Difficulties in diagnosing periodontitis
Periodontitis is an inflammation of the supporting apparatus of the teeth, caused by a group of microorganisms and accompanied by the progressive destruction of the periodontal ligament and alveolar bone with the formation of a periodontal pocket, recession, or both (Carranza, 11th ed.). Periodontitis is the leading cause of tooth loss in adults (NIH report, 2004). Not even caries and its complications, but periodontitis.
Despite the scale of the problem, the specialty of periodontology is still not officially recognized in Russia. As a result, there is no residency in periodontology either.
The difficulty of diagnosing periodontitis lies in its chronic, often asymptomatic course. There is usually no pain with periodontitis, so often the main symptom visible to the patient at the beginning of the disease is bleeding when brushing the teeth. When the patient finds himself in the chair, usually several teeth are already subject to removal. The first to suffer are the molars due to the presence of tri- and bifurcation, as well as the lower incisors due to the greater accumulation of dental plaque. The canines and premolars are usually the last to go.
The level of development of medicine in general and dentistry in particular is reflected by the possibilities of early diagnosis of diseases. It is the identification of diseases at the initial stages, when the severity is mild or moderate, that allows the most effective assistance to be provided to the patient.
Dentistry can be reactionary: patients turn to the dentist when they already have serious symptoms of a particular disease. This form of dentistry is typical for developing countries. In developed countries, dentistry is mostly preventive, that is, the disease is prevented before it occurs or diagnosed in the early stages. Typically, patients visit the dentist regularly for professional hygiene, regardless of the presence of symptoms.
This preventive model is also characterized by public interest in cosmetic dentistry, when patients continue to visit the dentist not only for prevention, but also to improve their appearance. Carrying out total implantation in patients with terminal periodontal disease has long been no longer a challenge in dentistry, but rather a sign of illiteracy of doctors and/or low level of dental IQ of the patient who allowed this to happen.
A description of the diagnosis of periodontitis in the early stages, when the patient can be significantly helped, is the purpose of this article. In the following series of articles, I will try to briefly and in simple language outline the basics of periodontal patient management and the principles of periodontitis treatment.
Visit our online store of dental posters Stomanet.ru: https://lavka.stomanet.ru Only original and truly useful posters for your practice. There is also about periodontology. Free delivery throughout Russia!
Management of periodontal patients. Part 1
Part 1 - periodontal map.
Difficulty in diagnosing periodontitis
Periodontitis is an inflammation of the supporting apparatus of the teeth, caused by a group of microorganisms and accompanied by progressive destruction of the periodontal ligament and alveolar bone with the formation of a periodontal pocket, recession, or both (Carranza, 11th ed.). Periodontitis is the leading cause of tooth loss in adults (NIH report, 2004). Not even caries and its complications, but periodontitis. Despite the scale of the problem, in Russia the specialty of periodontology is still not officially recognized and, as a result, there is no residency in periodontology either. The difficulty of diagnosing periodontitis lies in its chronic, often asymptomatic course. There is usually no pain with periodontitis, so often the main symptom visible to the patient at the beginning of the disease is bleeding when brushing the teeth. When the patient finds himself in the chair, usually several teeth need to be removed. The first to suffer are the molars due to the presence of tri- and bifurcation, and the lower incisors due to the greater accumulation of dental plaque. The canines and premolars are usually the last to go. An indicator of development in medicine, as well as in dentistry, is the diagnosis of diseases in the early stages, since it is in the initial and medium stages of severity that patients receive the greatest benefit from treatment. Dentistry can be reactionary when the population seeks help from a dentist when there are already serious symptoms of a particular disease. This form of dentistry is typical for developing countries. In developed countries, dentistry is mostly preventive, when the disease is prevented before it occurs, or diagnosed in the early stages. Typically, patients visit the dentist regularly for professional hygiene, regardless of the presence of symptoms. This model of dentistry is also characterized by the fact that a considerable part of the population is interested in cosmetic dentistry, when patients continue to visit the dentist not only for prevention, but also to improve their appearance. Carrying out total implantation on patients with terminal periodontal disease has long been no longer a challenge in dentistry, but rather a sign of the illiteracy of doctors and/or the low level of dental IQ of the patient who allowed this to happen. A description of the diagnosis of periodontitis in the early stages, when the patient can be significantly helped, is the purpose of this article. In a series of subsequent articles, I will try to briefly and in simple language outline the basics of managing periodontal patients and the principles of treating periodontitis.
