Congenital pathology of the lip, in which the soft tissues do not fuse, is usually colloquially called a “cleft lip.” This name is given because the upper lip of hares consists of two halves that are not fused together.
The nature of the defect is the same as that of a cleft palate. But in the case of the latter, not only the soft tissues do not fuse, but also the bones of the palate. In half of the cases, facial tissues are not affected, and there is no cosmetic defect. In this case, it will only be a “cleft palate”.
Cleft palate and lip are scientifically called cheiloschisis. This congenital pathology occurs in the womb, usually in the first trimester of pregnancy. Under the influence of harmful factors, the development of the lip, palate and alveolar process is disrupted.
Children with a cleft lip may have not only external defects, but also serious deformation of the skull bones. Because of this, difficulties arise with nutrition and speech. But the pathology causes only physical problems - the intellect and psyche of such children are in perfect order.
Cleft lip without cleft palate is a milder pathology, since only soft tissue is affected and the bones are not deformed.
What is a cleft lip
Cleft palate and lip appear in a baby in the first months of development. This is when the jaw and face are formed. Normally, by the 11th week, the bones of the fetus's palate fuse, and then the soft palate forms. In 2 - 3 months, the upper lip is also formed, when the processes of the upper jaw and the median nasal process are finally fused.
The first months of pregnancy are the most important for the formation of the correct anatomy of the child. If during this period the embryo is influenced by negative factors from the outside, a failure may occur in the process of formation of bones and soft tissues, and a cleft lip may occur. The process is also influenced by genetic factors.
Photo: shutterstock.com
Causes of cleft lip in children
Cleft lip develops under the influence of “internal” and “external” causes. Hereditary factors, inferiority of germ cells, and early abortions can affect the development of the fetus.
No less dangerous are infections that a woman suffers in early pregnancy.
Chemicals, radiation, maternal consumption of drugs, alcohol or smoking have a detrimental effect on intrauterine development. Poor nutrition, vitamin deficiency, cold and heat, abdominal injuries, fetal hypoxia also affect the formation of the fetus.
The causes of the pathology are still being studied. The main ones are listed above, but in rare cases, cleft lip develops after birth. After trauma, infection, or removal of tumors, the palate and lips may be damaged.
Symptoms of cleft lip in children
A baby's cleft lip is usually detected before birth, on an ultrasound after the 12th week of pregnancy. Unfortunately, even with such early detection, nothing can be done before the baby arrives.
After birth, the baby has deformed lips, a nose, and possibly a cleft palate. The form and degree of pathology vary in severity - clefts are possible even on both sides. But more common is unilateral cleft palate and lip.
A baby with such a defect does not latch on well, often chokes, and breathes shallowly. He is prone to nasopharyngeal and ear infections due to frequent reflux of food through the cleft in this area.
Treatment of cleft lip in children
It is important to understand that a cleft lip is often more than just a cosmetic problem. She will have to be treated in any case, and at a very early age. Otherwise, the child will not be able to suck, swallow food correctly, and sometimes even feeding through a tube is required.
Without treatment of the defect, the bite is formed incorrectly and speech is impaired. A cleft palate disrupts the timbre of the voice; children pronounce sounds poorly and speak “through the nose.” Even a cleft in only soft tissues will interfere with speech production. Frequent inflammation in the nasal cavity and ears due to reflux of food leads to hearing loss.
After the diagnosis is made, a decision is made about surgery - there are no other ways to help the child. The age at which the baby will be operated on is determined by the doctor. If the defect is too dangerous, the first operation is possible in the first month of life. Usually it is postponed until 5 - 6 months.
Treatment consists of several stages, so surgery alone will not work. Before the age of 3, the baby will have to undergo 2 to 6 operations. But as a result, only a barely noticeable scar and possibly slight asymmetry of the lips will remain. All other problems will be behind you.
Diagnostics
The first diagnosis of cleft lip is carried out inside the womb using ultrasound. After the birth of such a child, a doctor examines the severity of the pathology. It determines how much the defect prevents the baby from eating, and whether there are breathing problems.
They resort to the help of other specialists: otolaryngologist, dentist, infectious disease specialist. Next, general blood and urine tests, blood biochemistry, and x-rays of the maxillofacial area are prescribed. The baby's reaction to sounds and smells is checked - this is how hearing, smell, and facial expressions are assessed.
