Pharmacological properties of the drug Nurofen™ for children
The mechanism of action is due to inhibition of the synthesis of prostaglandins - mediators of pain, inflammation and temperature response. The drug has analgesic, antipyretic and anti-inflammatory effects, inhibits platelet aggregation. After oral administration, it is quickly and almost completely absorbed from the digestive tract. The maximum concentration of the active substance in the blood plasma is achieved 1–2 hours after administration. Ibuprofen is 90–99% bound to plasma proteins and penetrates into the synovial fluid. Metabolized in the liver to two inactive metabolites, which are quickly and almost completely excreted by the kidneys. A certain amount (10%) is excreted unchanged. The half-life is 2 hours.
How to give medicine to a child: rules and life hacks
Contents How to cut and crush tablets, capsules, patches?
What to do if you need very small doses of the drug?
Can long-acting drugs be divided into parts?
How to properly use patches for transdermal drug administration?
How to administer medications through feeding tubes?
A child cannot swallow a tablet or capsule whole, the drug does not have the required dosage and/or release form, the child has a “feeding” tube for feeding and administering drugs - how to give him medicine? How to do everything correctly, and most importantly, safely? Natalya Savva, Candidate of Medical Sciences, Associate Professor, Director of Scientific and Methodological Work of the Children's Palliative Foundation talks about this.
How to cut and crush tablets, capsules, patches?
The administration of a drug not according to its instructions is called off-label. This is any division of the tablet into parts, its crushing, dissolution, non-standard use of the solution from the ampoule. The effectiveness of drugs administered off-label may be reduced, and side effects may differ from those described in the instructions. But doctors often turn to such methods, not only in Russia, but throughout the world.
Nowadays there are many devices for dividing tablets into pieces and grinding them into powder. They are light, small, easy to carry, and can be purchased at a pharmacy or online. There are three main types of such devices:
- a device for dividing the tablet into parts (usually into two halves, then half can be divided further in half);
Photo: www.joom.com
- a device for grinding tablets (the simplest ones, like a mill, grind the tablet into powder, more complex ones can divide the tablet into equal parts and grind it into powder, there are devices with quiet operation for dividing and grinding at night);
Photo: dokmed.ru
- mortar and pestle (for grinding spices, can be used for grinding tablets, sold in regular stores).
Photo: ru.wikipedia.org
On sale you can find products “2 in 1” (for dividing and grinding tablets) and “3 in 1” (an organizer for storing tablets with a device for dividing and grinding).
Photo: market.yandex.ru
Photo: www.ozon.ru
What to do if you need very small doses of the drug?
Painkillers and other prescription drugs during a pandemic: how to get them?
How do I get a prescription for an elderly relative living alone? What to do if the pharmacy does not have the prescribed drug? What if the emergency doctor does not have the necessary medicine? Valeria Mikhailova Editorial team
Receiving palliative care
The tablet can be easily divided into four parts using the above devices or even a thin, sharp knife. Breaking the tablet into smaller pieces is difficult, especially if it is small or contains a large dose of medication and the child needs a very small dose. The contents of the capsule (powder or granules) are also difficult to divide into equal parts.
If such a situation arises, ask your local pediatrician to write a prescription to the pharmacy: there they can make a powder from tablets and capsules, and also make a liquid form of the drug from tablets (not from all tablets).
There are special pharmacies for extratemporal preparation (when the medicine is prepared in a pharmacy according to a doctor's prescription for a specific person) and a limited number of pharmacies that work with potent narcotic and psychotropic drugs. If the doctor has agreed and it is possible to buy a ready-made liquid form at the pharmacy (for parenteral administration of the medicine), use the solution from the ampoule (draw up with a small or insulin syringe).
If you need to divide the tablet into more than four parts, and there is no way to change the form of the drug, grind part of the tablet into powder, pour it into an insulin syringe without a needle and dose the desired part. The same can be done with the contents of the capsule. If you don’t have an insulin syringe, pour the crushed tablet or capsule contents onto a piece of paper in a square, evenly distribute the powder/granules into 2-6 squares and take the desired part.
Can long-acting drugs be divided into parts?
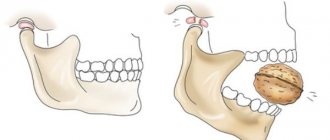
Tablets, capsules and patches designed for prolonged administration of the drug cannot be divided . They were invented to gradually introduce the drug into the body over a long period of time, so as not to take many pills often. If the integrity of the shell is broken, a large dose of the medicine will quickly enter the body. This may lead to an overdose. Therefore, the form and dosage of the drug must be selected initially so that there is no need to divide it into parts.