Why do you need an exam
Treatment for any patient with periodontitis begins with an examination. The examination is necessary to determine the patient’s treatment strategy, accurately identify hopeless teeth, if any, and also record the initial condition of the periodontium to monitor positive changes during the treatment process. The periodontal map is also an intelligible means of motivating the patient for treatment, since periodontal pockets of 4 mm and deeper are clearly highlighted by the site or software in red (Fig. 1 and 2). Since there is no pain with periodontitis, it is possible to motivate patients only by explaining the pathogenesis of periodontitis. The presentation of a treatment plan to such a patient is ALWAYS accompanied by a demonstration of a periodontal chart, x-rays and models illustrating the disease.
Option of a periodontal chart from the website periodontalchart-online in Russian
What you will need to take the exam
- Assistant. The assistant will enter measurements into the periodontal (perio) chart,
- Periodontal map. It can either be built into the software if your office is digitized, or a paper version can be downloaded from periodontalchart-online.com.
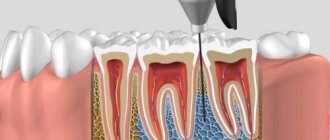
- Periodontal probe. The most convenient in my opinion is UNC-15: one division - 1 mm with black marks every 5 mm (Fig. 3).
- The exam takes an average of 30-40 minutes for the doctor + 15 minutes for the x-rays by the assistant.
Periodontal? probe UNC-15
Hygiene level , smoking
We begin the exam by collecting anamnesis: we find out the medications the patient is taking and the main systemic diseases. As you know, periodontitis has two main components: local factors (dental deposits, plaque, overhanging edges of fillings/open contacts that contribute to greater accumulation of the latter, etc.), as well as systemic factors (diabetes, smoking, obesity, stress are proven factors influencing the course of periodontitis). In the presence of systemic factors (especially diabetes and smoking), pocket formation and bone loss will occur more quickly than in the absence of such factors in a similar patient, even if hygiene is the same. Diabetes occupies a special place. Patients with diabetes are characterized by rapid destruction of periodontal tissue, so how successful the treatment of periodontitis will be will largely depend on the treatment of diabetes. A glycosylated hemoglobin level of less than 7% indicates good diabetes control. With all values higher, the treatment of periodontitis will be difficult. The dentist should motivate the patient to treat diabetes first. Smoking itself does not cause periodontitis, but it significantly accelerates its progression in those who already have it. Depending on the number of cigarettes smoked per day, bone loss in smokers, all other things being equal, is 2-5 times faster. Therefore, it is not uncommon to see a smoking patient with severe periodontitis in a chair despite the age of 40 years. With a smoking history of 25 pack/years, the periodontal age of this patient, according to the most conservative estimates, is the same as that of a similar non-smoking patient at 65 years old, all other things being equal.
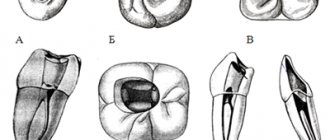
Setting pocket depth
We determine missing teeth, crown registrations, bridges, implants, etc. Next, we set the depth of the pockets (hereinafter, the pocket is the dental-gingival groove) at 6 points for each tooth: mesial-buccal pocket, mid-buccal, distal-buccal and mesial-palatal / mesial-lingual, mid-palatal / mid- lingual and distal-palatal/distal-lingual. The sequence does not matter, I do this: I start with the buccal surfaces 1.8 and gradually move tooth by tooth to 2.8, similarly the palatal pockets 2.8 - 1.8. We move to the lower jaw: cheek pockets 3.8 - 4.8 and then lingual pockets from 4.8 move to 3.8. We take measurements for each tooth and measurements at the proximal surfaces are most important, since this is where plaque accumulates the most and the pockets will be the deepest. The pressure of the probe is approximately 20 grams or the force of pressure of the probe under the ankle without causing pain.