Photo: @mart.production, pexels.com
Modern methods of treatment
Plastic surgery is used to eliminate the cleft lip defect. Doctors of various profiles will be involved in multi-stage treatment. Before surgery, the child often wears an obturator, a device that serves as a barrier between the nasal and oral cavities. This prevents the reflux of food, helps to breathe and talk normally.
For a small defect, isolated cheiloplasty is used - the skin, tissue, muscle and mucous layers of the lips are sewn together. If the nose is affected, rhinocheiloplasty is performed, correcting the nasal cartilage. Rhinognathocheiloplasty forms the muscular frame of the mouth area.
Cleft palate is treated with uranoplasty. Unlike previous operations, it is performed quite late - by 3 or even 5 years. Early intervention may harm jaw growth.
Additional reconstructive surgeries are needed to remove scars and improve speech and aesthetics.
In addition to surgical treatment, the child needs the help of a speech therapist, since it is more difficult for such children to pronounce sounds correctly than for others. The otolaryngologist makes sure that the baby’s hearing is not damaged and breathing is normal. If teeth grow abnormally, the orthodontist installs braces.
Constant oxygen deprivation due to shallow breathing, poor weight gain and frequent infections can lead to a sickly appearance and stunted growth.
The help of a psychologist will be no less important, since due to their characteristics, children with a cleft lip experience difficulties in adaptation. Despite the fact that the mind of such children is in perfect order, they may still lag behind in development. Due to psychological problems, reluctance to study due to bullying by peers, problems arise in learning. Difficulties in pronouncing words can also interfere with a full life. Therefore, it is better to complete all stages of treatment before school age.
Cleft lip - symptoms and treatment
A multidisciplinary team is involved in the treatment of patients with clefts, since even a well-performed operation does not guarantee the absence of other complaints. Team members: pediatrician, dentist, orthodontist, plastic or maxillofacial surgeon, nutritionist, speech therapist, ENT, ophthalmologist and neuropsychiatrist. The ENT doctor works to prevent concomitant pathology of the middle ear, which often develops with clefts, and, if present, treats it. Orthodontists make orthodontic structures (obturators), thanks to which the child can eat normally. Obturators are prosthetic devices that close a cleft and can be used for children of all age groups.
Dentists Hubener D.V. and Liu J.R. classified means for orthopedic treatment of the cleft into preoperative and postoperative, active and passive, extraoral and intraoral [14]. There was a long debate about how these methods affect the growth of facial bones and whether they worsen the prognosis, until naso-alveolar plates were invented, which were made first of acrylic, then of rubber. The plates closed the cleft, and the child could suck normally; in addition, the pressure of the plate helped support the wings of the deformed nose, improved the ratio of the lengths of the columella, the cleft parts of the lip, and gently moved the triangular bone [11].
Many types of surgical treatment have been described for the treatment of cleft lip and palate, although the possibility of performing such operations has arisen relatively recently.
Since early times, people have tried to find a way to get rid of this defect. They tried to connect the crevice with sharp sticks, then they used metal needles that were wrapped with thread. Due to the lack of means for pain relief, the operations were primitive and ineffective. Since the 16th century, they have tried to use special caps for external impact on the cleft, trying to cause the edges to stick together. The protruded premaxillary bone in the case of bilateral clefts was simply cut off, which most often led to worsening deformation of the midface.
Surgery to correct a cleft lip is called cheiloplasty . With the beginning of surgical corrections, cheiloplasty methods began to change and improve. The first operations were perceived as a miracle; they created a linear incision. Over time, they began to make incisions of increasingly complex configurations in order to correct associated deformities and prevent the appearance of new ones. Now, in order to correct the complex deformity that occurs in the midface area and create conditions for the normal development of the facial part of the skull, it is necessary that the operation fulfill the following conditions:
- Was safe for young children.
- I corrected the maximum in each specific case in 1 stage.
- Formed the correct line of the red border and Cupid's bow.
- Correct formation of the filtrum is desirable.
- Provided sufficient depth of the vestibule of the oral cavity.
- It eliminated improper attachment of the fibers of the orbicularis oris muscle and created a continuous layer of muscle, which will help in the correct formation of the bones of the facial skull.
- Lengthened the short medial part of the cleft lip.
- Corrected the shape and position of the nasal cartilage.
In 1938 A.A. Limberg described and in 1952 expanded the method of unilateral cheiloplasty. This method became the leading method in the USSR for a long time, because in most cases it made it possible to correct the concomitant deformation of the nasal wing on the cleft side.
