Types of anesthesia in pediatric dentistry
Modern dental technologies are very diverse.
Hypnosis, musical sound analgesia, laughing gas, electroanesthesia, and infiltration anesthesia can be used as anesthesia for children during dental treatment. But more often they use methods based on proven medications and compounds. Protocols can be classified according to a variety of criteria. General gradation:
- local anesthesia;
- Oxygen sedation;
- deep sedation;
- general anesthesia.
There are also different methods of how dental anesthesia is given to children:
- topical anesthesia - smearing the gums with an anesthetic to locally “freeze” the nerve endings;
- injection anesthesia - administration of the drug using a carpule syringe with a particularly thin needle;
- mask for children - used in dentistry to administer anesthesia or a nitrogen mixture.
The names of drugs for pediatric anesthesia during dental treatment deserve special mention. Most often this is:
- Sevoran for general anesthesia is a highly effective inhalation anesthetic with the highest safety profile.
- Propofol for deep sedation is a completely safe composition for intravenous anesthesia.
The method of pain relief is selected taking into account the patient’s age, indications for use, and the amount of planned dental work.
Pediatric anesthesiology is a separate branch of anesthesiological science. Approaches to anesthesia for children are generally similar to those for adult patients, but at the same time, there are very significant differences in certain issues. Considering that specialization in anesthesiology implies the ability of a doctor to provide anesthesia to a patient of any age, we believe that this article may be useful for doctors who mainly work with adult patients, but periodically encounter children in their practice.
Anatomical and physiological features strongly depend on the age of the child, and the older the child, the fewer these features become. A special group consists of newborns and children under one year of age, since this category of patients has many nuances. It should be understood that a child is not an adult of miniature size and weight, so you cannot limit yourself to just adjusting the doses of drugs used for pain relief. Each age of the child has its own specific characteristics, detailed information about which is available in the pediatric literature.
A preoperative examination of a child must necessarily include a medical history, including information about heredity and possible congenital pathology, as well as a history of the child’s growth and development. It is necessary to discuss in detail with the parents the choice of anesthesia, explain all the features, inform about possible complications and obtain written consent for anesthesia. If necessary, additional examination and consultation with specialists are prescribed. Assess the condition of the respiratory tract. The peripheral venous network is assessed for the possibility of catheterization of peripheral veins. Planned operations are postponed if the child has recently suffered a respiratory viral infection, has an exacerbation of chronic respiratory pathology or other pathology. It is necessary to give parents clear recommendations regarding the period of fasting before anesthesia, in accordance with the age of the child.
Necessary monitoring during anesthesia in children includes non-invasive blood pressure measurement, pulse oximetry, EC monitoring, gas monitoring, and body temperature monitoring. If necessary, this can be supplemented with advanced hemodynamic and other monitoring.
For anesthesia in children, general anesthesia, regional anesthesia, and a combination of these can be used. It is necessary to understand that a child under the age of 15 inclusive should not be present at his own operation, therefore the use of regional techniques is combined with general anesthesia or deep sedation. Regional anesthesia in children includes spinal, epidural, caudal, and conduction anesthesia. When performing peripheral regional blockades, ultrasound navigation and a neurostimulator should be used, which can significantly reduce the required amount of local anesthetic, speed up the blockade, make it less traumatic and reduce the number of complications. All peripheral regional blocks in children should be performed under deep sedation or general anesthesia.
General anesthesia in children usually includes mask and laryngeal-mask anesthesia, as well as general endotracheal anesthesia. In planned pediatric anesthesiology for short-term interventions, mask anesthesia with inhalation anesthetics (sevoflurane) is widely used while maintaining spontaneous breathing. Laryngeal mask anesthesia is performed for longer operations. For long-term interventions requiring the use of muscle relaxation, general endotracheal anesthesia with tracheal intubation and artificial ventilation is used. When performing emergency operations on children, given the danger of a full stomach and aspiration complications, general endotracheal anesthesia is also used.
In some situations, general intravenous anesthesia may be used in children, when intravenous anesthetics are administered through venous access directly into the bloodstream, while monitoring the patency of the upper respiratory tract and respiratory support is mandatory.
After the operation, the child awakens on the operating table, or, if necessary, is transferred to the intensive care unit for prolonged artificial ventilation in the postoperative period. If the child awakens on the table and does not require transfer to the intensive care unit, then after completion of anesthesia he is transferred to the recovery room, where he remains until recovery from anesthesia under the supervision of an anesthesiologist and nurse anesthetist.
Local anesthesia in dentistry for children
Local anesthesia is an anesthesia that temporarily blocks the transmission of nerve impulses. This means that during the treatment the child does not feel pain or discomfort. Dentists use local anesthetics as medications, selecting the composition after determining the patient’s allergic reactions.
Local anesthesia for children's teeth is usually carried out in two stages:
- application - for primary reduction of sensitivity;
- injection - administration of an anesthetic composition through an injection of an anesthetic.
Anesthesia for the treatment of baby teeth in very young patients takes place in three stages. The first is application “freezing”. The second and third are injection anesthesia. The first injection of anesthetic is performed with a minimum dose, a drop. Anesthesia takes effect almost immediately, after which the entire volume of the drug is administered.
Rodikova Tatyana
With children 3-4 years old we usually play a fairy tale - based on Frozen or invent our own. First, we smear the gums with “magic ice jam”, then we cast a spell like Elsa “to freeze microbes.” And after that we “make Olaf the snowman” or simply “freeze everything around.” Kids are happy to listen and help, which eliminates tears and whims during dental treatment.
Regional anesthesia in children and adolescents
Aizenberg V.L., Tsypin L.E., Lyannaya G.F. Russian State Medical University, Moscow
Regional anesthesia in pediatrics is a rapidly developing area of domestic anesthesiology. Only in the last four years it has firmly entered the arsenal of eight children's medical institutions in Moscow and is used in the form of combined or even independent anesthesia during operations on the abdominal organs, in pediatric oncology, urology, in orthopedics and traumatology, for minor surgical interventions and manipulations , so common in childhood.
All known types of regional anesthesia are used in children, but central blocks were the first to become most widespread: epidural, caudal, spinal and spinal epidural [3,5,6].
Since the beginning of the 70s of the last century, thanks to the work of domestic scientists, restrictions on peripheral blockades of plexuses and nerve trunks in children during operations on the limbs have been lifted [1,3].
And finally, with the advent of effective anesthetic creams such as EMLA, contact / surface anesthesia has become widespread in children for catheterization of veins, manipulation of the skin and when performing regional blockades. Moreover, you do not need to learn the last method of pain relief; you just need to follow the instructions included with the cream.
Rarely used methods today include intravenous regional anesthesia according to Beer, intraosseous and sheath anesthesia. Infiltration anesthesia is of auxiliary importance in children and adolescents.
A number of factors have contributed to the development of regional anesthesia in children.
First of all, this is the creation of an appropriate material and technical base: special needles, catheters, sets for various blockades in children, neurostimulators, local anesthetics of the amino-amide group, which raised the quality of regional blockades to a higher level and made it possible to perform them and use them with switching off the patient's consciousness due to the components of general anesthesia.