In the intervals between the transition to the next surface (from the buccal HF to the palatal HF, from the palatal HF to the buccal LF, etc.), we note bleeding during probing. This indicator characterizes the general inflammation of the gingival tissues and indicates the activity of the pathological process: the more bleeding points and the more intense the bleeding, the faster the periodontal tissues are destroyed. It is important to interrupt and dictate the bleeding during probing to the assistant during breaks, otherwise saliva will wash away the areas of bleeding (Fig. 4).
Severe bleeding on probing.
Recessions
After determining the depth of the pockets, we record recessions; as a rule, we can limit ourselves to those on the cheek surfaces of the teeth. Recessions are measured from the cemento-enamel junction to the gingival margin. Recession in the presence of keratinized gums is not an indication for treatment, since tooth sensitivity during recession is very rare. The majority of recessions are asymptomatic and surgical closure of them is performed only for aesthetic reasons - as a rule, the “top aesthetic six”. If recessions are accompanied by mucogingival defects (lack of attached gum), then the indications for surgical intervention and increasing the amount of attached gum and/or closing the recession expand, especially in patients with poor hygiene and in the anterior part of the gum.
Rice. 5. On teeth with significant recessions, the presence of mucogingival defects is determined - the absence of attached gums. If present in the anterior mandible, they tend to become inflamed, so a free gingival graft (GTG) or connective tissue graft (CTG) to augment the attached gingiva and/or close the recession will be indicated in the FINAL stages of periodontal treatment.
Recession with a mucogingival defect - lack of attachment? gums (muco-ginigval defect)
Mobility
Tooth mobility is a very important indicator that will be important in determining the prognosis. 0 degree - physiological mobility. Mobility of the I degree is less than 1 mm in the bucco-lingual direction, II degree - all variations between I and III degrees, III degree - mobility in the apico-coronal direction is added to the lingual-buccal mobility (the tooth can be pressed vertically in the socket). Mobility is determined by light swaying movements with the finger and the probe handle or the probe and mirror handles (Fig. 6).
Determining the degree of tooth mobility using the probe handle and finger.
It should be noted that tooth mobility is a dynamic indicator and depends not only on the amount of remaining bone support for the tooth, but also on the intensity of inflammation. In the process of periodontal treatment, as inflammation decreases, mobility often improves from grade I to grade 0, and from grade II to grade I.
The involvement of molar furcations is important for determining the prognosis of these teeth, since with pockets penetrating into the furcation zone there will be a constant accumulation of plaque and it is extremely difficult to achieve high-quality instrumentation of such zones. It is extremely difficult to accurately measure furcation involvement clinically, so measurements vary between different doctors, even on the same patient. For this reason, the determination of furcation involvement will not be described, since this part of the exam is not accurate.
Are targeted photographs of the entire oral cavity optimal? X-ray diagnostic method for a new patient. Chronic generalized periodontitis of moderate severity.
Bone loss and subgingival dental plaque between 1.6 and 1.7
Arrow of the furcation between the mesiobuccal and distal buccal roots, indicating the involvement of a class 3 furcation between them.
70% bone loss? support for the central lower incisors. X-ray visible? dental? stone.
Vertical defects mesial to the molars and class 3 furcation involvement on both.
Peri-implantitis.
