Benign growths that appear on the body as a result of exposure to the human papillomavirus (HPV) are called warts. They are neoplasms in the epidermis. Basically, warts on the skin are divided into types according to the type of HPV that caused the appearance on the skin. There are more than 200 genotypes of the virus. It affects not only humans; warts are also found in mammals and some species of birds. Very often, the virus is transmitted to humans from an infected animal. The most common HPV viruses include genotypes 2, 27, 57, 4 and 1. Below we will look at how to diagnose and remove warts, as well as avoid their appearance.
general information
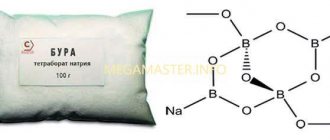
A common wart is a growth on the skin that has a rough surface and protrudes to a certain height above the surface of the epidermis. The color of warts is lighter or darker than the surrounding tissues; on large formations, internal vessels can be seen. The main cause of warts is infection with the human papillomavirus. HPV enters the body through damaged or water-soaked skin. Sometimes infection is possible even if there is no damage to the body. The difficulty of identifying the cause of infection is due to the fact that some warts in adults appear on the body only six months after infection.
HPV mainly affects children and young people. Patients who have a history of chronic skin diseases are susceptible to the problem:
- Psoriasis;
- Dermatitis;
- Eczema, etc.
Patients who have a weakened immune system are also at risk. We are mainly talking about people infected with HIV or those who have undergone organ transplantation. If a patient has problems with immunity, treatment difficulties may arise in the future. In this case, a viral wart most often recurs after removal.
Warts can be found on the skin anywhere on the body. Moreover, most often they are localized in the area of the fingers, elbows, knees, and hands.
Why do warts appear on the lip?
Warts on the lip can appear in men and women at any age. They also often affect children and adolescents. The only reason for the appearance of these benign growths is the papillomavirus. The latter has a high level of contagiousness and is easily transmitted from one person to another through contact in everyday life, as well as during intimate intercourse.
HPV infection with the subsequent appearance of warts on the lips can occur through kissing, unprotected oral sex, as well as through the use of decorative cosmetics (lipsticks, pencils, lip balms) and personal hygiene items shared with an infected person. Sometimes the source of a viral infection can be shared utensils with a sick person. However, such cases of transmission of the virus are rarer than through personal contacts, since the pathogen is not able to live long in an external dry environment.
Another factor that increases the risk of transmitting the virus is the thin, sensitive skin of the lips. In this zone, it is easily damaged, injured, and through abrasions, scratches and cracks, the papillomavirus easily penetrates into deeper layers and begins its pathogenic activity.
The incubation period of HPV ranges from 1 month to several years. Many people are interested in whether warts can appear on the lips immediately after contact with an infected person. The answer to this question is negative. It may take several months for new growths to appear on the skin. And in some cases they never form. It depends on the individual characteristics of the human body.
There are a number of factors that contribute to the transition of HPV from the passive to the active stage:
- Weakened immunity;
- Frequent stress and nervous exhaustion;
- Chronic infectious diseases;
- Hypothermia, colds;
- Sharp hormonal surges;
- Having bad habits;
- Frequent change of sexual partners.
However, even if a person does not develop warts on the lower lip or upper lip, the infected person is a viral danger and can easily infect healthy people.