A certain role was played by the ideology of multicomponent anesthesia and the awareness that in a number of patients general anesthesia with artificial ventilation is not the method of choice and gives a number of extremely undesirable complications. This applies to the anesthesia of premature and infant children with pulmonary dysplasia, patients with a history of malignant hyperthermia, as well as children with neuromuscular diseases and some other categories of patients.
There are three undeniable advantages of regional anesthesia:
- Anesthesia, relaxation and autonomic blockade are limited only to the surgical area. Therefore, there is no need for artificial ventilation if the operation lasts more than one hour. Naturally, this does not apply to interventions on the chest organs and upper abdominal cavity. It is also important that with regional anesthesia in children, pharyngeal and laryngeal reflexes are preserved.
- Comfortable, painless and shortened postoperative period.
- Combined regional anesthesia is less expensive and directly or indirectly reduces the costs of surgery and the postoperative period.
In pediatric practice, regional anesthesia can be used in three options:
1. As an independent type of pain relief without turning off consciousness.
This is possible in newborns, infants and young patients with appropriate psychological preparation, adequate premedication that does not deprive the child of control, and complete anesthesia, both the regional blockade itself and the operation. Under similar conditions, surgical interventions can be performed in children and adolescents who are afraid of unconsciousness and loss of self-control during anesthesia. Or in well-cooperating older patients with a “full stomach” and requiring emergency surgery due to injury.
According to our data, about 18% of children and adolescents can be operated on without turning off consciousness during the operation.
The absolute indication for regional anesthesia is patients with a history of malignant hyperthermia.
2. As a component of general anesthesia with artificial ventilation through an endotracheal tube or laryngeal mask during surgical interventions on the chest, abdominal and pelvic organs.
As a rule, central types of blockades are used, including spinal - epidural anesthesia.
In this embodiment, regional anesthesia enhances the analgesic component and autonomic blockade in the surgical area, and subsequently provides analgesia in the postoperative period.
3. Regional anesthesia is performed in unconscious patients, and the unconscious state is maintained for the entire duration of the operation.
This is the most commonly used anesthesia option for children who, for various reasons, do not want or need to be present for surgery. In this case, epidural / caudal or blockade of plexuses and nerve trunks is more often used, and switching off consciousness is achieved with inhalational or intravenous anesthetics / hypnotics / in small doses. Combined regional anesthesia with switching off consciousness in a child is the method of choice for surgical interventions on the extremities and perineum. In our pediatric orthopedics and traumatology clinic, 25–30% of interventions are performed under this type of anesthesia.
Contraindications.
Absolute contraindications for regional anesthesia in pediatrics are:
- Infection in the blockade area.
- Repeated seizures.
- Coagulopathies that cannot be effectively corrected.
- Central regional blocks are contraindicated in children with anatomical abnormalities at the puncture site or neurological diseases that may progress.
- Severe hypovolemia or arterial hypotension, difficult to respond to emergency correction.
- Disagreement of patients or their parents.
Local anesthetics
Of the many well-known local anesthetics, three drugs are predominantly used in domestic practice in children: lidocaine, marcaine and naropin. Ultracaine is used to a limited extent.
Lidocaine is usually used as a 1% solution. For peripheral blockades, adrenaline is added to it at a rate of 5 mcg/ml. The drug is characterized by a short latency period of 10–12 minutes and an average anesthesia time of 2–2.5 hours in children. Lidocaine provides postoperative analgesia for about 4–7 hours without additional administration. Its total dose for peripheral blockades is 7–9 mg/kg body weight.
Marcaine /bupivacaine/ - has a longer latency period of up to 20 minutes, but provides long-term anesthesia of up to 7 hours; postoperative analgesia when using Marcaine can last up to 20 hours or more. Its disadvantage should be considered neuro and cardiotoxicity, which occur with an overdose or accidental introduction of marcaine into the bloodstream. The total dose of marcaine for central and peripheral blockades in children is 2 – 2.5 mg/kg of the child’s body weight. By manipulating the dose of the drug, a differentiated block can be caused. It is used in children in the form of a 0.25% or 0.5% solution.
Naropin (ropivacaine) is a drug in many ways similar to marcaine, but produces a shorter motor block and is less cardiotoxic. Therefore, it can be used for regional intravenous anesthesia according to Beer. In pediatric practice, 0.25% - 0.375% and 0.5% solutions are used in a dose of 2 - 2.5 mg/kg body weight.
Comparative characteristics of the drugs according to our clinic are given in Table 1.
Table 1 shows that with a similar duration of anesthesia, the latent period of naropin is shorter than that of marcaine. Together with low cardio and neurotoxicity, this makes naropin more attractive in pediatric practice compared to marcaine.
It must be noted that the main problem with the use of these local anesthetics is the fact that the pharmacopoeia and other documents regulating the use of pharmacological agents in our country do not have clearly defined recommendations regarding their use in childhood. Anesthesiologists in most countries do not encounter such difficulties.
Premedication
Patients undergoing surgery under regional combined anesthesia require premedication. The exception is children under 6 months.
But premedication should not cause deep sedation and deprive the anesthesiologist of contact with the child. It is not necessary to include atropine in the preoperative preparation unless there are special indications, for example, during artificial ventilation of the lungs using muscle relaxants, or high concentrations of fluorotane.
Atropine can be used as premedication in infants, due to the relative weakness of their sympathetic system and the dominance of the parasympathetic, but it can be avoided in school-age children and adolescents.
In most children, it is possible to do without the inclusion of narcotic analgesics in premedication, since analgesia is not needed to perform a regional block, and during surgery the problem of analgesia is reliably solved by regional anesthesia itself. This is especially relevant in social terms due to the increase in drug addiction. Excluding promedol from premedication reduces the frequency of vomiting when consciousness is turned off with inhalational anesthetics. The most commonly used analgesic for premedication in children with regional anesthesia is paracetamol, its single dose is 15–25 mg/kg body weight. The most convenient forms of paracetamol are in syrup or suppositories. It is good to combine it with midazolam endonasally in drops or orally at a dose of 0.25 - 0.4 mg/kg. Sleep comes in about 10 minutes. But the child can be woken up and contacted, since the sedative effect of midazolam wears off after 30 minutes. The combination of ketamine (2 mg/kg) and midazolam (0.4 mg/kg) provides the most effective sedation in unruly and agitated patients. For regional anesthesia, it is logical to perform sedation using short-acting barbiturates at a dose of 2–4 mg/kg body weight. In children 2–3 years old, it is better to use the rectal route, and older patients can take barbiturates by mouth 1–1.5 hours before surgery.
This premedication has an anticonvulsant effect and may be useful in mild overdoses of local anesthetics.
In addition to the above-mentioned drugs, the following are used: instead of midazolam - Relanium or diazepam, instead of paracetamol - drugs from the group of non-steroidal anti-inflammatory drugs that have a good analgesic effect, /nurofen, nimulide, ketorolac, etc./ in age-related dosages.
Turning off consciousness
In most pediatric and adolescent patients, switching off consciousness during regional anesthesia and during surgery is necessary. According to our data, more than 70% of children undergoing surgery need this.