Periodontal expansion? gaps in tooth 2.2 due to occlusion? injuries
X-ray - diagnostics
The final stage of the exam is x-ray diagnostics. The gold standard is full mouth x-rays. This usually takes 15 minutes with an experienced assistant. An orthopantomogram would be the second choice, as it produces a lot of distortion and also cannot accurately show bone loss. CT is not the optimal x-ray diagnostic for a periodontal patient, as it provides too much unnecessary information. Also, a rare dentist with a complete record can afford to go over sections of each tooth. It should be noted that bitewing photographs are also the standard for determining caries of the proximal surfaces of the posterior teeth and at the moment there is no better way to identify early proximal caries (see Fig. 14-17) Caries of the proximal surfaces is the most common form of caries, which is often characterized by an asymptomatic course . In general, full-mouth sighting and bitewing X-rays are the optimal, inexpensive, and accessible form of X-ray diagnosis for any new periodontal or periodontally healthy patient. Carrying out such X-ray diagnostics will significantly burden both therapists and hygienists and/or periodontists of your clinic. And most importantly, patients will be diagnosed at earlier stages of both caries and periodontitis.
X-ray diagnostics of proximal caries
Positioner to speed up the acquisition of images by the assistant. It also allows the assistant to be away from the radiation source and thereby reduce the radiation dose.
Diagnosis.
There are different classifications of periodontitis, based on loss of attachment or probing depth, etc. Unfortunately, nature, when creating periodontitis, did not think about dentists, so there is no ideal and accurate classification of periodontitis and all have shortcomings. To make diagnosis easier for the clinician, most patients will have mild, moderate, or severe chronic generalized periodontitis.
Mild degree Moderate degree Severe degree
pockets 4-5 mm pockets 6-7 mm pockets >8 mm
loss of bone support - 1/3 bone loss 1/2 bone loss >1/2
lesion of furcations - class 1 lesion of furcations - class 2 furcations - class 3
———————————————-
Sergey Dolgov
diploma of dentist from RUDN University
Doctor of Dental Surgery, Master of Science in Dentistry – Saint Louis University
periodontist, private practice in Mankato, Minnesota
Member of the American Academy of Periodontology and Implantology
Author: Ivoclar Vivadent —
Why do you need to conduct an examination?
Treatment of any patient with periodontitis begins with an examination. The examination is necessary to determine the patient’s treatment strategy, accurately identify hopeless teeth, if any, and also record the initial condition of the periodontium to monitor positive changes during the treatment process.
Option of a periodontal chart from the periodontalchart-online website in Russian
A periodontal chart is also an excellent tool to motivate a patient for treatment. In images created by special services or software for maintaining periodontal charts, pockets with a depth of 4 mm or more are clearly highlighted in red, and the patient sees them. This is important, since there is no pain with periodontitis and the patient can only be motivated by explaining the pathogenesis of periodontitis. The presentation of a treatment plan to such a patient is ALWAYS accompanied by a demonstration of a periodontal chart, x-rays and drawings illustrating the disease.
Primary periodontal status. What are the stages?
It is calculated by a periodontist. After removing supragingival plaque and cleaning all subgingival areas. In fact - after professional hygiene and closed curettage. (Indicated for patients with periodontitis.) Steps:
- Photo puncture. Doctors will take photographs of your mouth before, during, and after treatment. This is a visualization of the problem - agree, we understand better when we see. Together with the doctor, you will look at enlarged photos of your teeth and figure out what requires treatment or more careful care. In addition, the photo protocol allows you to evaluate the progress of treatment, especially in cases where small changes occur over a long period, as in periodontal treatment.
- Probing and measurement of all periodontal pockets with the calculation of special indices.
- Demonstration to the patient of the periodontal diagram and selection of individual products for home care.
- Prescribing an individual gum treatment schedule and supportive professional care.
- Referral for consultation to related specialists (therapist/surgeon/orthopedist/orthodontist).
To conduct a periodontal examination, you need...
- Assistant. The assistant will enter measurements into the periodontal (perio) chart.
- Periodontal map. If you use a special program for registering patients, etc., perhaps this program allows you to create periodontal records of patients. You can print a periodontal chart from the website www.periodontalchart-online.com.
- Periodontal probe. The most convenient, in my opinion, is UNC-15: one division - 1 mm, black marks every 5 mm (Fig. 3).
Periodontal probe UNC-15
The examination takes on average 30-40 minutes of the doctor’s time + 15 minutes for the x-ray (assistant’s work).
Periodontal map
A medical history or periodontal chart is a document that contains all the information about a patient’s dental health. The medical history begins when the patient first visits the dental office and is updated with each new visit.