In 1952, Tennyson C.W. in the USA and in 1955 Obukhova L.M. in the USSR they described a cheiloplasty method of a more complex configuration. The method is still used today; in addition, cheilorhinoplasties have been developed on its basis to reduce the likelihood of developing associated deformities. The techniques are interesting primarily for their historical significance: for the first time, complex-shaped incisions began to be made and the lip was lengthened. However, lengthening the lip on the cleft side was also a limiting factor because it itself created a recognizable deformity. Techniques are now being used to solve this problem.
The most used technique for suturing unilateral clefts in the world now is the Millard technique and its modifications. In our country this is a modification of I.A. Kozina.
Millard cheiloplasty involves simultaneous restoration of the continuity of the upper lip and correction of the nasal cartilage. On the medial fragment of the upper lip, point 1 is marked - the center of the cupid's bow. On the healthy half of Cupid's bow, look for limiting point 2 (apex of the arc), located approximately 2-4 mm from the midline. This distance is laid on a white roller on the shortened side, obtaining point 3. The length of the lateral fragment of the lip on the healthy side is measured between the limiting point 2 and the commissure of the mouth (point 6). The resulting distance (approximately 20 mm) is laid on a white roller on the damaged side of the commissure (point 7) and a limiting point 8 is obtained. Point 8 will be the top of the cupid's bow on this side; it should connect to point 3 on the medial segment. Measure the distance from point 2 to the base of the nasal wing of the healthy side (point 4), the same distance is set aside from point 8 to the base of the nasal wing of the affected side (point 10). On the shortened side, from the middle of the base of the columella (point 5) to point 3, an arcuate rotational incision is made, symmetrical to the arc of the philtrum on the healthy side. If necessary, extend the incision to point x (reverse incision towards the healthy philtrum). On the lateral (side) fragment, according to the length of the section x-5-3, point 9 is found medially from the base of the flattened wing of the nose. Modifications are mainly used to expand the intervention to the nose, with secondary cheiloplasty, hidden and incomplete clefts.
The advantages of this method of primary cheiloplasty:
- maximum tissue preservation;
- moving all elements of the upper lip to the correct position;
- formation of the bottom of the vestibule of the nasal cavity and the deep vestibule of the mouth.
The method simultaneously corrects the position of the deformed wing of the nose, and some modifications are supplemented with one-stage rhinoplasty. In addition, the arcuate scar is hardly noticeable and can be used for corrective cheiloplasty in adulthood.
Closure of a bilateral cleft can be one-stage or two-stage. This depends on the volume of the cleft, the experience and confidence of the surgeon in his techniques. Each option has its pros and cons, but it is believed that with the help of one-step closure of the cleft, it is more likely to fully create a sphincter of the orbicularis oris muscle.
Sometimes it is practiced to connect the edges of the cleft. This is not a full-fledged cheiloplasty, but only the transfer of a complete cleft into an incomplete one in the expectation that the pressure of the connected part of the lip will have an orthopedic effect on the edges of the cleft, which will lead to their convergence. In most Western countries, the Millard method of cheiloplasty remains the leading one [12].
With a two-stage closure, one side of the cleft is first closed using any method, and after some time the other side is closed.
The debate about at what age to perform surgery still continues to this day. There are those who urge treatment to be carried out as early as possible. Even operations on the fetus are offered, due to the lack of scarring in the prenatal period. Many insist on surgery in the first days and even hours of life. On the one hand, there are advantages to this (parents are not afraid of the child’s appearance, there are no intra-family conflicts, there are no problems with nutrition), but there are also disadvantages (imperfect thermoregulation of newborns, high sensitivity to blood loss, very small anatomical basis). In the 60s of the last century, a large-scale analysis of the results of operations performed in the maternity hospital in the first days of life was carried out. The result showed in almost all children much worse results than in patients who were operated on as adults [1]. N.M. Mikhelson, in one of the oldest Russian manuals on plastic surgery, advises performing the operation at the age of 5-6 months, when the child is sufficiently strong and developed. He believed that cosmetic success was easier to achieve during this period. It is also described that such operations should be performed under local anesthesia, due to the danger of anesthesia [10]. Now there are safe drugs for anesthesia, so it is difficult to imagine performing an operation on young children under local anesthesia. Most surgeons believe that primary cheiloplasty is indicated at the age of 6-12 months.