For this purpose, both inhalational and intravenous anesthetics are used, as well as hypnotic drugs such as propofol.
Inhalational anesthetics, such as nitrous oxide with oxygen (1:1) and fluorothane at a dose of 0.4–0.6 vol/%, are more manageable and are used most often, especially at the beginning, when the child needs to establish venous access before surgery, yes and the injection of propofol into a vein is accompanied by painful sensations.
Nitrous oxide remains one of the most attractive and most popular inhalational anesthetics in children in the world today. Inhalational anesthetics allow, if necessary, to quickly deepen general anesthesia and quickly return to its initially low level. The use of ftorotan in minimal doses to turn off consciousness during regional anesthesia is not advisable in children with increased intracranial pressure, but the addition of adrenaline to local anesthetics at a dose of 5 mcg/ml against the background of ftorotane is not contraindicated.
The use of a local anesthetic cream such as EMLA allows school-age children to use an intravenous method of turning off consciousness using a small “butterfly” needle installed in a peripheral vein in the arm. Typically, sodium thiopental is used at a dose of 5-6 mg/kg or ketamine (1-2 mg/kg). Propofol (2-3 mg/kg) has been widely used in recent years. Painful sensations along the vein from its introduction are leveled by a mixture of propofol with a solution of lidocaine.
Central blockades
In childhood, any central blockade is used. This is possible from the neonatal period. Children have a number of advantages over adult patients that you need to be aware of.
They rarely have chronic diseases of the cardiovascular system, heart rhythm disturbances, arterial hypertension, and the tendency to hypotension under the influence of central blockades does not appear until a certain age.
Thus, spinal anesthesia in children under 5 years of age is not accompanied by noticeable arterial hypotension, epidural anesthesia does not reduce blood pressure in children under 8 years of age, and caudal anesthesia does not affect hemodynamics at all. Therefore, in these categories of patients there is no need to carry out preliminary “venous support” or resort to the use of sympathotonic agents.
In young children, the turnover of cerebrospinal fluid is accelerated compared to adults, so even the use of marcaine for spinal anesthesia provides them with pain relief for up to 1.5 - 2 hours, and this is not enough for serious and lengthy operations. Therefore, it is in children that it is necessary to develop combined spinal - epidural anesthesia, which is the method of choice for abdominal operations in children.
There are three methods of spinal-epidural anesthesia: single-level, two-level and using the Epistar needle, which allows you to insert an epidural catheter, administer an epidural test - a dose of anesthetic, and then perform spinal anesthesia through another channel of the same needle. This sequence of manipulations eliminates trauma to the subarachnoid space with the epidural catheter.
During central blocks, the level of location of the spinal cord and dura mater depending on age should also be taken into account.
By the time the fetus is born, its spinal cord ends at level L 3, and the dura mater in newborns ends at level S 4. By the age of one year, due to growth disproportions, the level of the spinal cord rises to L 1, the dura mater ends at S 2-3. The line connecting the iliac crests crosses the midline in infants at the level of the fifth lumbar vertebra, and in a newborn even lower - at the level of L 5 - S 1. Thus, a puncture performed higher than L 4 in infants is fraught with danger spinal cord needle injury.
It should also be noted that in newborns and infants the epidural space contains much less adipose tissue and vessels than in older patients and adults, therefore, in the neonatal period and infancy, it is possible to pass the epidural catheter from the caudal access to any desired level for epidural anesthesia subject to subsequent verification of its location.
Thus, the characteristics of childhood are more likely to favor the use of central blocks with combined anesthesia for surgical interventions in children than to impose restrictions on their use.
Peripheral blockades of plexuses and nerve trunks.
Restrictions on peripheral blockades of plexuses and nerve trunks in children were lifted in the early 70s after the advent and widespread implementation in different countries of the method of neurostimulation for a painless search for mixed and motor nerve trunks, the achievement of which was judged by the response of the corresponding muscle group [1,3] .
Then it seemed to us that with the use of neurostimulators at any age, failures in performing peripheral blockades would go away. Today, dozens of types of neurostimulators have been created, but a certain, small percentage of incomplete anesthesia is still observed and, according to various authors, amounts to 3–7%. This may be due to an insufficient volume of anesthetic, or a concentration lower than that required for this operation, as well as to anatomical variants of the nerve trunks that cannot be known in advance.
The search for nerve trunks occurs first at a current strength of 1–2 mA with a frequency of 2 hertz. This allows you to approach the nerve at a distance of approximately 1 cm. The needle and nerve come together at a current strength of 0.3 - 0.4 mA, the distance decreases to 2 mm, but the needle approaches the nerve from one side and the bevel of the needle can be directed away from the nerve trunk. In cases where the anesthetic solution tightly fills the fascial sheath containing nerve trunks and vessels, anesthesia is usually sufficient. An example is an axillary block of the brachial plexus during operations on the hand or lower third of the forearm. But when the nerve plexus is located in the form of a “crow's foot”, or branches that innervate the operation area extend from it above the level of anesthesia, then failures are possible. This applies to the lumbar plexus and all parts of the brachial plexus except the axillary fossa. In these cases, it is necessary to inject an anesthetic along the expected front of the plexus location or identify each nerve trunk separately by characteristic movements of the hand or forearm and anesthetize it. This is what we do when anesthetizing the brachial plexus using an infraclavicular approach in our own modification, anesthetizing two or three nerve trunks in turn. The method provides anesthesia up to the middle of the shoulder in the absence of complications [5].
Blockade of the sciatic nerve, the largest nerve in humans, requires a sufficiently high concentration of anesthetic in accordance with the age of the child and regardless of the approach, with the needle as close as possible to the nerve trunk.
In the literature of the last two years, reports have appeared on the identification of nerve trunks for regional anesthesia using ultrasound diagnostics with high-frequency sensors, including in childhood. Similar studies have begun in our country.
Complications.
Complications when performing peripheral regional anesthesia in children with modern equipment are extremely rare. Thus, in our orthopedic-surgical clinic over the past 4 years, there have been three unintentional punctures of a vessel per 1,500 anesthesias, which is 0.2%.
With central blockades, complications are observed more often and can be divided into two groups: specific and nonspecific.
A group of specific complications is usually associated with technical errors or specific properties of individual anesthetics and technical means. They are usually observed during the period of mastering the techniques
Much more serious are nonspecific complications, among which it is necessary to highlight toxic reactions associated with an overdose of an anesthetic or accidental direct injection into the vascular bed, aseptic and infectious inflammation in the form of meningitis, epiduritis, aseptic arachnoiditis and, of course, total block during spinal anesthesia. The total number of such complications, according to various authors, does not exceed 0.16-0.4%, and they may not have serious consequences if the anesthesiologist is prepared to eliminate them [2,4].
In conclusion, it must be emphasized that the main task of today is the need to widely introduce effective, fairly safe and economical methods of regional anesthesia into the practice of anesthesiologists working with children, at least to the same level as in the surgical treatment of adults.
Literature.
- Eisenberg V.L. // Vestn. surgery.-1972.-No. 5 – pp. 88 – 92.
