A number of dental procedures are impossible without laboratory diagnostic results.
Sometimes it is difficult to establish a diagnosis through examination of the patient by a dentist and using hardware diagnostic tools. In case of planned surgery, tests are also mandatory.
Laboratory diagnostics in dentistry can include both general clinical tests and complex morphological and biochemical screening.
This allows you to assess the work and condition of individual systems of the patient’s body, as well as predict the effectiveness of therapy, the approximate time of treatment and recovery.
At the first stage of making a diagnosis, the dentist examines and interviews the patient about problems with the dental system, listens to his complaints and the history of the development of the disease. In some cases, this is enough to make a diagnosis. But most often, the dentist refers the patient for an additional X-ray examination or orthopantomogram (second stage).
In 90% of cases, the data obtained is enough for a correct diagnosis and development of a treatment plan. In difficult cases, the doctor prescribes laboratory diagnostics, as well as hardware examination methods - MRI, CT, ultrasound. Popular diagnostic measures are general clinical blood and urine tests, as well as serological and microscopic examination.
Basic examination methods
Patient interview. This is done at every appointment. The doctor collects information about complaints, existing symptoms, past illnesses, medications taken, etc.
Inspection. The dentist examines the mucous membranes, teeth, evaluates the structure of the face, the closure of the dentition, the presence of swelling, edema, and other signs of inflammation. After a general examination, the condition of each of the teeth in the upper and lower jaw is assessed.
Crowns are examined using a dental mirror (allows you to see hard-to-reach areas and direct light to them). A sharp probe is used to assess the condition of the enamel. If there is a possibility of inflammation, percussion is performed, tapping the tooth (along the cutting edge or chewing surface). Normally it should be painless.
To assess the condition of the periodontium, the gums are examined, the presence of swelling, reddened, swollen, and injured areas is checked. Shallow probing may be performed to detect bleeding. If there is swelling or swelling, palpation (feeling) is performed. It is also used to assess tooth mobility.
Microscopic research methods in dentistry
This group of analyzes allows us to study the cellular structure and its changes in the oral mucosa and damaged surfaces of the dentofacial apparatus. Depending on the tasks facing the doctor, this may be a cytological sampling, biopsy or bacteriological screening.
General blood analysis.
In most cases, general clinical blood diagnostics is an additional diagnostic method. The absolute indications for using the technique are:
- Permanently appearing wounds in the oral cavity;
- Long-lasting damage to the mucous membrane;
- The appearance of necrotic tissue in the oral mucosa;
- Suspicion of problems with the functioning of the hematopoietic organs.
Very often, the first sign of a disorder in the hematopoietic processes is irritation and damage to the oral mucosa.
Biochemical diagnostics of blood and urine.
It is prescribed if a patient is suspected of having diabetes mellitus, which can manifest itself as irritation of periodontal tissue, dry mucous membranes, and the appearance of wounds and ulcers. Additionally, the doctor may decide to prescribe a gastric juice test. The main metrics in the analysis are indicators of albumin and globulins, their ratio, the amount of phosphorus and calcium in the blood serum.
Analysis for drug allergies.
The use of medications in dentistry can cause allergic reactions in the patient. This may be urticaria, blisters, tissue swelling, exanthema, anaphylactic shock. To determine the patient’s resistance, the doctor conducts a survey, studies the patient’s chart, and prescribes skin and provocative allergy tests. If necessary, indirect tests can be prescribed (injecting the patient's blood serum into the patient being studied).
Serological study.
The method consists of analyzing specific antigens and antibodies in the patient’s blood, as well as identifying certain elements of the serum through the reaction of the immune system. This method allows you to detect syphilis, brucellosis and human immunodeficiency virus.
Saliva analysis.
To make a diagnosis, in some cases of pediatric dentistry it is necessary to conduct a study of the child’s saliva. The subject of analysis may be:
- The amount and rate of saliva production in the oral cavity;
- Indicators of pro- and antioxidant systems of the body;
- Acid-base balance of saliva, an indicator of free radical oxidation;
- Mineral balance;
- Number of enzymes and buffer capacity.
Cytology.
The method is based on the study of the cellular structure and conglomerates of the analyzed surface. The cytological method is quite simple and not traumatic for the patient. It can be repeated several times. It allows you to monitor the effectiveness of prescribed therapy. And it can even be carried out on an outpatient basis, and at any stage of the inflammatory process. The analysis is taken in one of the following ways:
- Scraping from the damaged surface (ulcers, gumboils, fistulas, abscesses, erosions) and periodontal pockets;
- A smear-imprint from a damaged surface (ulcers, fluxes, fistulas, abscesses, erosions) and periodontal pockets;
- Smear reprints from the damaged surface (ulcers, gumboils, fistulas, abscesses, erosions) and periodontal pockets;
- Liquid sediment after rinsing the mouth;
- Puncture of deep periodontal tissues.
Strokes-imprints
obtained in one of two ways.