The extent of the operation depends on the degree of the cleft. Many modern authors believe that in case of a complete cleft, primary cheiloplasty (when only the cleft is sutured) should be used in exceptional cases, since it does not correct the condition of the nose. Therefore, now the primary rhinocheiloplasty technique should be used, when, together with suturing the cleft, the position of the alar cartilages, septum, and vomer is corrected. The quality of the primary operation should be maximum, since repeated corrections are more difficult to perform in conditions of soft tissue deficiency and extensive scarring [4].
Complications during surgery
When performing surgery, the danger is aspiration (inhalation by the patient) of blood and mucus, which can cause asphyxia. To prevent this, you should prevent bleeding and carefully suck out the contents of the oral cavity (blood, saliva, mucus). Possible complications also include collapse, shock, laryngospasm and other conditions.
Mortality on the operating table and shortly after surgery is usually associated with improper selection of patients. You cannot operate on malnourished and premature children, those who, even before surgery, suffer from inflammatory conditions of the respiratory system, hearing, and decompensated abnormalities in the development of the brain, heart, and blood vessels. Also, surgery is prohibited in the presence of thymic-lymphatic status (enlarged thymus). The possibility of surgery should be decided together with the pediatrician.
Complications after surgery
In the coming days after surgery, stenosis (narrowing) of the larynx, bronchitis, pneumonia, urinary retention and other somatic complications may occur, the prevention and treatment of which should be carried out with the participation of a pediatrician. The most common local early complication is suture dehiscence, which is usually associated with technical errors in the operation:
- excision of a significant amount of tissue in the area of the edges of the cleft;
- insufficient tissue preparation;
- incorrect layer-by-layer suturing of the wound;
- tissue tension in the wound area, inflammation and swelling in the operation area.
Sometimes the sutures come apart due to injury (a child’s fall, an accidental blow to a hard object), infection, or the child’s illness with ARVI, rhinitis and other inflammatory pathologies. If the sutures diverge, the issue of applying secondary sutures is decided according to the patient’s condition.
When examining a patient who has undergone surgery, the height of the upper lip, the degree of its deformation, the depth of the vestibule of the mouth and its tightness (the presence of oronasal anastomoses and palate defects) are checked. You should pay attention to lip mobility, phonation, and changes in the structure of the dental system. The integrity of the orbicularis oris muscle can be tested by having the patient stretch his lips into a smile and purse his lips into a tube [1].
Severe psychological trauma is caused by scar changes after an unsuccessful first operation. One of the most unpleasant long-term complications of cheilorhinoplasty is deformation of the upper lip, nose and upper jaw, which can occur for various reasons [9].
After surgery, the patient may have a lack of soft tissue of the upper lip, its lengthening or shortening, stiffness due to extensive scarring, or an aesthetic defect. Alveolar cleft leads to the formation of crowding of teeth, the growth of dystopic (improperly positioned) and supernumerary (extra) teeth, which can support inflammation or, due to their location, form an oronasal fistula (an opening between the oral cavity and the nasal cavity). In general, such a fistula can also be due to excessive tension, cutting sutures, a defect in suturing, etc. Through it, the discharge of liquid part of food into the nasal cavity can persist, which in turn helps to maintain chronic rhinitis, sinusitis, etc.
Possible insufficiency of the muscle ring of the orbicularis oris muscle, which develops with defects in muscle alignment or insufficient separation of muscle fibers from the pyriform opening. Deformation of the vestibule of the mouth in the form of its flattening complicates further orthodontic treatment, which is so necessary for patients, and aggravates the retrusion of the midface (backward displacement). Deformations of the external nose and septum lead to a significant deterioration in the aesthetic result and disruption of nasal breathing, and breathing through the mouth in such patients aggravates the deformation of the facial skeleton.
Prevention of cleft lip in children at home
It is quite difficult to avoid such a problem. If such a pathology has been observed in the family, you can consult a geneticist to find out the likelihood of having a baby with a cleft lip.
It is important to take special care of yourself in the first weeks of pregnancy - avoid infections, injuries, and eat well. As a preventative measure, pregnant women take folic acid.
It is necessary to detect the problem as early as possible, even in the womb. Since cleft palate and lip may cause additional complications during childbirth, your doctor should be aware. During childbirth, the risk of amniotic fluid entering the baby's respiratory tract increases.