Types of warts
There are several types of formations. Basically, the division into types of warts is associated with the external aspect, the cause of occurrence and other factors. The following types of warts are distinguished:
- Ordinary (vulgar)
. This type of formation is characterized by an age limitation - predominantly the problem caused by HPV develops in childhood. Warts on the hands, fingers and toes are a common location for the problem. What a wart looks like - a colorless lump the size of a pin's head. Sometimes larger formations are possible. A viral wart rarely manifests itself as a single rash; most often you can find a whole scattering of neoplasms in the affected area. An interesting fact is that if the largest wart in the affected area is correctly removed surgically, the rest will disappear on their own over time. - Flat
. These types of warts mostly appear between the ages of 10 and 25. They are small papules that practically do not stand out above the skin. The surface of the wart is colorless, in some cases the skin in the affected areas acquires a yellowish tint. Viral warts most often appear on the back of the hand, hands, neck and face. - Plantar
. Most often, people with this problem have the question of how to get rid of warts. This is due to the fact that the rashes cause discomfort and pain, especially while walking. They mainly occur on the feet in places that experience excessive friction when walking. The main problem of such a neoplasm is difficulty in self-identification due to its appearance, which is very similar to ordinary plantar calluses. - Seborrheic
. The types of warts in this category are diagnosed in elderly patients. A distinctive feature of education is long-term formation, sometimes it takes several years. Appears as a dark brown small spot on the body, which gradually increases in size, eventually reaching a diameter of 5-6 centimeters. Warts are characterized by the presence of a greasy surface with crusts. Over time, the formation thickens, becomes covered with cracks and darkens significantly. Senile warts occur on closed areas of the body. - Condylomas
. It has a specific place of occurrence - in the area of the perineum and genitals. Warts can also be found in the armpits, under the breasts in women, and in the area of the nasolabial triangle in children. They got their name due to their pointed and lobed structure. Such warts are characterized by multiple distribution in the affected area - the rash is never isolated. The color of the new growth is colorless or pale pink. In some cases, warts begin to rub against clothing or other objects, eventually become damaged, become purple in color, and begin to bleed.
What is the danger of warts on the lip?
Warts on the lip are, first of all, a pronounced cosmetic defect. They are located on a noticeable area of the face and can cause certain psychological discomfort in a person. However, in addition to this, they also pose a certain threat to the patient’s health.
Many people who first encountered this pathology are interested in what to do with warts on the lip. The answer is clear: treat under the supervision of a doctor. These are viral formations, which means that a person is an active carrier of HPV and poses a potential threat to others.
In addition, some warts can be caused by oncogenic strains of papillomavirus. This means that sooner or later the growths can degenerate and become malignant tumors, which require much more serious treatment than simple benign tumors.
There are many factors that can cause malignancy of warts on the lip. First of all, this is injury to growths. In the case of lips, this happens quite easily, since the integrity of thin and delicate skin and neoplasms here can be damaged by teeth, food, hands, and clothing.
Even if an injury to a wart does not lead to its degeneration, it can cause severe bleeding, inflammation, and the addition of an additional infection followed by suppuration.
Also, warts on the lips can grow, interfere with eating, speaking, and cause speech defects. When exposed to frosty air, painful cracks and crusts appear on these formations.
There is also a risk of self-infection. This happens especially often in children, when when the patient frequently touches the wart, he spreads the virus throughout the body. For this reason, pathological growths may appear in other areas.
Causes of warts
A question that worries even those who have not encountered this: why do warts appear? The main method of infection is contact. If you come into contact with a person who already has HPV in their body, there is a high probability that it will be transmitted to you, especially if there are associated factors. The main method of transmission is through handshakes. You can also become infected through common household items, such as bed linen, towels, slippers, etc. There is a high risk of catching the virus in public places - in swimming pools, baths, gyms, etc.
The risk of contracting warts increases under the influence of various unfavorable factors
:
- There are small injured areas on the arms and legs. People who do physical labor at work are at risk. It is extremely difficult for such employees to keep their hands from injury while performing work tasks. Cracks, scratches, and cuts appear on the hands, through which HPV can easily penetrate.
- Decreased protective immune functions of the body. You can determine the problem yourself. Just keep track of how often you get colds throughout the year. An indicator of 4 times or more should cause concern.
- Violent sweating in the hands and feet.
These factors make it easier for the papilloma virus to enter the patient’s body and cause the appearance of warts. The infection is characterized by a long incubation period - the first rash in some cases appears only 1.5 months after infection.
Symptoms
The types of warts also affect the symptoms experienced by an infected patient. Moreover, all types of formations are characterized by a list of identical symptoms:
- The appearance of single or multiple neoplasms. Warts can appear not only on the skin. A rash on the mucous membranes is also possible.