- Aizenberg V.L., Pogodaeva E.N. // Clinical surgery. – 1975. – No. 5. pp.43 – 44.
- Aizenberg V.L., Tsypin L.E. Regional anesthesia in children. – M. Olympus. – 2001.- 240 p.
- Steor R.Ya., Blazhenov M.B., Aizenberg V.L. // Journal of Intensive Care. – 1998. – No. 1. – pp. 27 – 29.
- Aizenberg V.L., Tsypin L.E., Lyannaya G.F. // Anesthesiology and resuscitation. – 2003. – No. 1. – p.56 – 59.
- Dalens BJ Pediatric regional anesthesia. CKC Press Radio. Florida, - 1990.- p.491.
Regional anesthesia and pain management. Thematic collection. Moscow-Tver 2004, pp.211-221
Oxygen-nitrogen sedation
ZAX is a mixture of oxygen and nitrous oxide, often known as laughing gas. Served through a mask. After inhaling the gas, the child falls into a relaxed, sleepy state, calmly perceives the surrounding reality, hears and understands speech addressed to him.
- maintains a positive mood - at the same time as treatment, the child watches cartoons and gets great pleasure from it;
- neutralizes pain - the pain threshold increases, which allows you to endure dental treatment comfortably and calmly;
- reduces natural reactions - the child is no longer frightened by bright lamps and the buzzing of the drill.
Superficial ZAX sedation is recommended for patients over three years of age and, with an experienced doctor, can replace pediatric anesthesia during dental treatment.
PART I
Answered by Konstantin Vladimirovich Artamonov, leading anesthesiologist-resuscitator at the children's dental clinic "Malysh and Carlson."
Tell me, at what age can general anesthesia be used for dental treatment in children?
There are no age restrictions for treatment under general anesthesia. For example, under general anesthesia, reconstructive operations are performed for congenital anomalies of the structure of the maxillofacial region, for example, cleft palate in children in the first months of life.
In our clinic, we treat dental diseases for children aged one and a half years and older under general anesthesia. We recently treated decayed upper front teeth of a nine-month-old baby. The parents brought the child from abroad, since such treatment is not provided there.
On the websites of leading children's dental clinics they literally praise sevoran anesthesia, but not a word is written about its shortcomings. Tell me, does the drug Sevoran really have any disadvantages?
It would be incorrect to say that Sevoran (sevoflurane) is an ideal drug in anesthesiology. There is simply no ideal drug. However, Sevoran anesthesia (ABBOT Laboratories USA) really has virtually no side effects. Due to the low solubility of the drug in the blood, administration and removal from anesthesia occur quite quickly, which reduces the metabolism of the drug in the body to a minimum. And in the process of metabolism, non-toxic products are formed (unlike other inhalational anesthetics).
Side effects of Sevoran include dizziness upon awakening, which persists for about 30 minutes, as well as rapid restoration of pain sensitivity after recovery from anesthesia (therefore, local anesthesia is required for traumatic procedures), nausea and vomiting may occur.
In genetically predisposed patients, skeletal muscle hypermetabolism syndrome (malignant hyperthermia syndrome) may occur, the incidence rate is 1:50,000 - 1:100,000 (according to statistical data from various Russian and foreign sources).
Please help me figure out which anesthesia is safer for a child: inhalation or intravenous.
The choice of anesthesia is determined by a combination of factors, primarily the general somatic status of the patient and the scope of the upcoming treatment. Dental treatment in children on an outpatient basis is possible both using inhalation anesthesia with Sevoran (general anesthesia) and intravenous anesthesia with propofol (superficial and deep sedation) with the same degree of safety. Patient safety in our clinic is ensured by the use of modern anesthesia and respiratory equipment and hemodynamic monitoring. The anesthesiologist selects an individual dose of the drug for each child, which means that the little patient receives exactly the amount of anesthetic that he needs.
How does a child fall asleep?
The use of inhalational anesthetics during general anesthesia is all the more preferable for children because to induce anesthesia you just need to breathe through a mask, and in the case of intravenous anesthesia, you must have an intravenous catheter. Therefore, in our clinic, if there are no contraindications, inhalation anesthesia with sevoflurane is used, and an intravenous catheter is installed during sleep (for transfusion of the necessary drugs).
During anesthesia, the child does not feel pain during treatment and tooth extraction, but what sensations will he have after waking up?
Sevoran has a sufficient analgesic effect for dental treatment. Indeed, pain sensitivity is restored quickly after waking up - this is one of the few disadvantages when performing inhalation anesthesia with Sevoran. Therefore, when removing teeth under anesthesia, our pediatric dentists additionally perform local anesthesia, trying to carry out traumatic manipulations at the beginning of treatment in order to reduce the baby’s discomfort after waking up. In addition, preemptive analgesia is administered intraoperatively before treatment. In the postoperative period, non-steroidal painkillers (nurofen or paracetamol) are prescribed in age-specific dosages.
How will the child feel and behave after recovery from anesthesia? On the websites of clinics offering dental treatment under anesthesia, they mostly write that after 20 minutes the child is running and playing. Is it so?
The child’s well-being and behavior after general anesthesia depends on several components.
Firstly, the initial psycho-emotional status of the child.
Including previously acquired negative experience of dental treatment “with retention”. Often parents decide to undergo dental treatment under anesthesia when the situation in the child’s mouth is simply catastrophic. There are many inflamed and damaged teeth in the oral cavity. Naturally, when a baby does not sleep for several nights, suffering from toothache, he practically does not eat, and he feels unwell.
Secondly, the volume of dental treatment performed and the duration of anesthesia treatment.
Naturally, when several pulpitis are treated (nerves are removed and canals are filled) and severely damaged tooth crowns are restored, and in some cases tooth extraction cannot be avoided, the child will experience discomfort when waking up. Often, after a long treatment (more than three hours), babies cry because they want to eat.
Sometimes after anesthesia, children experience agitation (excitement). This is due to the fact that when a child wakes up in a half-asleep state, coordination of movements has not been fully restored. Since the child is encountering this condition for the first time, it may bother him.
These are the main factors that determine the child’s condition after general anesthesia. I would like to note that the parents’ mood, their anxiety and vigilance, as well as questions like “Do your teeth hurt, are you in pain?” also worsen the child’s mood after waking up. On the contrary, a calm attitude and the ability to distract a child lead to a quick, positive result: the child is calm, drinks water, watches cartoons.
What is preferable for administering anesthesia to a small child: an endotracheal tube or a laryngeal mask?
In the children's dental clinic "Malysh and Carlson" laryngeal masks from LMA are used to ensure airway patency during general anesthesia. The laryngeal mask is made of thin, soft latex. This is what she looks like. Masks of different sizes are selected depending on the patient’s weight.
Its fundamental difference from an endotracheal tube is that it is located only in the oropharynx and does not penetrate the larynx, which prevents irritation of the respiratory tract and trauma to the vocal cords that occur when using an endotracheal tube. That is why general anesthesia using a laryngeal mask is tolerated by small patients much more comfortably than general anesthesia using an endotracheal tube. But in some cases, tracheal intubation cannot be avoided. In such cases, of course, intubation is used (we have everything necessary for this).