A periodontal record or dental record is a right that all people have to record the treatments and times they have been treated by a dentist during their lifetime, very important information so that no matter where you are, any professional dealing with you, could know the patient's oral history and thus prevent emergencies and be able to apply individual treatment.
The Importance of the Periodontal Chart This document is an excellent decision aid for the dental health professional. Thus, the main purpose of dental history is to improve the patient's medical care, since having information about his current condition and medical history makes it easier to make an appropriate diagnosis and treatment.
For legal purposes, the medical history is also of great importance as it serves as evidence of the procedures performed on the patient. This is why any new information added to the medical record must be signed and dated.
On the other hand, the medical record is also used for educational and research purposes, in which case the anonymity of the patient must be guaranteed.
The main function of a periodontal chart is to make healthcare more user-friendly by leaving a sample of all the information that a doctor can access to fully understand each patient's situation. A person's medical history is very extensive and depends on the specialty of the attending physician. In this case we are talking about dental history.
Data that can be observed in the periodontal chart. We can identify the doctors and other specialists who were involved in each intervention, so if something happens, we can find out which people were present for the various operations performed by the doctors.
Characteristics of the periodontal record As we have already seen, the medical record has a dual nature, on the one hand, as a scientific document, and on the other, as a legal document.
Therefore, it must satisfy the following characteristics:
— It must be unique, integrated, cumulative (it is completed as diagnoses and interventions are made) and chronological.
- Must contain true information.
— There must be an effective system for retrieving clinical information. Informed consent obtained in accordance with the law must be attached.
— Must be available at all times for ongoing evaluation and critical analysis by specialists.
- Must be written clearly and legibly by anyone.
Any medical record is by definition confidential and must be kept in a secure place to prevent access by third parties. There is no standard template for taking a dental history, but in order for it to be useful, it is expected to meet the characteristics already mentioned and collect the information we detail below.
How is a periodontal chart compiled? Typically, a periodontal chart consists of the following four sections:
— Medical history: it contains the most important data of the patient (name, age, contact details, general health, habits...) along with the reason for visiting the consultation. — Examination: collects all the data of interest that appears during a visit to the dentist. The examination is divided into intraoral and extraoral. The condition of each tooth is reflected in the odontogram - a schematic representation of the patient's teeth, in which the teeth are designated by two numbers: the first indicates the quadrant of the oral cavity in which the tooth is located, and the second indicates the type of tooth (molar, incisor.) - Diagnosis: with information from two In the previous sections, the dentist can make a diagnosis, which is properly reflected in the medical history. — Treatment plan: after diagnosis, the time comes for prescribed treatment (if necessary), which is also noted in the medical history. In terms of format, although a dental record can still be viewed on paper as well as in handwritten form, computer media is now preferred. This is known as a digital, electronic or computerized health record. The electronic format has a number of significant advantages:
Read on the topic: Device before and after facial treatment
Avoids storage problems: periodontal records are no longer stored in large filing cabinets, but are stored on computers or in the cloud, where they do not take up physical space.
Improves access: Finding any patient's electronic periodontal record is a matter of seconds. Moreover, if it is in the cloud, it can be accessed at any time.
Increases security: electronic history does not deteriorate and significantly reduces the likelihood of loss or artificial destruction of information.
Medical history One of the sections that we saw above is the medical history, this is where the affiliation data from the previous medical history is collected. Next, an objective examination is carried out, during which we take a detailed look at the problems that the patient may have in the oral cavity or surrounding areas, such as the lips, cheeks, palates, tongue, hard and white palate, floor of the mouth, gums, frenulum or tonsils , as well as other areas.
After this study, dental problems are also studied, in case there are problems with caries or decayed teeth.
After an exhaustive examination of the patient, it will be concluded whether he/she requires dental care or is in ideal condition, this will be added to the consultation data and reflected in the final clinical report.