Either by applying special disinfected and degreased glass to the damaged surface (the method does not allow obtaining a print if the damage is localized deep in the mouth or access to it is difficult), or by obtaining data with a special rubber band (contact zone size 5x5 mm) and then transferring the print to the glass . Both methods are not perfect and cannot always be used. The main problem is the collection of necrotic tissue, and not the material being studied. In this case, the dentist may decide to perform a scraping
. To do this, dead areas (necrosis) are first removed from the site of damage and a smear is taken using a dental spatula (if the fistula tract is examined, the dentist uses a curettage spoon). It is important to prevent saliva, blood, and foreign objects from getting on the slide.
If catarrhal stomatitis, gingivitis or periodontitis is suspected, as well as if it is necessary to determine the reactivity of the components of the riticuloendothelial system, sediment is collected from the liquid
after several stages of rinsing the mouth (according to Yasinovsky’s method).
Collection of punctate
prescribed in case of observation of tumors, thickening of the mucous membrane and enlargement of lymph nodes. To do this, use a sterile syringe with a volume of 5 or 10 ml and a needle length of 6-8 cm. The needle is inserted into the area under study with the right hand, while fixing it with the index finger and thumb of the left hand. After the needle is inserted to a sufficient depth, I knead the area a little with the fingers of my left hand to obtain a sufficient amount of punctate. The syringe plunger is retracted while drawing. Next, the laboratory assistant disconnects the syringe and places the resulting mass on a glass slide. The procedure is carried out several times, after which the needle is removed. The procedure must be carried out quickly enough to avoid getting foreign substances or blood on the slide. Otherwise, it is difficult to prepare high-quality study drugs, which will lead to distortion of the results.
The biological material obtained as a result of the above-described manipulations is dried at room temperature (additional sources for drying are not used) and fixed in one of two mixtures - methyl alcohol or Nikiforov's solution. Additionally, the material is painted. For this, azure-eosin is used in the required concentration (depending on the urgency of the analysis).
Cytological examination allows us to determine:
- Viral diseases;
- Tuberculous ulcers;
- Some types of neoplasms;
- Acantholytic pemphigus;
- Erosion;
- Lichen planus;
- Traumatic ulcers...
It is recommended to monitor the clinical and cytological results of the study. If the data does not match, a repeat analysis or biopsy may be prescribed to eliminate diagnostic errors.
Biopsy.
It is carried out by resection of tissue for examination. The method is more accurate than cytological sampling, since there are no changes in the material that are associated with the phenomenon of autolysis. The procedure is prescribed to confirm the data of other tests or if it is impossible to establish a diagnosis using another method. For a biopsy, excision of tissue measuring 5-6 mm is sufficient. If the damaged area is small, its complete excision is recommended - the so-called total biopsy. The resulting material is also placed in a special solution and sent for histological diagnosis.
Bacterioscopy.
A bacteriological type of study in which the analyzed material is obtained from the surface of the mucous membrane to determine the cause of the disease, as well as to determine the type of bacillus. Bacterioscopy reveals:
- Syphilis;
- Gonorrhea;
- Actinomycosis;
- Infections with various fungal infections;
- Leprosy;
- Tuberculosis;
- Other.
The procedure can be carried out according to two protocols – native and fixed. In the first approach, fresh, unprocessed material is collected, placed on a glass slide and sent for research. In the second approach, the following sequence of actions is observed:
- The procedure is carried out on an empty stomach, before brushing your teeth (or 4 hours after eating and rinsing).
- The use of medications is excluded.
- The surface of the wound is cleaned with a cotton swab, and material is collected from the deep tissues.
- Cultures are carried out on various media, and the material is sent for analysis.
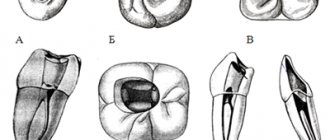
Radiography
An image is taken of a small area of the jaw, more often to diagnose the condition of one tooth. It allows you to evaluate the characteristics of bone tissue, the tooth itself, the tissues around it and its root (gums, bone, ligaments).
X-rays in dentistry are used to:
- diagnose hidden caries, pulpitis, inflammation or cracks of the root canals;
- collect information about the dental system before implantation, prosthetics or monitor their results;
- assess the volume of bone tissue during sinus lift;
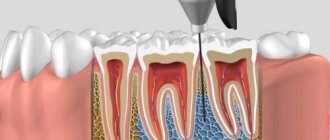
- check the quality of root canal treatment (must be filled without voids or pores);
- assess the structure of the dental system before and after orthodontic treatment;
- perform an accurate diagnosis if the patient’s complaints correspond to several diseases.
There are several types of X-rays used in dentistry.
Intraoral, dental. Performed to obtain an image of a single tooth or small area. The picture is taken using a radiovisiograph - a digital camera that captures an x-ray signal. The technology allows you to obtain high-resolution images: the doctor can see the condition of the canals, hard tissues, etc., and identify diseases at the initial stage. Radiation exposure with digital radiovisiography is minimal, which allows the method to be used for primary and intermediate diagnostics, when assessing the results and quality of treatment. The image is taken in a few minutes: a sensor is placed in the patient’s mouth on the side of the tooth being examined, and a pulsed radiation source is placed near the face. The image is available for viewing immediately.