Deep sedation with Propofol - drug-induced sleep
During dental treatment, anesthesia for children or deep sedation may be used. These concepts are often confused, since in both cases the child is immersed in medicated sleep. But the difference is significant:
- General anesthesia in dentistry is given to children through a mask. Artificial sleep is as deep as possible, with complete loss of sensitivity.
- Sedation with Propofol involves intravenous administration of the drug and requires additional pain relief.
Propofol guarantees:
- natural physiological state of sleep;
- falling asleep in 1-2 minutes;
- exceptionally high safety for the child;
- simple awakening and rested state;
- extremely low risk of allergic reactions and side effects.
The quality and depth of sleep is controlled by an anesthesiologist. At this time, dentists treat and save teeth, remove completely destroyed units, and install prosthetic structures.
What are the benefits for children?
Application anesthesia in dentistry for children begins to act in almost five to ten minutes. Anesthetics are produced as various gels, ointments, and sprays. Before performing dental surgery, a special antiseptic is most often used , after which is applied to:
- hard dental tissues;
- pulp;
- mucous membranes.
The application has a mild effect without damaging deep tissues. In this case, the depth of impact is within three millimeters. The analgesic effect lasts for half an hour, which allows the doctor to carry out treatment . If more time is needed, the drug is reapplied.
Application anesthesia does not cause fear in children, since it makes dental procedures virtually painless. The main substances of the drugs are tetracaine, lidocaine, benzocaine. The substances presented are intended to dull pain and block the sensitivity of nerve endings. The advantages of the procedure include complete safety and affordable cost.
Deep sedation with Propofol - drug-induced sleep
Dental anesthesia for children
Dental treatment for young children under anesthesia raises the maximum number of questions among adults. The main ones relate to the safety of the procedure and side effects. Parents are also interested in what kind of anesthesia they give their children during dental treatment - whether there are high risks of negative consequences.
Is anesthesia harmful for dental treatment for children?
Sevoran is a non-narcotic, non-toxic, completely safe drug that is used in dentistry for treatment under general anesthesia. It is given to the child through a mask, instantly putting him to sleep.
Among the advantages of the drug, confirming its safety for young patients:
- excreted from the body unchanged;
- does not affect internal organs;
- does not depress the heart;
- maintains physiological blood pressure readings.
Sevoran simply turns off consciousness and does not cause side effects. Additional positive points:
- pain relief - doctors do not administer additional drugs to the child;
- pleasant smell - children themselves breathe through the mask with pleasure;
- quick recovery from anesthesia - awakening takes only 10-15 minutes.
The high quality of the composition ensures that the use of anesthesia for dental treatment for children eliminates any unpleasant consequences.
Anesthesia at the dentist for children: features
Having figured out whether it is possible to treat a child’s teeth under general anesthesia, parents begin to prepare the child for the procedure.
To do this, the young patient is prescribed a series of examinations:
- Consultation with a dentist.
The doctor must assess the amount of work - determine caries, pulpitis, and the intensity of tooth destruction. Together with the parents, a decision will be made on how many teeth to treat, what to remove, and whether prosthetics are necessary. - Testing, primary diagnostics.
The basic set of studies is general and biochemical blood tests, electrocardiogram (ECG).
- Obtaining permission from a pediatrician.
If there are chronic diagnoses, the child is also sent for a consultation with a specialized specialist in order to eliminate any risks during dental treatment.
When all issues are agreed upon, the doctor sets a date for treatment and gives final recommendations.
Soldatenkova Alina
When removing baby teeth, it is very important to preserve space for future permanent ones. To do this, they either undergo prosthetics or go to an appointment with an orthodontist to install an orthodontic seat holder.
Parents about anesthesia
An operation is always a very important moment in a child’s life. You have to leave the familiar and safe environment of home, be in an unusual place, communicate with strangers. But this difficult period can also become a positive experience in a child’s life if you teach him to adapt to an unfamiliar environment. How this period goes largely depends on the help and support of parents, which the child needs more than ever at this time. The purpose of this message is to give recommendations on how to properly prepare a child for surgery and help him survive this period as painlessly as possible. In the days before hospitalization, we advise parents to review the booklet with their child, tell him about his illness or problem, the purpose of the surgical intervention and about anesthesia. Let the child tell you what he thinks about it, parents should try to answer all his questions. Deception should be avoided in this conversation, even if it seems reassuring.
What is anesthesia? Components and types of anesthesia
Anesthesia is a state in which the patient is unconscious, his body is motionless, relaxed and does not feel pain. Anesthesia literally means a decrease in the sensitivity of the body or part of it, up to the complete cessation of perception of information about the environment and one’s own condition. The main purpose of anesthesia is to ensure adequate protection of the human body (in this case, a child) from pain, metabolic, and emotional stress. In adult patients, anesthesia is administered in most cases during surgical operations. At the same time, in children, almost all painful manipulations, for example, painful dressings, examinations of the bladder (cystoscopy) or respiratory tract (bronchoscopy), various x-ray examinations (often magnetic resonance or computed tomography, requiring the child to remain motionless for a long time) also performed under anesthesia.
Anesthesia components
Modern anesthesia must provide several components:
- switching off consciousness - the child should not be “present” at his own operation, he should be in a state of medicated sleep;
- analgesia - elimination of pain sensitivity;
- amnesia - lack of memory (the child should not remember the period of the operation/manipulation and wake up without negative memories);
- sometimes an additional, fourth component of modern anesthesia is required - myoplegia. This happens when it is necessary to relax all the muscles during surgery. This applies to “major” operations: on the lungs, abdominal organs, spine, large joints, cranial cavity;
- Finally, today anesthesia is not carried out without monitoring - this term currently refers to careful monitoring of body functions and processes in order to prevent complications of surgery and anesthesia.
It is monitor control that allows for safe and high-quality anesthesia.
Types of anesthesia
Modern anesthetic care can be provided using a large arsenal of methods and tools used. The following main types of general anesthesia can be distinguished:
- single-component anesthesia - is carried out using one drug administered in various ways: through the respiratory tract (inhalation), intravenously, intramuscularly. This anesthesia is used for “minor” operations, painful manipulations and research;
- combined anesthesia - a combination of various drugs is used - inhalation and/or intravenous. This makes it possible to use the beneficial qualities of each component of general anesthesia;
- Regional anesthesia involves blocking pain transmission from peripheral nerves to the central nervous system by injecting a local anesthetic solution. Thus, the surgical area becomes insensitive to pain. It should be noted that regional anesthesia methods are practically not used independently in children, but their combination with general anesthesia is increasingly used in the practice of pediatric surgery. In this case, general anesthetics are used to turn off consciousness, and the remaining components are provided using regional anesthesia;
- Combined anesthesia is a method of anesthesia when general anesthesia is combined with regional methods of anesthesia.
