At the initial stage, the canals are usually cleaned, in particular the elimination of pathogenic microflora between the teeth and gums, and the cavity is treated with antibacterial components. Endodontic therapy may include the installation of a temporary filling and the application of an antiseptic dressing with antimicrobial properties in the root canal. Antibiotics may be prescribed to stop the inflammatory process.
High-quality endodontic therapy allows you to eliminate the infectious focus. As inflammation increases, an element of the dental system can be removed. In some cases, the specialist performs appropriate tooth-preserving procedures, for example, hemisection, that is, removal of one of the molar roots.
The opening of an abscess is always performed using anesthesia; discomfort and pain are excluded during high-quality endodontic treatment. After the abscess removal procedure, drug therapy and surface treatment with special bactericidal compounds may be prescribed. The final step is to take an x-ray to ensure complete recovery.
The specialists of the AlphaDent clinic are always ready to help if you have complaints about a periapical abscess without a fistula or with a fistula. Dentists have the necessary knowledge and sufficient experience to provide high-quality endodontic treatment.
Qualified treatment will eliminate the recurrence of the infection that caused the abscess. Timely dental care will help keep your teeth and mouth in good condition. It is recommended to make visits to the dentist for preventive examinations in order to exclude complex endodontic treatment associated with the removal of an abscess.
Periapical dental x-ray
Periapical dental x-rays, along with interproximal x-rays, are targeted x-ray examinations. Simply put, such an x-ray allows you to take an individual “photograph” of a specific tooth, a maximum of two neighboring ones.
This type of diagnosis has another name – root snapshot. It is done in a vertical plane and reflects not only the crown of the tooth, but also the root. Moreover, the image also captures part of the gum, as well as the bone tissue around the root of the tooth and below the apex - the apical part of the root tip.
Thus, on a periapical image you can see not only painful phenomena in the tooth root or periodontal tissues, but also pathological processes occurring in neighboring tissues - abscesses, the formation of cysts and granulomas, and so on.
Thus, a common phenomenon in advanced dental diseases is a periapical abscess. With a progressive inflammatory process, when tissue begins to break down and the pulp dies, an abscess can occur without pain. In such cases, periapical x-ray allows a definitive diagnosis.
Periapical x-rays of teeth are simply necessary for endodontic therapy - root canal treatment. Most often, dentists send patients with suspected pulpitis for such an x-ray - inflammation of soft tissues with neurovascular endings in the tooth cavity. In this case, an image can give a complete picture: what is the source of damage to the root and whether the inflammatory process has spread to neighboring tissues.
When performing pulp removal, it is also important for the dentist to know the individual characteristics of the patient’s root canal structure. Sometimes the diseased root may “hide”, then it will be necessary to take a repeat periapical photograph, while correcting the angle.
You may also be sent for a periapical dental x-ray after treatment. This is necessary for the doctor to make sure that the root canal is sealed completely and tightly. After all, the remaining cavities can lead to new inflammatory processes.
Thus, according to classical methods, during endodontic treatment it is necessary to take at least three periapical images: upon treatment - a diagnostic image, then an x-ray to determine the size of the tooth canal and, finally, a control image.
Root photographs are sometimes prescribed for mechanical dental trauma. If the damage is fresh, then from such an image a dentist can easily diagnose a fracture of the tooth, in particular, its hard structures.
Periapical photographs are also taken for those who plan to install an implant. Such an x-ray is necessary to assess the height of the vertical bone structures in the implantation area. Sometimes, in order for the implant to hold securely, the jawbone is augmented with bone materials.
Unfortunately, periapical dental x-rays alone cannot always provide an accurate picture of the condition of the tooth. Some details in such a photo may be distorted. In particular, periapical images provide a poorly informative image of the crown. From such an image it is not always possible to see the presence of carious cavities, or to understand the relationship between the root and the crown. Therefore, periapical dental x-rays are most often done during initial diagnosis and at the end of treatment to assess the quality of the work.
If necessary, the dentist may require additional bitewing or panoramic X-rays during treatment. But you shouldn’t be afraid of modern X-rays. New generation digital devices make this procedure safe for the health of patients.