- When pressing on the surface of the formation, painful sensations occur.
- The nail plate becomes deformed, and the periungual fold grows in the affected area.
- Deformation of the feet in case of massive lesions, severe pain.
What do warts on the inside of the lip look like?
Photo of warts on the inside of the lip
A characteristic sign of a wart on the mucous membrane of the lip is quite severe discomfort, which reminds itself every time you eat. At this time, there is a feeling as if something is interfering in the oral cavity, as if there is a foreign body.
This symptom is often accompanied by the periodic appearance of blood, which is associated with a violation of the integrity of the formation as a result of mechanical or chemical damage - hot dishes, cutlery, toothpaste, rinses containing biologically active components.
A wart on the mucous membrane of the lip can reach a size of 0.5-1 cm, and the larger it is, the stronger the discomfort. Usually it is not difficult to recognize by its whitish color that differs from the general background. The surface of the growth is most often smooth, it itself is round, regular in shape and rises several millimeters above the mucous membrane.
The wart on the inside of the lip has a high density, it is hard to the touch, there are no voids inside, which is why, in fact, its shape remains round and regular. Sometimes dentists confuse this formation with stomatitis, which gives similar symptoms.
If a wart on the mucous membrane of the lip is damaged and salt and various spices come into contact with it, a burning sensation may occur. To eliminate it, you will need to rinse your mouth thoroughly with clean warm water. A growth with compromised integrity is not protected from infections that can freely penetrate inside. As a result, inflammation and irritation of the mucous membrane will become possible.
- See also what a flat wart on the lip looks like
Types of warts and specific symptoms:
- Molluscum contagiosum
. Localization - on the body or in the genital area. There are depressed areas on the surface. If you press on the wart, a mushy substance may begin to ooze. - Nevi
. May be a congenital problem, raised significantly above the surface of the skin. Characterized by a dark brown color, as well as the presence of hair. - Basalioma
. It has a crust on the surface; if it is removed intentionally or accidentally, bleeding begins.
Diagnostics
The differential diagnosis is based on the clinical picture of the specific type of neoplasm, as well as on the study of the anamnesis. The size of the papule, the rate at which it increases in size, the number of formations and other factors are taken into account.
To make a final diagnosis, the patient may be referred for histological examination.
If the appearance of warts is planned to be excluded using destructive methods, it is first important to be tested for HIV, hepatitis and syphilis.
Treatment methods for warts
Treatment of warts does not guarantee 100% results. Even a healed wart may reappear in the future. Removal of warts only in 70% of cases does not result in relapse after a while. The behavior of warts is unpredictable. Treatment of warts may often not bring any results, and in some cases the problem resolves on its own without any intervention at all.
Treatment of warts has two goals - destruction of the viral tumor, improving the quality of life for the patient. Indications for starting treatment are the clinical manifestation of the problem. The most common method is based on the destruction of education. However, there is no guarantee that after complete healing of the tissue in the affected area, the problem will not reappear. Most often, relapses are typical for neoplasms of a large area - from two centimeters. Warts on the fingers and in the area of the periungual plate are also considered problematic.
Warts are treated using several methods. The choice of a specific method for treating warts directly depends on the type of lesion, its prevalence, location and other factors. All interventions are carried out without mandatory hospitalization of patients.
Treatment of warts with physical destructive methods
- Electrocoagulation
. The affected area is numbed, then an electric current is applied to the wart using a needle tip. The method allows you to remove the wart layer by layer. - Cryodestruction
. Freezing the surface of the tumor using liquid nitrogen. The duration of exposure is from 1 to 5 minutes. A repeat procedure is required a week after the first. - Laser exposure
. Depending on the size of the wart, laser contact on the area lasts from a few seconds to 2-3 minutes. The crust formed on the surface is cut with scissors, then the bottom of the wart is re-exposed using a laser. The disadvantage of this method is that a wound surface is formed, which the patient needs to treat independently. The affected area should not be re-injured, and it is also important to avoid getting wet. The scab that appears on the surface is removed by the patient. - Radiosurgery
. The affected area is exposed to electromagnetic waves. As a result of this effect, the surface of the wart is dissected without mechanical force. The intervention is carried out with local anesthesia of the affected area. Most often, a 2% lidocaine solution is administered.