Based on the method of drug administration, anesthesia can be divided into:
- inhalation - the anesthetic enters the patient’s body through the respiratory tract, which can be: mask - the anesthetic is supplied through a mask located on the face. With this type of anesthesia, injections are given to the child when he is already unconscious and does not feel anything. Modern inhaled drugs can cause blackout within a few breaths. Most “minor” operations and manipulations are performed in children under this type of anesthesia. endotracheal - in this case, after turning off consciousness, an endotracheal tube is inserted into the child’s trachea, through which artificial respiration is carried out and inhalation anesthetics are administered. This type of anesthesia is used for “major” operations (on the thoracic and abdominal organs and others) and special manipulations.
- intravenous - drugs are administered intravenously through a catheter placed in a vein.
Who administers the anesthesia?
An anesthesiologist is a specialist who administers anesthesia. In order to obtain a certificate as an anesthesiologist in Russia, a doctor must not only obtain a diploma of higher medical education, but also complete a two-year residency in the chosen specialty. The tasks of an anesthesiologist include not only the selection of drugs for anesthesia, but also, mainly, ensuring life safety and comfortable conditions for the patient. During the operation, the anesthesiologist constantly monitors and manages all the vital functions of the body under conditions of operational stress: breathing, blood circulation, metabolism. The anesthesiologist is constantly next to the patient and continuously monitors his condition / immediately responding to the slightest changes. Thus, the successful outcome of surgical treatment as a whole and the safety of the patient largely depend on the experience, knowledge and practical skills of the anesthesiologist.
Meeting with an anesthesiologist
Typically, the child and parents meet with the anesthesiologist for the first time before surgery/manipulation. The doctor examines the child and collects from the parents the necessary information about the history of the child’s development and diseases (history). It is very important to tell the doctor all the information he is interested in. This will help the anesthesiologist determine the plan for the necessary anesthetic examination and the method of anesthesia that should minimize the risk during the proposed operation/manipulation. The anesthesiologist must assess the patient’s level of preparedness, finally decide on the anesthesia technique, explain the features of the chosen anesthesia and the rules for preparing for it, and also discuss all issues of interest with the child’s parents. What is important to ask your anesthesiologist?
- Drugs administered before surgery (premedication) and during it;
- What will be required of the child during induction of anesthesia;
- Until what moment can you stay with your child?
- What is the expected duration of anesthesia;
- When will the child come to his senses, how will the recovery proceed and when will you be able to see him;
- How to behave correctly after anesthesia (surgery) to help your child recover as comfortably as possible;
- If your child is taking medications, it is important to ask the anesthesiologist whether they need to be taken on the day of surgery, and if so, when and in what quantities.
The conversation between the parents and the anesthesiologist ends with the signing of a document called “Informed Consent for Anesthesia.” The Informed Consent records the results of the conversation, including information about which treatments the parents consider unacceptable for their child. If the operation is performed for emergency reasons and the parents are not in the hospital, the child can be operated on without obtaining informed consent with such a decision formalized by a council of specialists. Before parents sign informed consent, the anesthesiologist must provide enough information for them to make an informed decision. Communication between parents and the doctor presupposes a high degree of trust in the professional competence of the anesthesiologist. Parents have the right to express, and the anesthesiologist, if possible, fulfill wishes about the method of anesthesia. However, it is also important to understand that no matter how unique their child’s case may seem to the parents, something similar has probably already happened in the anesthesiologist’s practice. Under no circumstances does the anesthesiologist seek to violate the parental ban on carrying out certain activities. But, if parents impose such a restriction, they must be aware that every doctor is responsible for the patient’s health - this is his professional task. Any proposed treatment is intended solely for benefit, and a categorical prohibition may hamper the effectiveness of the medical process.
Preparing a child for anesthesia
Particular attention should be paid to preparing children for anesthesia. For planned surgery, the child may have a light dinner the night before and should follow the usual drinking regime. You should also wash your baby thoroughly. It is very important that the child's stomach is empty before surgery. This measure improves the safety of anesthesia. During anesthesia, the reflexes of the human body are weak, therefore, if food or liquid remains are present in the stomach, then in the event of nausea and vomiting, there is a risk of them getting into the lungs, and this is very dangerous. Please ask your anesthesiologist what restrictions your child should follow. Particular attention should be paid to the child’s psychological preparation for surgery. When communicating with a child, it is very important to follow a few simple rules:
- Be calm! Children's anxiety coincides with the anxiety of parents. The ideal psychological preparation of a child for surgery is that the parents themselves are calm and wise about the upcoming process. Recent research has shown that reducing anxiety in parents, in turn, helps reduce anxiety in children.
- Be honest with your child. Parents must explain to the child why the operation is necessary and honestly tell the child about it, taking into account their age and development. The story is better perceived by the child in a simple, conversational form without medical details of the upcoming process.
- The child must clearly understand that everything is done only for his benefit.
- When talking to a child, you can use the following words: “The doctor needs to fix something so that your body is healthy and beautiful.”
- It is very important that the child understands that he will sleep during the operation. In a dream, people don’t feel, don’t hear, don’t see anything. The doctor will give him a medicine that will make him fall asleep, and he will only wake up when the operation is over.
- You should choose your words carefully.
Some medical terms may frighten a child. For example, when talking about anesthesia, you would be better off using the following expressions: “put you into a special medical sleep” or “take a breath of sweet air.” Choose more positive words, such as “prick” (instead of “needle”), “crib” (instead of “gurney”), “fix” or “repair” (instead of “cut off” or “remove”). Be careful when using words like "put to sleep." This may have double meaning for children whose pets do not return home after being “euthanized.” Parents must make promises that they can definitely keep. Say: “Bye! I’ll wait for you, and we’ll see you when you wake up!”, instead of: “I won’t leave you anywhere” - since this is impossible. You should not bribe or, on the contrary, intimidate a child. Such actions can only help for a short time, but will have a bad effect on the child’s psychological state in the long term.
Use optimal ways to deal with stress at different age stages of the child:
| 1-3 years | Early childhood | 1. The presence of loving, calm parents 2. Art therapy (drawing, sculpting upcoming events) 2. Fairy tale therapy (we come up with a fairy tale with a good ending about an operation on a bunny, bear cub or boy/girl) |
| 3-6 years | Game age | 1. The presence of loving, calm parents 2. Art therapy (drawing, sculpting upcoming medical events, where it is important to allow the child to be the “author” of saving the patient) 3. Fairy tale therapy (we come up with a fairy tale with a good ending about an operation on a bunny, bear cub or boy /girls) 4. Role-playing games (play in the hospital with dolls, soft toys, with a toy doctor set) |
| 6-12 years | School age | 1. The presence of loving, calm parents 2. Simulating a situation with a successful operation 2. Using books or a computer to collect information about the operation |
| 12-18 years old | Youth | 1. The presence of loving, calm parents 2. Information: the teenager needs to understand what to expect and what the sequence of the operating procedure is. Preoperative information should be age-appropriate. For example, teenagers are more interested in information from the Internet about their illness rather than the results of scientific research. |
On the day of surgery you must:
Remember that the child should not eat before surgery. Even chewing gum and candy are prohibited! Wash the child thoroughly. On the day of surgery, it is necessary to remove everything unnecessary from the child:
- jewelry, earrings, nail polish;
- if the child wears contact lenses, they must also be removed;
- If the child wears dental plates, consult the anesthesiologist about whether and when they should be removed.