After the birth of a child with a cleft lip, you need to conduct a full diagnosis, consult with specialists and assess the severity of the pathology. If doctors insist on early surgery, it means that the baby really needs it.
The first months and years of such a child’s life will be difficult, feeding will be difficult and parents need to be prepared for this. But do not forget that after all stages of treatment the child will be completely healthy and the problem will be left behind.
results
In patients with RHN, elements of bulbar syndrome were most often detected, and somewhat less frequently, pseudobulbar syndrome; signs of brainstem dysfunction were common; signs of dysraphic status, including vertebral anomalies, were often detected (Table 1).
Table 1. Features of the neurological status in patients with RHN
Elements of bulbar syndrome in varying degrees of severity were found in 100% of patients with RHN and had their own characteristics. First of all, attention was drawn to disturbances in the innervation of the tongue (Fig. 1): deviation of the tongue was detected in 13 (61.9%) patients; hypotrophy of the tongue - in 18 (85.7%) patients (central - in 13 (61.9%) patients, regional - in 2 (14.3%), general - in 3 (9.5%) patients); fasciculations and motor restlessness of the tongue - in 5 (23.8%) and 4 (19.0%) patients examined with RGN, respectively.
Rice. 1. Language of a child with RGN.
Sagging of the soft palate and deviation of the uvula of the soft palate (uvula) were noted in 7 (33.3%) patients of the main group. At the same time, swallowing and the pharyngeal reflex were preserved in almost all patients. Only in 1 (4.8%) case were there minor swallowing disorders.
17 (81.0%) patients of the main group had speech disorders: isolated dysarthria - 5 (23.8%), isolated dys- and nasophonia - 3 (14.3%). Severe speech disorders in the form of a complete bulbar speech syndrome - severe dysarthria in combination with disturbances in voice sonority (naso- and dysphonia), as well as with features of the speech flow (slow, less often - 3 (14.3%) cases - scanned speech) were identified in 9 (42.9%) patients. Severe speech disorders were more often noted in younger patients - their average age was 9.9 ± 2.0 years.
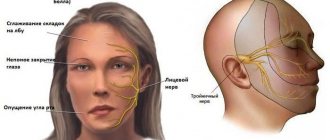
Somewhat less frequently in patients with RHN, neurological symptoms were detected from other cranial nerves (III, IV, V, VI, VII pairs): facial innervation - perioral fasciculations - 6 (28.6%), hypomimia - 5 (23.8%) , “fast and furious” facial expressions - 3 (14.3%), facial asymmetry - 2 (9.5%); weakness of the masticatory muscles and/or deviation of the lower jaw were detected in 2 (9.5%); signs of dysfunction of the oculomotor nerves - strabismus and nystagmus - in 3 (14.3%) and 4 (19.0%), respectively. Several patients had sensory organ disorders: congenital hearing loss - 2 (9.5%), congenital progressive myopia - 1 (4.8%).
Disorders of facial innervation were in 2nd place in frequency of occurrence in patients with RHN after elements of bulbar syndrome: in the group as a whole, specific features of facial expressions in the form of hypomimia, less often a kind of “forced” emphasized facial expressions were identified in 7 (33.3%) patients with RGN.
Also, very often in patients with RHN, a static disorder was detected (Fig. 2), mainly from the cervicothoracic spine - 16 (61.9%) of those examined in the main group. In patients of the main group, different shoulder heights were detected - 13 (50.0%) patients, chest asymmetry with unilateral muscle wasting - 3 (14.3%), kyphoscoliosis - 12 (57.1%) patients, limited spinal mobility - 3 (14.3%) patient.
Rice. 2. Disturbance of statics (a variant of the development of the cervicothoracic spine) in a child with RHN.
Manifestations of facial dysraphism were frequent: eye difference - 11 (52.4%) patients, hypo- and hypertelorism - 7 (33.3%) patients, facial asymmetry with underdevelopment of one half of it - 7 (33.3%) patients, various height of the ears - 3 (14.3%) patients.
Thus, it is possible to create a kind of “neurological portrait” of a patient with RGN: specific elements of bulbar syndrome (mainly affecting the tongue muscle), features of facial expressions, facial and spinal (mainly from the cervicothoracic region) dysraphism. As the age of the subjects increased, the severity of dysarthria and brainstem dysfunction (from the III-VII pairs of cranial nerves) decreased, but mild speech disorders (dysphonia and/or nasophonia) persisted even in adult patients. In older patients, vertebral problems (back pain, recurrent radicular syndromes, early degenerative changes in the spine) and signs of autonomic dysfunction came to the fore. For this reason, 6 out of 10 (60%) patients with RHN over 12 years of age were observed by a neurologist.