Treatment of warts with chemical methods
- Zinc solution. Before removing the wart, the doctor treats the surface with alcohol to disinfect and facilitate penetration of the composition. The solution is applied using a spatula or capillary, it all depends on the size of the wart. The duration of application is until the neoplasm changes its color. The procedure is repeated after 1-2 weeks. For ordinary warts, 1-2 procedures are most often sufficient; if we are talking about plantar warts, applying the solution may require three times. The wart tissue undergoes mummification under the influence of the composition, in order to increase the effectiveness of the effect; dead areas are removed before new application. During the periods between procedures, the patient is not recommended to wet the area. The surface is also subjected to antiseptic treatment using alcohol-free compounds.
- Composition based on nitric, acetic, oxalic, lactic acid and sodium nitrate trihydrate. In this method, the surface of the wart is also pre-degreased. It is important to apply the composition exclusively to the affected areas, without touching healthy tissue. The product turns tumors on the skin yellow and on mucous membranes white. The patient is required to return for an examination 3-5 days after treatment. The method is not suitable for warts that exceed 5 centimeters in diameter.
How to remove warts in childhood? Treatment is possible only with the help of destructive methods in order to avoid possible toxic effects on a fragile organism.
It is important to remember that it is easier to prevent the appearance of warts than to subsequently treat them in a clinic. There are several rules of prevention:
- Maintain personal hygiene, wash hands after visiting public places, use only personal items.
- If damage appears on the skin of the hands or feet, they must be treated with iodine or brilliant green until they heal. It is also advisable to limit contact with HPV carriers.
- Normalization of nutrition. The body must receive all the elements necessary for the normal development of the body. It is also important to remove stress from your daily life as much as possible.
Warts and molluscum contagiosum in pediatric practice
Warts and molluscum contagiosum are two viral dermatoses that are common in children. They usually do not present diagnostic problems, but treatment decisions may be difficult when there are multiple lesions and the child is young.
Molluscus contagiosum
Pathogenesis
Molluscum contagiosum is a benign skin tumor caused by viruses of the Proxivirus family, a bulk DNA virus of the Molluscipoxivirus subspecies. Virus synthesis occurs in keratinocytes of the epidermis. The viral genome is encoded for proteins capable of disrupting the physiological mechanisms of the host, one of the factors of which is the inhibition of T lymphocyte activation. The absence of immune cells in skin lesions explains the immune tolerance that favors this infectious agent during human infection.
Epidemiology
Infection with molluscum contagiosum is a purely human affair. Contamination most often occurs directly, but can also be indirect through contaminated objects. The presence of skin lesions may favor virus inoculation. This disease is sporadic or endemic, most often found in children's institutions. Crowding, skin-to-skin contact and a humid atmosphere, especially in swimming pools, are factors favoring dissemination, but there are also individual differences in the risk of infection. The incubation period after exposure varies from several weeks to several months, with an average period of two to seven weeks. The infection then spreads by autoinoculation, with each lesion developing over several weeks.
Molluscum contagiosum occurs quite often if there is a cellular immune deficiency, acquired or congenital, or with atypical dermatitis.
Clinic
According to the type of the most common manifestation, molluscum contagiosum appears as closed papules, in the form of pearls, hemispherical, five millimeters in diameter and with a sunken center. Pressure on the center produces a characteristic whitish discharge. Lesions are usually multiple, from several elements to several hundred; they predominate on the face and torso.
There are atypical forms. Also, molluscum contagiosum can be very small, difficult to see, or, conversely, “giant” up to a centimeter in diameter. Sometimes the umbilical depression may be absent. Inflammatory lesions sometimes take on a chaotic appearance.