If your child has a loose baby tooth, tell the anesthesiologist. The medical staff will check that there is no risk of the tooth falling out during the operation. If the child is taking medications, then on the day of surgery he should take them in accordance with the recommendations of the anesthesiologist. Talk to your child again about how the job of doctors and nurses is to help him and take care of his health. Make sure that he understands why the operation is needed and perceives the upcoming medical intervention as helping his body.
Postoperative recovery
The process of awakening after general anesthesia consists of a gradual return to independent breathing, restoration of sensitivity and movement. The anesthesiologist will try to make this process as comfortable as possible for the child. It is possible that after the operation the child will experience pain for some time, but the clinic staff has everything necessary to cope with this pain. Upon returning home, the child is likely to show himself to be more dependent: he may wake up at night, try to be with you more often than usual, and be afraid of strangers. All this will normalize over time. The most important thing at this time is the peace and love of parents. If the child wants to return to the topic of the medical intervention he experienced, praise him and tell him that you are proud of how courageously he showed himself and how well done he was for overcoming this situation. Then shift your child's attention to positive thoughts and actions.
Frequently asked questions from patients:
1.When can elective surgery be cancelled? Answer: The most common reason for such withdrawal is an acute illness of the child: ARVI, childhood infection (measles, scarlet fever, etc.), colds, fever, diarrhea, repeated unexplained vomiting. Anesthesia in these cases can cause various complications.
2.Is there a risk of complications during anesthesia? Answer: Unpredictable reactions of a particular organism are possible, which is why such careful preparation for anesthesia takes place. In modern medicine, an anesthesiologist has sufficient knowledge, skills and tools to cope with even the most difficult situation.
3.Is there a risk of waking up during anesthesia? Answer: Rare cases of intraoperative awakening have been described in the world literature, but currently anesthesiologists use modern objective methods of monitoring the level of consciousness, which makes it possible to successfully prevent such episodes even in cases where the patient cannot report it. Thus, the risk of waking up during surgery is almost reduced to zero.
4. Will there be pain during the operation? Answer: The primary task of the anesthesiologist is to protect the patient from pain. In some cases, due to the characteristics of the body, anesthesia may not completely eliminate pain sensitivity, however, the anesthesiologist always has a number of alternative techniques in his arsenal that will help him cope with any situation and prevent the presence of pain. The anesthesiologist remains close to the patient throughout the operation and has all the necessary knowledge and equipment to provide safe and comfortable anesthesia.
5.Can anesthesia affect the child’s further development, his memory, attention, and learning abilities? Answer: General anesthesia is a process that, in its complexity and depth of impact on the body, is quite comparable to surgery. Accordingly, “small” surgical interventions do not have any visible impact on the further development of the child, while “major” surgical interventions force one to change their lifestyle for some time, reduce mental and physical stress, and carry out special procedures that accelerate the recovery of the child’s body. Something similar can be seen in relation to general anesthesia. Currently, modern anesthesia drugs preserve the child’s cognitive abilities as much as possible. After prolonged anesthesia, postoperative rehabilitation therapy is sometimes required to promote final recovery. Thus, the use of modern drugs for general anesthesia ensures a favorable outcome of medical intervention.
Article - Pediatric dentistry
Features of anesthesia in children in dentistry
In pediatric practice, pain relief plays a primary role.
If an adult patient is able to endure mild discomfort and spend several hours in a row in a chair, then the child’s psyche is not yet ready for this. A painful procedure can instill a lifelong fear of dentists and interfere with quality treatment. Moreover, anesthesia gives the desired psychological effect and helps the child trust the doctor. Features of pain relief in children
- Most drugs can only be used from the age of four, which imposes severe restrictions on the treatment of very young patients.
- The anesthesiologist must be highly qualified and be able to correctly calculate the dosage.
- The child may be afraid of treatment and dental instruments, especially needles.
- Children are often allergic to anesthetics.
The choice of one type or another depends on the procedure to be performed by the doctor, the age and psychological state of the child.
Application anesthesia
- Local anesthesia in children in dentistry is not complete without the use of special anesthetic solutions or gels (most often based on lidocaine), which are used to treat the gums before starting treatment. The active substance easily passes through a thin layer of the mucous membrane and dulls sensitivity. As a rule, topical anesthesia is used to numb the site of the future injection - this is a typical feature of anesthesia in children in dentistry. But even one “freezing” with a gel or spray is enough for some procedures - for example, to remove mobile baby teeth, the roots of which have almost completely dissolved.
- Topical anesthesia products in children's clinics have a pleasant taste and aroma to make it easier for the child to tolerate treatment.
Injection anesthesia
- In pediatric practice, articaine-based anesthetics are most often used, which are administered using a syringe. This drug is approximately five times more powerful than novocaine, but is less toxic and less likely to cause allergies. It can be prescribed from the age of four.
- Injection anesthesia has its own varieties. Pediatric dentists use infiltration or conduction anesthesia depending on the indications. In the first case, an injection is made into the mucous membrane at the border of the alveolar process and the transitional fold so that the anesthetic reaches the endings of the dental nerves. In the second case, the solution has an effect on the branches of the trigeminal nerve. Conductive anesthesia in children in dentistry is permissible from the age of six and is indicated for tooth extraction - mainly in the lower jaw.
Child's oral hygiene
Dentists recommend taking care of the prevention of dental ailments in children even before the appearance of their first teeth. What does this mean, how to properly care for children’s teeth, and do the rules of oral hygiene differ between children and adults?
According to WHO (World Health Organization), 92% of people around the world brush their teeth incorrectly, therefore, adults also teach their children to brush their teeth incorrectly. Only a few people pay attention to the fact that the child’s oral cavity has significant differences from the adult’s oral cavity, which means that the hygiene of baby teeth is also different. Dentists advise paying attention to the structure of baby teeth, especially the first molars. The sixth teeth are more vulnerable than others. They erupt faster than others and often the distal tubercles are late freed from the “hood”, which serves as a place for plaque accumulation. In addition, it is in childhood that the probability of caries occurring is close to 100%. This is due to the inability of the child’s body to resist bacteria, the structure and vulnerable structure of the tooth itself, and other factors.
The best option for parents is to consult with a hygienist, who will show your child how to brush their teeth properly and tell you how often this should be done. There is one golden rule in oral hygiene that is relevant for both adults and children: after eating, brush your teeth. However, it is not always possible to follow it, especially when it comes to snacking on the go, at a party or in transport. At home, this rule must be followed strictly. The most important thing is not to forget about this important procedure and bring it to automaticity. What are the basic rules of children's hygiene?
The first months of life - taking care of your gums
In the first six months of life, the oral cavity is massively populated with microbes, which creates favorable conditions for the occurrence of caries, infantile thrush, stomatitis and other diseases. There are a lot of cases when microbes do not sleep, for example, when adults who are carriers of caries kiss a child, lick a pacifier, neglecting boiled water, and taste food with the spoon that will be fed to the baby. The risk of infection increases tenfold. To prevent something irreparable from happening, after each feeding the baby should wipe the gums with special fingertips or napkins with a weak soda solution.