For example, extended-release morphine sulfate tablets
(MST) should never be divided into parts under any circumstances.
But extended-release morphine sulfate capsules
can be opened and the contents of the capsule can be used, divided into parts and mixed with water: each granule in the capsule of this particular drug is designed as a prolonged-release microtablet. And the capsule shell is intended only for storage (like sachets/sachets of the drug).
Important Always consult your doctor
How to properly use patches for transdermal (transdermal) drug administration?
Patches for percutaneous (transdermal) administration of drugs are divided into those that cannot be divided categorically (reservoir type) and those that are undesirable to be divided and cut (matrix).
Reservoir-type fentanyl patches must not be shared. It contains a clear opioid gel that penetrates the skin through a special semi-permeable membrane. If it is damaged, the absorption of the drug cannot be controlled, and rapid absorption will lead to serious overdose of the drug and severe side effects.
Matrix patches
(painkillers, anti-drooling) order in the right dosage so that you don’t have to divide them. As a last resort, if the situation is desperate, you can divide the matrix patch into parts, but first consult with your doctor, because dividing the expected effect may change.
Place the patch for percutaneous administration of the drug on a flat surface! There should be no damage or hair on the skin of the body or shoulder. Before applying the patch, if necessary, remove hair, rinse the skin with clean water (do not use products that irritate the skin) and dry the application area thoroughly.
The patch for percutaneous administration is sold in special thermal packaging: it must be glued to the skin immediately after removal, otherwise its effectiveness will decrease. To apply the patch, remove the protective film from it, and then press it firmly to the application site for 30 seconds. Make sure the patch fits snugly against your skin, especially around the edges. If the child sweats and the medication patch comes off immediately or when worn, cover it on top with a regular fixing patch.
The transdermal patch is protected by a waterproof film, so you can wear it in the shower (but not for long). The patch must be worn continuously for the time prescribed by the doctor (for example, 72 hours), after which it is replaced with a new one. Always apply a new transdermal patch to a different area of skin without touching the site of the previous application. The patch can be re-applied to the same application site no earlier than after 5-7 days.
How to administer medications through feeding tubes?
Doctors offer to put a gastrostomy on a child, but I’m afraid
Why parents are afraid - we’ll figure it out together with specialists and those who have already gone through the procedure Natalya Lavrinovich
Stomas
If the drug is administered incorrectly, the tube may become clogged. To prevent this from happening, follow some rules:
- Dissolve the crushed tablet or capsule contents in 10 ml of boiled water at room temperature. To administer the drug into the jejunum, dissolve it in sterile water.
- Flush the tube with water before and after administering the medication slowly, using the volume of water determined by your doctor. In children under 1-2 years old it is usually up to 10 ml, in children older - 15-20 ml. If the drug is administered into the stomach, use plain water, if into the jejunum, use sterile water.
- For flushing, use a syringe with a volume of at least 20 ml so as not to create high pressure from injection (the smaller the volume of the syringe, the higher the pressure). Flush the tube slowly and gently using an intermittent start-stop technique.
- Do not mix medications with food: the tube may become clogged, and if the food is poorly absorbed, the medication will be absorbed unpredictably. The scheme is as follows: food - rinsing - medicine - rinsing - food.
- If feeding is being given by drip, stop the infusion, administer the medication, rinse with water, and continue feeding.
- If you need to administer several drugs, administer them one at a time, doing at least minimal rinsing between them: they may interact with each other.
- Some drugs interact: for example, iron and zinc. They need to be administered at different times.
- There are drugs that can stick to the wall of the tube (carbamazepine, clonazepam, diazepam, phenytoin). Dissolve them with water (at least 30 ml).
- There are forms of the drugs that are highly viscous and can clog the tube. Dilute them with water (at least 30 ml).
- If you are injecting an injection into the tube, be sure to dilute it with water (at least 30 ml).
Important Do not crush or inject coated, long-acting drugs for buccal or sublingual administration into the stomach or jejunum.
Memo: caring for a gastrostomy tube How to care for the oral cavity, take a shower and monitor the patient’s diet Vera Foundation
Care
- There are drugs that, when interacting with food, form a suspension (antacids, promethazine). It can block the tube, so administer such medications separately from food, rinsing the tube with water.
- There are drugs that cannot be administered with food, since food does not allow the medicine to be absorbed (carbamazepine, ciprofloxacin, phenytoin, warfarin). Enter them 1-2 hours after or an hour before meals, dilute them with water (at least 30 ml).
- There are medications that need to be administered on an empty stomach (ketoconazole, penicillins, tetracyclines). They should not be administered into the jejunum. The drug must be well dissolved in water and the tube must be rinsed before and after administration.