In addition to the characteristics of cranial innervation, microfocal neurological symptoms were found in 9 (42.9%) patients with RHN. It was predominantly represented by elements of cerebellar syndrome (nystagmus, muscle hypotonia, minimal coordination disorders) - 4 (19.0%) patients, autonomic-vascular disorders in older patients - 5 (23.8%) in patients aged 15-17 years. In 2 (9.5%) elements of akinetic-rigid syndrome were identified.
It is important to note that cognitive impairment was not typical for patients in the main group: signs of mild cognitive impairment (not limiting social adaptation) were detected in only 2 (9.5%) of the examined patients with clefts.
In several patients with RGN, the examination revealed signs of a neurological disease, which required more in-depth additional examination (MRI of the brain and spine, ultrasound examination of the brachiocephalic arteries, consultation with a pediatrician and geneticist). According to such additional examination, carried out in 5 (23.8%) patients of the main group, anomalies in the development of the brain stem and posterior cranial fossa, craniovertebral junction and neural tube were identified, in 2 patients genetically determined diseases were identified: incomplete Dandy-Walker anomaly ( underdevelopment of the cerebellum, expansion of the greater and inferior cerebellar cisterns without signs of hydrocephalus) in the structure of Stickler syndrome - 1 patient; aplasia of the corpus callosum (Fig. 3) and brainstem anomaly in the structure of Mobius syndrome - 1 patient; Chiari malformation type I in combination with characteristics of the vessels of the vertebrobasilar system (kinking syndrome of the basilar artery) - 1 patient; Chiari malformation type II in combination with spina bifida
— 1 patient; 1 patient showed signs of parahypocampal sclerosis with epileptic syndrome (Table 2).
Table 2. Developmental anomalies and diseases of the nervous system in patients with RHN
Rice.
3. MRI picture of aplasia of the corpus callosum in a girl R., 12 years old, with ROP. On sagittal FSE T1WI (a, b) the corpus callosum is not differentiated; attention is drawn to the enlarged foramen of Maugendie (a) with a relatively preserved volume of the cerebellum; its tonsils are slightly lowered (b) - to the entrance to the foramen magnum. In this case, there is a slight widening of the interhemispheric fissure and a typical “butterfly” of the lateral ventricles on FSE T2WI in the coronal projection (c). On axial FSE T1WI (d) and TE2WI (e), FLAIR T2WI (f), instead of the corpus callosum, a slightly widened interhemispheric fissure is visible with a change in the configuration of the ventricles characteristic of aplasia of the corpus callosum. In the control group, signs of bulbar syndrome and disorders of facial innervation were not recorded ( p
<0.001).
Microfocal neurological symptoms of other localization (asymmetry and/or revival of tendon reflexes, mild coordination disorders) were detected significantly ( p
<0.01) less often in controls than in patients with RHN - in 3 (27.3%) of the examined patients.
Signs of spinal dysraphism (different shoulder heights, kyphoscoliosis) were detected in 6 (54.5%) patients in the control group, facial dysraphism (different palpebral fissure heights, facial asymmetry) - in 4 (36.3%), less frequently than in the main group. but without statistically significant differences with it. It is important to note that based on clinical examination, only so-called minor developmental anomalies, often detected in practically healthy people, were recorded. At the same time, relatively gross disturbances in the statics of the cervicothoracic region detected in patients with RHN (underdevelopment of one half of the chest, high grade kyphoscoliosis, fixed torticollis) were not found in the control group.
Popular questions and answers
The pediatrician remains the main doctor for a child with a cleft lip - he prescribes additional examinations and refers to specialists. Pediatrician Daria Shchukina will tell you more about this pathology .
What complications can there be with a cleft lip?
Without treatment, the child's speech will be impaired, even if the palate is not affected. If the cleft lip is severe, there will also be difficulty sucking.
When to call a doctor at home for a cleft lip?
When a child has ARVI or similar diseases. In emergency cases, you need to call an ambulance. Treatment of cleft lip is planned; in case of such a pathology, there is no need to call a doctor at home. Are cleft palate and cleft lip the same thing? Why then are they called differently? Not really. Indeed, both diseases are congenital. A cleft lip is a cleft and a defect in the soft tissues of the lip, and a cleft palate is a cleft palate where there is communication between the oral cavity and the nasal cavity. However, they are often combined, and then the child will have both an external and internal defect. Moreover, there is a possibility of developmental defects in other organs and systems.