Particular profuse forms have been described in atopic children, possibly facilitated by dermatocorticoids, and in immunodeficient children: with leukemia, receiving chemotherapy or in persons affected by HIV+. Molluscum contagiosum is considered an opportunistic lesion during SCID or appears to be more numerous and voluminous the deeper the immunosuppression.
Complications are rare. Inflammation ranges from simple erythema to true abscesses centered around the mollusk, corresponding to an aseptic process with a favorable course, but which may require an incision for isolation. Bacterial superinfection is possible, sometimes leaving permanent scars. An eczematous reaction adjacent to molluscum contagiosum is quite common (in approximately 10% of cases), probably secondary to a delayed delayed-type reaction directed against the Proxivirus. It often indicates regression.
Diagnostics
Clinical diagnosis. Most often it is quite simple, but requires a thorough examination to identify typical lesions. None of the paraclinical studies are helpful except in cases of clinical doubt. In these cases, histological examination is typically performed to identify intracytoplasmic eosinophilic inclusions in keratinocytes.
Treatment
Curettage
A blunt or sharp curette is used (Curette Siefel), which requires confident and precise movement. Pre-treatment with Emla anesthetic cream for an hour under a transparent film eliminates the painful “brake” of this method. Treatment often requires many sessions, depending on the number of lesions, the child's tolerance and the dose of Elma cream applied per session (depending on the weight and age of the child). In practice, based on one session per month, cure usually occurs within three to four months.
Added to this method is the simple expression of the contents of molluscum contagiosum, which often makes it possible to get rid of this lesion. In fact, minimal trauma and, a fortiori, secondary lesions during curettage, even incomplete, expose the lesions to the inflammatory process causing their disappearance.
Chemotherapy treatments are varied
Its principle is based on the induction of local inflammation, or slight superficial ulceration, by applying a caustic solution once twice a day to each molluscum contagiosum. While these treatments are sometimes effective, they are often irritating, making them difficult to use long-term. The substances used are very diverse and vary depending on fashion and schools.
Other methods
Cryotherapy and electrocautery are gradually being abandoned, as they can cause permanent scars. Immunomodulation-type treatments, such as tuberculin application, have been proposed in children previously vaccinated with BCG or isoprinosine, but their effectiveness has not been confirmed.
Molluscum contagiosum is a common pathology in children. Its benign nature orients in the direction of a rational therapeutic approach: less traumatic and less painful. In any case, based on epidemiological data (auto-inoculation, contagiousness), active management is preferred: curettage of the lesion under Elma protection in several sessions.
Special cases
In an immunosuppressed child, where molluscum contagiosum is especially profuse, the appointment of anti-HIV therapy or the administration of cidofovir (a DNA polymerase inhibitor active in the effect on cytomegalovirus) is of real interest, both in relation to the restoration of cellular immunity and in its direct antiviral effect. Currently, cidofovir is being studied for topical use.
A problem arises when molluscum contagiosum is located on eczema plaques. It is certain that treatment of eczema with dermatocorticoids favors its spread, but eczema itself contributes to its persistence and chronicity. In practice, local corticotherapy is completely useful in cases of severe eczema and does not appear to favor the proliferation of molluscum contagiosum.
WARTS
Warts are benign tumors associated with skin infection by the papilloma virus (PVH). They are extremely common in children, quite profuse, and are favored by the presence of autoinoculation. Their ubiquitous localization often complicates the choice of therapy.
Physiopathology
Human papillomavirus is a ubiquitous virus that infects humans among a large number of mammals. It has a special tropism for keratinocytes of the Malpighian epithelium. It belongs to the Papovaviridae, DNA bicathenaire viruses. These viruses are very resistant in the external environment and are not destroyed by cold, drying and detergents. . . Study of their genome revealed genes involved in viral DNA replication, proliferation and cellular immortalization. There are more than 70 human papillomaviruses, classified depending on the presence of oncogenic risk, their genotype and their tropism for the skin or mucous membranes.