Anesthesia and operating room reports are very important and the doctor and patient must work together to ensure that no problems arise. In this case, we are talking about filling out a form in which the client warns about possible allergies to materials or medications in order to prevent negligence in the event of surgery. After filling out the form and truthfully answering all questions, the consent will be signed.
We would like to point out that the patient has the right to access their dental history, with some caveats that are intended only for the medical team. Otherwise, you may be able to obtain a copy of the data in the clinical report. On the other hand, in the event of death, the information will only be available to the patient's family and friends, unless it is clearly stated that you do not allow access to their personal data.
The dental record is the only legally valid document, so it is in the interests of both parties that everything is done as correctly and thoroughly as possible. It is important that the doctor-patient relationship be developed in such a way that the treatment and results are beneficial to both the patient and the dentist.
When it comes to dental records, your dentist and doctor can certainly give you more information on how to create and maintain them. Don't delay contacting a specialist.
Hygiene level, smoking
We begin the examination by collecting an anamnesis: we find out the medications the patient is taking and the main systemic diseases. As you know, periodontitis has two main components: local factors (dental deposits, plaque, overhanging edges of fillings/open contacts that contribute to greater accumulation of the latter, etc.) and systemic factors (diabetes, smoking, obesity, stress - proven factors influencing course of periodontitis).
The presence of systemic factors in patients (especially diabetes and smoking) accelerates the formation of pockets and bone loss. Even with the same attitude towards hygiene, a patient who does not suffer from systemic factors will lose bone more slowly.
Diabetes occupies a special place. Patients with diabetes are characterized by rapid destruction of periodontal tissue, so the success of periodontitis treatment largely depends on the control of diabetes. A glycosylated hemoglobin level of less than 7% indicates good diabetes control. If this threshold is exceeded, treatment of periodontitis will be difficult. First of all, the dentist must motivate the patient to treat diabetes.
Smoking itself does not cause periodontitis, but it significantly accelerates its progression in those who already have it. Depending on the number of cigarettes smoked per day, bone loss in smokers, all other things being equal, occurs 2-5 times faster. Therefore, it is not uncommon to see a patient with severe periodontitis at the age of 40 smoking in a chair. With a smoking history of 25 years (about 1 pack per day), the periodontal condition of such a patient, according to the most conservative estimates, will be similar to the periodontal condition of a non-smoking patient aged 65 years.
Setting pocket depth
The first step is to identify missing teeth, register crowns, bridges, implants, etc. Next, we set the depth of the pockets (hereinafter, the pocket is the dental-gingival groove) at 6 points for each tooth:
- mesiobuccal pocket,
- midbuccal,
- distobuccal
- mesial-palatal/mesial-lingual,
- midpalatal/midlingual and
- distal-palatal/distal-lingual.
The sequence does not matter, I do this: I start with the buccal surfaces 1.8 and gradually move tooth by tooth to 2.8, similarly the palatal pockets 2.8 - 1.8. We move to the lower jaw: cheek pockets 3.8 - 4.8 and then lingual pockets from 4.8 move to 3.8. We take measurements for each tooth. Measurements at the proximal surfaces are most important because this is where the most plaque accumulates and the pockets are the deepest. The probe pressure is approximately 20 grams. Try to press the probe under the nail until the threshold of pain occurs, remember the force. This is a pressure of about 20 grams.
In the intervals between the transition to the next surface (from the buccal HF to the palatal HF, from the palatal HF to the buccal LF, etc.), we note bleeding during probing. This indicator characterizes the general inflammation of the gingival tissues and indicates the activity of the pathological process: the more bleeding points and the more intense it is, the faster the periodontal tissues are destroyed. It is important to pause and dictate the bleeding indicators to the assistant during probing, since saliva quickly washes away areas of bleeding.
Severe bleeding on probing.
Recessions
After determining the depth of the pockets, we should record the recessions. As a rule, we can limit ourselves to data on recessions on the cheek surfaces of teeth. Recessions are measured from the cemento-enamel junction to the gingival margin.
In the presence of keratinized gums, recession is not an indication for treatment, since tooth sensitivity during recession is very rare. Most recessions are asymptomatic and surgical closure is performed only for aesthetic reasons (“top aesthetic six”).