At what age should surgery be performed so that it is not too late?
There is no consensus on this matter. Optimally - before speech formation begins, but in general - the earlier, the better. Cleft lips can be corrected from the first days of life, or in a hospital setting in 3-4 months, sometimes also in several stages.
Cleft lip and palate are no longer a death sentence
Simply put, this anatomical defect, due to its similarity with the structure of the corresponding organs in the hare and wolf, is strictly designated as “cleft lip” and “cleft palate.” In medicine it is called cleft lip and palate. Even in the middle of the last century, such a purely external disorder represented an almost insurmountable barrier to the normal development of a child, including speech. Now such problems have already been solved. The main thing is to seek help from the appropriate specialists as early as possible.
FROM THE FIRST DAYS OF LIFE
As a rule, the expectant mother learns that a child will be born with a cleft lip and palate at 16-20 weeks of pregnancy during a screening ultrasound. Heredity affects only 15-20% of cases. The rest is due to infectious diseases, stress and toxicosis that the woman suffered in the first two months of pregnancy, when the maxillofacial skeleton is formed. It is useless to look for reasons and those to blame. It is better to immediately contact pediatric maxillofacial surgeons, send pictures and ultrasound results by email, and keep in touch with specialists by sending pictures of the next ultrasound scans.
The baby, if there are no other problems, will be born in a regular maternity hospital. You need to take a photo of what the defect looks like and send it to the doctor. In the vast majority of cases, the operation is performed when the child is 2-4 months old. Mother and child face a difficult period: due to an anatomical defect, the newborn does not eat well, cannot swallow and suck fully, in order to feed him, he has to use special bottles and nipples.
Breastfeeding is difficult to maintain under such conditions.
But, if surgery takes place within the first month of life, many problems can be avoided. True, this requires specialists who are familiar with the technique of operations on newborns and the appropriate equipment. In the Moscow Children's City Hospital No. 9 named after G.N. Speransky, all conditions came together in 2011. And for the eighth year now, specialists from the First Moscow State Medical University named after I.M. have been at its base. Sechenov operates on newborns with cleft lip and palate.
The youngest patient was only 3 days old. The baby can suckle at the breast the very next day after surgery. On the 6-7th day, mother and child are discharged home.
TO BE CONTINUED
Parents need to be prepared for the fact that the baby will undergo multi-stage treatment with the participation of many specialists. Neonatologists, anesthesiologists and maxillofacial surgeons prepare a newborn for surgery, and, if necessary, orthodontists. After surgery, a small scar remains. It usually takes six months to heal.
At 6-8 months, surgery to correct the palate is performed. It is important to do it before the baby begins to master the first syllables. At 2-2.5 years, if necessary, correction of the lip and nose is carried out, at 4-4.5 years, the alveolar process defect is eliminated. All this time, the child’s development is closely monitored by a pediatrician, neurologist, maxillofacial surgeon and psychologist. When the baby begins to master speech, a speech therapist is involved. An orthodontist monitors the baby's jaw development. The same specialist, if necessary, straightens the teeth, corrects the primary and then the permanent bite. If teeth need to be restored (children with cleft lip and palate sometimes have two missing upper front teeth), an orthopedic dentist is involved. In total, 10-15 specialists are involved in the treatment. Thanks to their efforts, the main problems are solved before school. In adolescence, if necessary and desired by the teenager, minor cosmetic problems remaining after operations are eliminated.
***
AN EXPERT IS HERE TO HELP YOU
Adil Mamedov
,
dentist, honored doctor of the Russian Federation, laureate of the international humanitarian award ICPF, doctor of medical sciences, professor, head. Department of Pediatric Dentistry and Orthodontics of the First Moscow State Medical University named after I.M. Sechenov
***
Operations to eliminate cleft lip and palate are carried out at the expense of the compulsory health insurance fund, that is, they are free for the baby’s parents.
For treatment in the appropriate clinic, you need to receive a referral in form 057u and pass the necessary tests.
***
A cleft lip and palate is only a physical defect. It does not affect mental health and mental abilities. Among the people born with this feature, there are famous scientists, great athletes, and famous musicians.
Source: Happy Parents