- It is better to dissolve the drug in a syringe with warm water, alkaline/carbonated drinks (the pH of the drug must be taken into account). Be sure to consult your doctor first!
- To unblock the tube, you can use warm water, alkaline (carbonated) drinks, or a mixture of proteolytic enzymes. Consult your doctor in advance!
On the website of the Children's Palliative Foundation in the "Library" section there is a "Formula of drugs in palliative pediatrics", which indicates the specifics of dilution and administration of certain drugs.
Created using a grant from the Absolut-Help Charitable Foundation
Stock image used from Depositphotos.
Use of Nurofen™ for children
Oral only. The dose for children depends on the age and body weight of the child. Single dose - 5–10 mg/kg. The maximum daily dose should not exceed 30 mg/kg. Children aged 3 to 6 months - 2.5 ml of suspension (50 mg) every 8 hours, but not more than 7.5 ml (150 mg) per day. Children aged 6 to 12 months - 2.5 ml of suspension (50 mg) every 6 hours and no more than 10 ml (200 mg) per day. Children aged 1 to 3 years - 5 ml of suspension (100 mg) every 8 hours and no more than 15 ml (300 mg) per day. Children aged 4 to 6 years - 7.5 ml of suspension (150 mg) 3 times a day (450 mg). Children aged 7 to 9 years - 10 ml of suspension (200 mg) 3 times a day (600 mg). Children aged 10 to 12 years - 15 ml of suspension (300 mg) 3 times a day (900 mg). For fever after immunization (children aged 3–6 months) - 2.5 ml, if necessary - another 2.5 ml after 6 hours, but not more than 5 ml over 24 hours. The duration of use depends on the course of the disease and is usually 3 days
Side effects of Nurofen™ for children
Hypersensitivity may manifest itself as a nonspecific allergic reaction and anaphylaxis; exacerbation of asthma, bronchospasm; various skin rashes. From the gastrointestinal tract : nausea, vomiting, discomfort or pain in the epigastric region, laxative effect, possible exacerbation or development of gastric ulcer, bleeding. From the nervous system : headache, dizziness. From the hematopoietic organs : anemia, thrombocytopenia, agranulocytosis, leukopenia. From the urinary system : impaired renal function. If any side effect occurs, discontinue the drug immediately and provide proper care.
Special instructions for the use of Nurofen™ for children
The drug should be used with caution when:
- systemic connective tissue diseases;
- hypertension (arterial hypertension) and/or heart disease;
- liver and/or kidney failure.
If gastrointestinal bleeding or ulcers develop, the drug should be discontinued immediately. In patients with severe dehydration, ensure sufficient fluid intake. Particular caution must be exercised when used in children with severe dehydration due to diarrhea, after major surgical interventions, with cardiac, hepatic and renal failure, when using diuretics. In these cases, careful monitoring of diuresis and renal function is necessary.
NUROFEN oral suspension (strawberry), 100mg/5ml 100ml bottle
The simultaneous use of ibuprofen with the following drugs should be avoided: · Acetylsalicylic acid: with the exception of low doses of acetylsalicylic acid (not more than 75 m by a doctor, since combined use may increase the risk of side effects. With simultaneous use, ibuprofen reduces the anti-inflammatory and antiplatelet effect of acetylsalicylic acid (possibly increased incidence of acute coronary insufficiency in patients receiving small doses of acetylsalicylic acid as an antiplatelet agent after starting ibuprofen).Other NSAIDs, including selective COX-2 inhibitors: the simultaneous use of two or more drugs from the group of NSAIDs should be avoided -due to a possible increase in the risk of side effects.Use with caution simultaneously with the following drugs: · Anticoagulants and thrombolytic drugs: NSAIDs may enhance the effect of anticoagulants, in particular warfarin and thrombolytic drugs. · Antihypertensives (ACE inhibitors and angiotensin II antagonists) and diuretics: NSAIDs may reduce the effectiveness of drugs in these groups. Diuretics and ACE inhibitors may increase the nephrotoxicity of NSAIDs. · Glucocorticosteroids: increased risk of gastrointestinal ulceration and gastrointestinal bleeding. · Antiplatelet agents and selective serotonin reuptake inhibitors: increased risk of gastrointestinal bleeding. · Cardiac glycosides: simultaneous administration of NSAIDs and cardiac glycosides can lead to worsening heart failure, a decrease in glomerular filtration rate and an increase in the concentration of cardiac glycosides in the blood plasma. · Lithium preparations: there is evidence of the likelihood of an increase in the concentration of lithium in the blood plasma during the use of NSAIDs. · Methotrexate: there is evidence of the likelihood of an increase in the concentration of methotrexate in the blood plasma during the use of NSAIDs. · Cyclosporine: increased risk of nephrotoxicity with simultaneous administration of NSAIDs and cyclosporine. · Mifepristone: NSAIDs should be started no earlier than 8-12 days after taking mifepristone, as NSAIDs may reduce the effectiveness of mifepristone. · Tacrolimus: When NSAIDs and tacrolimus are co-administered, the risk of nephrotoxicity may increase. · Zidovudine: Concomitant use of NSAIDs and zidovudine may lead to increased hematotoxicity. There is evidence of an increased risk of hemarthrosis and hematomas in HIV-positive patients with hemophilia who received concomitant treatment with zidovudine and ibuprofen. · Quinolone antibiotics: In patients receiving concomitant treatment with NSAIDs and quinolone antibiotics, the risk of seizures may be increased.