Learning to brush baby teeth
Children who have already acquired teeth, with parental help, begin to brush their first baby teeth themselves using a special toothbrush for children. In this case, you need to start with 15-20 seconds for each cleaning, gradually increasing the duration. The main task of the mother at the stage of introducing the child to the brush is to awaken interest in a routine but necessary activity. There are at least two win-win ways:
- Teaching children oral hygiene goes a long way if parents offer the child a game. Having heard how the kind toothbrush aunt cleans her teeth one after another, making them beautiful and driving out harmful microbes, most kids will willingly open their mouths and patiently wait for the process to end.
- Another effective training method is to do as mom does. Often, children copy their parents' behavior, speech and facial expressions. In the same way, they learn how to brush their teeth properly. By doing daily brushing with your baby, and at the same time helping him, you will make sure that after some time the child will reach for the toothbrush on his own. The main thing is that the child likes the taste of the toothpaste!
Professional oral hygiene in children
Professional hygiene is usually understood as a set of procedures, the purpose of which is to improve the health of the tissues and organs of the oral cavity and prevent the occurrence of dental ailments. This includes removing soft and hard plaque from teeth, closing fissures, that is, dental dimples, making them less vulnerable, as well as covering the dental surface with a special varnish. The dentist's office is not as treacherous as it looks at first glance. In addition to the preventive procedure, the doctor can conduct an oral hygiene lesson, select a toothpaste and brush for the child based on the individual characteristics of the oral cavity structure, and also give useful and competent care tips.
Caries in children
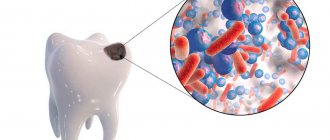
Dental caries in children: features of the disease
Considering the prevalence of caries in children, from the moment the first teeth appear, parents should pay special attention to the child’s hygiene and nutrition, as well as regularly visit the dentist for examinations and preventive procedures. All this is necessary in order to protect baby teeth as much as possible until the moment when they are replaced by molars. Look at the statistics: in children aged a year and a half, caries is diagnosed on average in 10 - 15% of cases, and by the age of five, more than 70% of children already suffer from this disease. Moreover, caries in preschool children develops at a much faster rate than in adults, so if left untreated, the child risks losing all of his baby teeth even before they begin to be replaced by molars. The causes of caries can be very different, which is largely why it is a widespread dental disease.
Types of caries in children
There are several parameters for classifying childhood caries. The key ones are the type of caries at the site of origin and the degree of its development. Below you can see what caries looks like in children in its various manifestations.
- Proximal caries
- Carious lesions are present on both one and the other antagonist teeth. Caries between teeth in children is also common, which some experts also classify as the approximal type.
- Cervical caries
- It is formed at the point of contact of the crown part of the tooth with soft tissues. Often goes deep into the tooth.
- Circular caries
- Unlike cervical caries, which are localized in a specific area, circular dental caries in children spreads along the entire gum line surrounding a specific tooth, so that over time the crown part simply falls off. This type of caries is very common in children with baby teeth.
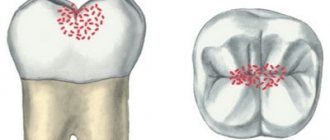
- Fissure caries
- It affects fissures - grooves on the chewing surface of the teeth. It is considered one of the most common types of caries in both primary and permanent teeth.
Stages of childhood caries
- Initial caries. At first glance, it is almost invisible and appears as a small speck on the enamel. This type of caries is highly treatable because it has not yet penetrated into the layers of enamel and dentin.
- Superficial caries. This type of caries affects the enamel layer, but not deep enough to reach the dentin. Enamel caries in children is also treated quite quickly and effectively.
- Average caries in children. At this stage, caries affects not only the enamel, but also the dentin.
- Deep caries. With deep caries, all tooth tissues (enamel, pulp, dentin) are affected. Root caries in children is the final stage.
In addition to the parameters described above, experts distinguish caries according to the rate of development: from compensated (slowly progressing caries) to decompensated (when damage to tooth tissue occurs very quickly). In addition, the disease can be either local (that is, covering one tooth) or focal, when caries moves from one tooth to another. Caries on a child’s front teeth often follows the second pattern, especially in the absence of timely treatment.
Treatment of dental caries in young children
When we talk about dental caries in young children, we mean the age category from six months to 5 years - it is at this age that a number of baby teeth are fully formed, but the process of their loss has not yet begun. Caries of primary teeth in children usually progresses quite quickly, so parents always need to be on guard in order to detect the disease in time and take the child to the dentist.
Caries in children under one year and at 1 year
When a child is one year old, dental caries is a very unpleasant problem that needs to be corrected urgently. This is the so-called early caries in children, which is becoming more common today. Before the age of one year, a child usually develops front incisors. The treatment is gentle and is carried out without a drill. Usually this is fluoridation and remineralization of teeth. What is used to protect children's teeth from caries? The teeth are saturated with useful minerals (calcium, fluoride, etc.).
Caries in a child at 1.5 years, at 2 years and at 3 years
Caries in children under 3 years of age is also usually treated with gentle methods. At this age, doctors actively use the silvering technique, when teeth are treated with a solution of silver nitrate. This is a very effective technique, the disadvantage of which is the staining of tooth enamel. For more obvious signs of caries, photodynamic therapy is effective - removing damaged tissue and treating the tooth with a laser. When teething in chewing teeth, caries in a 3-year-old child can be prevented by sealing fissures (treating the grooves of chewing teeth). Caries in children's chewing teeth can develop very quickly, so fissure sealing is a good preventative measure.
Caries in a child at 4 years old and at 5 years old
After children reach 3 years of age, ICON technology (polymerization of teeth with treatment of carious cavities with instruments) is actively used for dental treatment. In the early stages, ozone therapy is used, which makes it possible to destroy carious bacteria. For deep caries, depophoresis is effective: copper and calcium hydroxide is injected into the area affected by caries. The solution penetrates the root tubules and destroys pathogenic bacteria.
Caries in a child at 6 years old, at 7 years old, at 8 years old, at 9 years old
At this age, active replacement of milk teeth with molars occurs. During these years, doctors do not recommend placing light and photopolymer fillings. At advanced stages of caries, today, as a rule, glass ionomer fillings or colored compomers are placed on baby teeth.
Caries in a child at 10 years old, at 11 years old, at 12 years old
After ten years, the child receives a set of permanent teeth. Often, molars are treated using “adult” methods, but there are also some nuances here, in particular, different depulpation protocols and more active use of a drill. Caries of the 6th tooth is especially common in children with molars, so sealing the fissures of chewing teeth is also relevant at this age
Caries of permanent teeth in children
If a child has caries of molars, then in the long term this can cause more problems than in the case of baby teeth, because they will no longer be replaced. The peculiarities of caries in children with molars are that they need to be treated in a special format. What do we mean? Firstly, even at 15 years old, a child remains a child and has all the same fears. That is why it is recommended to use gentle techniques and sedation as anesthesia. Secondly, it is still not recommended to put polymer and some other types of fillings on children's molars. On the other hand, the anatomy and structure of molars differ from baby teeth, so in most cases it is quite difficult to do without a drill.