If recessions are accompanied by mucogingival defects (lack of attached gum), then the indications for surgical intervention and increasing the amount of attached gum and/or closing the recession expand, especially in patients with poor dental hygiene and those in whom such a situation is observed in the anterior region LF.
Recession with mucogingival defect - absence of attached gums (muco-ginigval defect)
On teeth with significant recessions, the presence of mucogingival defects is determined - the absence of attached gums. In the anterior mandible, such defects may become inflamed, so a free gingival graft (GTG) or connective tissue graft (CTG) to augment the attached gingiva and/or cover the recession will be indicated in the FINAL stages of periodontal treatment.
What is periodontal status?
Determination of periodontal status is a procedure performed by the periodontist (primary status) and the hygienist (recurrent status).
The periodontal status is determined AFTER dental treatment. There will be a whole range of examinations and diagnostics of the dental system. As a result, you will receive information (in the form of a diagram):
- about the health and condition of the gums, bone tissue and ligaments surrounding each tooth
- about the localization of plaque on each tooth, its quantity (not only in the supragingival part, but also in the subgingival space)
- degree of gum bleeding
- about areas of gums where home care needs to be improved
- about the presence/absence of pathological pockets
- what personal hygiene products you need, taking into account your characteristics.
Our periodontists use the PerioChat program, which graphically reflects all the changes that have occurred in bone tissue and soft tissues. Based on this summary table, the periodontist will select an individual gum treatment regimen.
Mobility
Tooth mobility is a very important indicator that is important for determining the prognosis. Degrees of mobility:
- 0 degree - natural physiological mobility;
- I degree - mobility less than 1 mm in the bucco-lingual direction;
- II degree - all variations between I and III degrees;
- III degree - mobility in the apico-coronal direction is added to the lingual-buccal mobility (the tooth can be pressed vertically in the socket).
Determining the degree of tooth mobility using the probe handle and finger.
Mobility is determined by light swaying movements of the fingers and the probe handle or the probe and mirror handles.
It should be noted that tooth mobility is a dynamic indicator and depends not only on the amount of remaining bone support for the tooth, but also on the intensity of inflammation. In the process of periodontal treatment, as inflammation decreases, mobility often improves from grade I to grade 0, and from grade II to grade I.
Involvement of the molar furcations is important in determining the prognosis of these teeth, since pockets penetrating into the furcation area will continually accumulate plaque there. It is extremely difficult to achieve high-quality instrumentation of such zones. It is extremely difficult to accurately measure furcation involvement clinically, so the results of measurements made by different doctors in the same patient may vary. For this reason, we do not describe the definition of furcation involvement: the accuracy of the data obtained is insufficient.
X-ray diagnostics
Sight images of the entire oral cavity are the optimal way to x-ray diagnose a new patient. Chronic generalized periodontitis of moderate severity.
The final stage of the examination is x-ray diagnostics. The gold standard is full mouth x-rays. An experienced dental assistant spends about 15 minutes on this procedure. An orthopantomogram is an acceptable choice, but it is distorting and cannot accurately show bone loss.
Bone loss and subgingival dental plaque between 1.6 and 1.7
Loss of 70% bone support in the lower central incisors. Radiologically visible tartar.
Peri-implantitis.
Arrow of the furcation between the mesiobuccal and distal buccal roots, indicating the involvement of a class 3 furcation between them.
Vertical defects mesial to the molars and class 3 furcation involvement on both.
Widening of the periodontal fissure of tooth 2.2 due to occlusal trauma
CT is not the optimal method for x-ray diagnosis of a periodontal patient, as it provides too much unnecessary information. In addition, “going over” sections of each tooth is a luxury that the rare dentist with a complete record can afford.
It should be noted that bitewing photographs are also the standard for determining caries on the proximal surfaces of posterior teeth. At the moment, there is no better way to detect early proximal caries. Proximal caries is the most common form of caries and is often asymptomatic.