Interactions of Nurofen™ for children
Concomitant use with:
- acetylsalicylic acid or with other NSAIDs and GCS drugs (the risk of side effects from the gastrointestinal tract increases);
- anticoagulants (increasing the effect of oral anticoagulants and increasing the risk of bleeding).
Use cautiously simultaneously with:
- antihypertensive drugs and diuretics (increased risk of developing a reaction from the kidneys);
- methotrexate and lithium drugs (increased levels of these drugs in the blood plasma);
- cyclosporines (drug interactions are possible, which can lead to an increased risk of nephrotoxicity).
Nurofen for children Suspension, 200 ml, 100/5 mg/ml, for oral administration, for children, strawberry
Interaction with other drugs
The simultaneous use of ibuprofen with the following LSAs: acetylsalicylic acid should be avoided: with the exception of low doses of acetylsalicylic acid (no more than 75 mg/day) prescribed by a doctor, since combined use may increase the risk of side effects. With simultaneous use, ibuprofen reduces the anti-inflammatory and antiplatelet effect of acetylsalicylic acid (an increase in the incidence of acute coronary insufficiency in patients receiving small doses of acetylsalicylic acid as an antiplatelet agent is possible after starting ibuprofen). Other NSAIDs, incl. selective COX-2 inhibitors: the simultaneous use of two or more drugs from the NSAID group should be avoided due to a possible increase in the risk of side effects. Use with caution simultaneously with the following drugs Anticoagulants and thrombolytic drugs: NSAIDs may enhance the effect of anticoagulants, in particular warfarin and thrombolytic drugs drugs. Antihypertensive drugs (ACE inhibitors and angiotensin II antagonists) and diuretics: NSAIDs may reduce the effectiveness of drugs in these groups. Diuretics and ACE inhibitors may increase the nephrotoxicity of NSAIDs. GCS: increased risk of gastrointestinal ulcers and gastrointestinal bleeding. Antiplatelet agents and SSRIs: increased risk of gastrointestinal bleeding. Cardiac glycosides: simultaneous administration of NSAIDs and cardiac glycosides may lead to worsening heart failure, a decrease in glomerular filtration rate and an increase in the concentration of cardiac glycosides in the blood plasma. Lithium preparations: there is evidence of the likelihood of an increase in the concentration of lithium in the blood plasma during the use of NSAIDs. Methotrexate: there is evidence of the likelihood of an increase in the concentration of methotrexate in the blood plasma during the use of NSAIDs. Cyclosporine: increased risk of nephrotoxicity when NSAIDs and cyclosporine are co-administered. Mifepristone: NSAIDs should be started no earlier than 8-12 days after taking mifepristone, as NSAIDs may reduce the effectiveness of mifepristone. Tacrolimus: when NSAIDs and tacrolimus are co-administered, there may be an increased risk of nephrotoxicity. Zidovudine : Concomitant use of NSAIDs and zidovudine may lead to increased hematotoxicity. There is evidence of an increased risk of hemarthrosis and hematomas in HIV-positive patients with hemophilia who received joint treatment with zidovudine and ibuprofen. Quinolone antibiotics: in patients receiving joint treatment with NSAIDs and quinolone antibiotics, there may be an increased risk of seizures.
Overdose of Nurofen™ for children, symptoms and treatment
Increasing the dose to 400 mg/kg may cause acute intoxication, which may be accompanied by nausea, vomiting, abdominal pain, dizziness, headache, drowsiness, nystagmus, blurred vision, tinnitus and, rarely, decreased blood pressure, metabolic acidosis, and renal failure. and loss of consciousness. When the first signs of overdose appear, you should immediately stop using the drug and carry out symptomatic therapy. There is no specific antidote.