Epidemiology
The incubation period is little known, ranging from a few weeks to more than a year. The prevalence of cutaneous warts is estimated at 10% of the general population, with a clear increase over two to three decades. The most common victims are school-age children and young adults, with a peak incidence at 15 years of age.
Transmission is direct or mediated by infected squamous epithelium. It can be cutaneous and mucous, transmitted sexually or not, rarely maternal-fetal, and is favored by microtraumas. Favorable factors are considered: frequent visits to swimming pools, more than once a month, a humid environment, antecedents of atopy or genetic diseases such as Wiskott-Aldrich syndrome.
Clinical forms
The clinical aspects of human papillomavirus infection are extremely diverse. Vulgar warts are most common among children. We are talking about epidermal, papillomatous and keratic tumors, the size of which varies from one to several millimeters. Their number varies from several to several dozen, sometimes merging into profuse keratized spaces. These common warts vulgaris, often located on the dorsal surface of the hands and fingers, are mainly associated with HPV-2.
Peri-ungual and subungual warts
Caused by PVH-2, more rarely PVH-1, they are located under the free distal or lateral edge and at the level of the nail matrix. They are profuse and recur in the child onychophage and are often painful. Onychodystrophy with damage to the matrix may be irreversible if treatment is too aggressive. The child's periungual (epiloia), exostosis, or other subunval tumor is removed. The disappearance of dermatoglyphs from the skin is a good argument in favor of a wart.
Filiform warts
Caused by PVH-2, they are localized at the level of the face, where they occupy a periorificial position, like perinarinal or peribuccal warts inoculated by licking, or at the level of the skin of the scalp and at the level of the neck of adolescents due to the fact of auto-inoculation during shaving.
Flat warts
These are small papules on a flat surface, protruding several millimeters, pink or light yellow, located on the face, dorsal surfaces of the hands and fingers. Their arrangement is linear or merging panels. They are associated with human papillomavirus types 3, 10 and 28; they are more common in immunocompromised patients. The profuse form makes one look for epidermodysplasia versiformis. The differential diagnosis of this type of wart should include lichen planus in pruriginous lesions and cephalic histiocytosis.
Warts on the soles
They are a common reason for seeking medical attention, either because they are painful and/or cause functional limitations or because of pressure from the school environment, particularly when the child is involved in strenuous sports activities, such as in the swimming pool. Human papillomavirus manifests itself at the level of the soles with two very different clinical pictures: myrmecies and mosaic warts. Both of these patterns rarely occur together in the same patient.
La myrmecies
Association with PVH-1 is most common. This is an endophytic wart, usually solitary, deep and painful due to the presence of pronounced hyperkeratosis. The keratized surface is dotted with black dots, which are thrombosed microcapillaries or inclusions of foreign bodies.
Mosaic warts
Less common, they are associated with PVH-2. They are located superficially, painless, multiple and merging into an extensive keratized surface. Spontaneous regression is the rule and occurs more quickly in children than in adults.
Special cases
Epidermodysplasia verrusiformis is a rare autosomal recessive genodermatosis. It is characterized by a pathological predisposition to certain types of human papillomavirus, usually pathogenic. They manifest themselves in childhood with the profusion of flat warts associated with the macula, comparable to those in pityriasis versicolor. The prognosis depends on the carcinogenic nature of individual human papillomaviruses.
In immunodeficient patients, clinical pictures are described that resemble verrusiform epidermodysplasia due to the presence of vulgar warts, especially profuse and recurrent ones, often atypical in clinical terms.
Anogenital candillomas are infections associated with human papilloma viruses with tropism for mucous membranes. They are rare in children, but their frequency increases in parallel with the frequency of condylomas acumines in adults. Anogenital warts in children are caused either by human papillomavirus types 6 and 11, or by the common human papillomavirus type 2. Although sexual transmission exists, many studies show that most often we are talking about innocent auto- or hetero- inoculation through persons dealing with children. However, in the context of abuse in an “atypical” family environment, vigilance is the rule.