Panoramic. It is performed to assess the structure and condition of the jaw as a whole, allows you to identify foci of inflammation or infection, pathology or disease of the TMJ, and assess the condition of the maxillary sinus and periodontium. Panoramic photographs are needed in preparation for implantation, prosthetics, and orthodontic treatment. They are performed using a special apparatus. The radiation dose is higher, but remains safe.
CT scan. It is used in planning sinus lifting, bone grafting, implantation, and other surgical interventions, and in diagnosing periodontal diseases. The photographs are taken in certain projections and used to build a three-dimensional model of the jaw. Computed tomography is very informative. The study provides information about the localization of inflammation (including intraosseous), the presence of tumor-like formations, their structure, size, features of the location of the root canals, etc.
Tests before implantation
Dental implantation, like any other procedure involving surgery, requires careful preparation. Neglecting the implantation protocol is fraught with its rejection and inflammatory processes. Therefore, it is important to pass all the necessary tests before implantation. This will allow:
- Identify hidden problems with gum tissue;
- Eliminate reactions to anesthesia and the use of medications;
- Determine the condition of the patient’s bone tissue;
- Assess the patient's general condition before surgery.
A complete list of tests that can be prescribed by a dentist before implantation:
- Clinical general blood test;
- Analysis of glucose levels in the patient's blood serum;
- Syphilis test RPR HBsAg;
- APTT;
- Fibrinogen test;
- Determination of prothrombin;
- INR;
- Determination for Antithrombin III;
- Thrombin time analysis;
- Determination of the presence of antibodies to HIV 1 and 2;
- Determination of the presence of HIV antigen 1 and 2;
- Qualitative test Anti-HCV-total;
- Urine analysis for protein and creatinine content.
Tests for periodontal disease
Periodontal disease is an extremely dangerous disease, which has a pronounced systemic-dystrophic nature in relation to periodontal tissues. Often, to get rid of a disease, it is necessary to jointly diagnose and draw up a treatment plan from specialists in several fields - a general dentist, periodontist, and therapist. Therefore, in the process of preparing for therapy, the doctor can prescribe the widest possible list of laboratory tests. The results of the study make it possible to identify which system of the patient’s body has weakened, which led to the development of periodontal disease.
Computed tomography (CT)
Computed tomography is used to examine bone structures in more detail .
Most often, the need for CT arises for intra-articular fractures and to clarify the structure of bone tumors. The accuracy of the study is achieved through a series of layer-by-layer X-ray images of the examined area, obtained by the doctor after computer processing.
Pros of CT:
- High information content in the study of bone structures;
- Ability to evaluate soft tissues;
- Possibility of computer 3D reconstruction of the studied area.
Cons of CT:
- High radiation exposure;
- Inability to use frequently;
- The impossibility of conducting research in patients with fear of closed spaces (claustrophobia).
Comprehensive diagnostics at the Estetika clinic
Our clinic in Novosibirsk has modern German dental equipment installed. High-precision equipment allows for high-quality radiation diagnostics, which is one of the informative research methods in dentistry. We also have a modern digital device “Gendex” for three-dimensional diagnostics.
The articles published on the site are for informational purposes only, and the services described may not correspond to the list of services provided in the dental clinic. Please check with the administrator for the availability and cost of procedures.
Saliva examination
To make a diagnosis, it is sometimes necessary to determine the amount of saliva and the rate of its secretion, calculate the pH value, buffer capacity, and check the mineral composition. For example, a deficiency or excess of one or another element can provoke unfavorable conditions for enamel.
No less important are the biochemical parameters of the oral fluid:
- indicators of anti- and pro-oxidant systems;
- free radical oxidation values;
- the amount of enzymes in saliva, etc.
Microbiological studies
This is a determination of the composition of the oral microflora and its sensitivity to antibacterial drugs. The reason for the importance of the study is not only the huge role of the microbial factor in the development of inflammation, but also the large number of cases where the disease is particularly resistant to traditional therapeutic interventions. Microbiological tests make it possible to determine the causative agent of inflammation, determine which antibiotic will be most effective in eliminating it, and also determine the treatment tactics for a specific form of periodontitis. Microbiological studies are also important because new microbial associations are emerging and their resistance to common antibiotics is increasing. Analysis of oral samples is usually performed before and after treatment to control its quality.
Up to contents
Biochemical methods
This is mainly a biochemical blood test. It is performed to detect signs of inflammation and changes in metabolic processes. Periodontal disease, especially in people over 40 years of age, is often accompanied by changes in lipid levels. A short (several indicators) or extensive biochemical analysis can be performed. Close attention is also paid to the composition of cells, their color, the presence of microbes, cell adhesion, etc. As a result of research, it is possible to establish the intensity of the development of inflammation and the direction of development of the pathological process.
Up to contents