X-ray diagnostics of proximal caries
In general, sighting and bitewing images of the entire oral cavity are the optimal, inexpensive and accessible form of X-ray diagnosis for any new patient, regardless of his periodontal condition. Carrying out such X-ray diagnostics will significantly burden both therapists and hygienists and/or periodontists of your clinic. The most important thing: both caries and periodontitis will be diagnosed at earlier stages.
Positioner to speed up the acquisition of images by the assistant .
It also allows the assistant to be away from the radiation source and thereby reduce the radiation dose .
Filling out a dental patient's medical record for the treatment of chronic periodontitis
EXAMPLE 2
Complaints
. Pain and bleeding gums, bad breath, difficulty chewing food.
Anamnesis
.
Pain and bleeding gums have been bothering me for days or months. Mobility appeared, indicate when
.
Previous treatment was carried out ( if carried out, indicate which one
).
Objectively. Soft and hard supra- and subgingival dental deposits in the area of the teeth______. The gums are hyperemic, swollen, bleed on probing, and purulent exudate is released from periodontal pockets. Muehlemann index______. Index Silnes - Loe______. The width of the attached gum is sufficient/insufficient
. Attachment of the frenulum of the lips, tongue______. Strands of the mucous membrane of the vestibule of the mouth in the area of _____. Bite______. Anomalies in the position of the teeth______, trema, and diastema are determined. The depth of periodontal pockets is up to 6 mm, gum recession______mm, tooth mobility______ (see Periodontogram). Overhanging edges of crowns/fillings in the teeth area______. Supracontacts in the area of teeth______. Radiologically, bone tissue resorption is determined up to 1/2 of the root length.
Diagnosis
. Chronic localized periodontitis K05.30) of mild severity in the area of teeth______.
Treatment. First visit
Training in individual oral hygiene, supervised teeth brushing. Dental plaque was removed using ultrasonic equipment and hand instruments.
Second visit
Under the form of anesthesia
anesthesia
name, concentration, dose,
curettage of periodontal pockets was carried out (including removal of subgingival dental deposits, polishing of root surfaces) in the area of the teeth______, medicinal treatment with an antiseptic solution
name, concentration, dose
.
Third visit (from one to several)
Control of individual hygiene, elimination of supracontacts, replacement of low-quality fillings on teeth______.
Next visits
Operations to correct soft tissues of the vestibule of the mouth and gums indicate the surgical procedure
.
Next visits
After 6 weeks, repeat periodontal examination. In the case of preservation of periodontal pockets, flap surgery was performed in the area of the teeth______with preliminary temporary splinting of mobile teeth, indicate the technique and material used
.
Under the type of anesthesia,
name, concentration, dose, an incision was made along the gingival margin, the mucoperiosteal flap was folded back, granulations, the epithelium of the inner surface of the mucoperiosteal flap, subgingival dental plaque, infected cement were removed, and the root surfaces were polished.
The wound was treated with an antiseptic solution name, concentration, dose
.
Osteoplastic material is introduced into the bone defect name
.
The flap is placed in place and fixed with suture material (name and number)
.
Next visit
Removing stitches.
Recommendations
Use a soft toothbrush, interdental brushes, and floss. Make oral baths with a solution name, concentration, dose for______ days. Rational prosthetics. Maintenance periodontal treatment is carried out 3 times a year.
Diagnosis
There are different classifications of periodontitis, based on loss of attachment or probing depth, etc. Unfortunately, nature, when creating periodontitis, did not think about dentists, so there is no ideal and accurate classification of periodontitis, and all used classifications have drawbacks.
To simplify, we can say that all patients suffer from ,
moderate or severe
chronic generalized periodontitis .
Chronic generalized mild periodontitis
- pocket depth - 4-5 mm;
- loss of bone support - 1/3;
- lesion of furcations - class 1.
Chronic generalized moderate periodontitis
- pocket depth - 6-7 mm;
- loss of bone support - 1/2;
- lesion of furcations - class 2.
Chronic generalized severe periodontitis
- pocket depth - >8 mm;
- loss of bone support - >1/2;
- lesion of furcations - class 3.