Diagnostics
Clinical diagnosis. If there is any doubt, histological examination confirms viral papilloma by identifying a specific cytopathogenic effect on keratinocytes (koilocite). Virological diagnosis by molecular analysis of viral DNA is not routinely performed. PCR is the most sensitive method for determining the type of human papillomavirus and is used to identify oncogenic viruses or when there is doubt about the presence of sexual abuse.
Treatment
The most effective treatment is a host immune response induced by altering the cellular response. In an immunocompetent child, spontaneous regression rates of about 40-50% explain why therapeutic abstinence is part of therapeutic proposals.
The basis of medical treatment is to destroy the infected cells. All types of treatments used for infections with human papillomaviruses address only visible lesions, but none of them eliminates the virus that caused them. The remedies are numerous, but no study has shown the superiority of one type of treatment over another.
Physical treatment
They are represented by surgical excision, electrotherapy, CO2 laser and cryotherapy. With the exception of cryotherapy, all these methods require local anesthesia, which limits their indications.
Cryotherapy
It consists of applying liquid nitrogen to the wart using a Cotton-Tige or cryostat. The white cooling halo should remain for 15 to 30 seconds. The application is carried out every three to four weeks and recovery usually occurs within four to six months. The disadvantage of this method is pain, which limits its use in children. A recent study showed that there was no immediate or delayed effect on pain with local anesthetics such as Elma, given one hour before cryotherapy.
Chemical treatments
They are quite numerous. Keratolytics combine topical preparations based on salicylic acid and/or acetic acid, urea and glutaraldehyde. Local chemotherapy drugs including bleomycin injected into lesions, 5-fluorouracil in lipstick or podophylline have questionable effectiveness in adults and are extremely rarely used in children.
Pharmaceuticals
Currently, they are more widely used than mainline drugs. Mostly 10-60% acetylsalicylic acid is used alone, or in association with lactic acid. It is necessary to protect the skin around the wart. Colored rubber bands impregnated with salicylated petroleum jelly 15% (Transvercid) represent an interesting alternative for the child to conventional colloids, since there is a preliminary experience of pain. This should be systematically associated with weekly manual picking.
Special cases of plantar warts
Approximately 95% of plantar warts heal spontaneously within two to five years, without pain and without scarring, myrmecies more quickly than mosaic warts. In addition, children heal spontaneously much faster than adults and their horny bed is less dense, which facilitates the implementation of progressive techniques.
If the wart does not cause any functional limitations, then the natural evolution of warts and the likely time frame for spontaneous healing can be simply explained to parents. If there is a limitation, then it is most likely associated with hyperkeratosis than with the wart itself and treatment consists of mechanical pickling and/or chemical (salicylated petroleum jelly 20-50%, treated with urea 30%) under an occlusive adhesive plaster, accompanied by weekly manual pickling with a file or rasp , pumice. The adjacent skin should be protected with a bandage or varnish. Glutaraldehyde (Verutal) may also be used, but should not be associated with other treatments, especially cryotherapy due to the risk of skin necrosis.
When localized on the sole, physical treatment, cryotherapy and fortiori CO2 laser are used less and less due to the presence of pain, the functional impairment they cause and possible residual scars.
CONCLUSION
Molluscum contagiosum, like warts, are benign viral tumors that spontaneously regress over time. Contagiousness, social and school pressure, and unsightly appearance often require active treatment. In fact, it often happens that the child is deprived of the right to use the pool because of this or is asked to consult a dermatologist regarding radical treatment. In any case, in these contexts, no restrictions on the school, including all activities associated with it, are justified in these two cases.
No school restrictions if you have warts or molluscum contagiosum.
Source:
- P.Schoenlaub, P.Plantin/ Verrures et molluscums contagiosums: mise au point pratique/ Arch Pediatr ; 7; 1103-10
- Translation from French - Yu.M. Bogdanov, Department of Pediatrics, Physics and Training Faculty of the Northern Medical University, Arkhangelsk
The article was published on the website https://www.medafarm.ru