Costen's syndrome (pathological bite) was discovered in the 30s of the twentieth century by otolaryngol D. Costen and is one of the types of deviations in the functioning of the temporomandibular joint.
The essence of the pathology is the incorrect distribution of the load between the upper and lower jaws, leading to inflammation of the cartilage disc and its further degeneration in the absence of the necessary treatment.
The main complication of Costen's syndrome is a sharp decrease or complete loss of joint mobility.
Pathogenesis
The symptom complex develops when the ligamentous apparatus is weakened, inflammatory exudate accumulates in the joint cavity, due to which the disc does not fit tightly to the articular head and a popping sound occurs when moving, due to deformation of the articular heads caused by the deposition of salts; in collagen diseases, joint stiffness and accompanying phenomena are caused by destructive processes in the connective tissue. According to Kosten, with movements of the altered articular head, compression of the auditory tube, pressure on the auriculotemporal nerve and chorda tympani is possible.
Symptoms of Costen's syndrome
A characteristic feature of the symptoms of this pathology is that often the signs of Costen syndrome are completely unrelated to each other. In particular, these include:
- difficulties in opening and closing the mouth, its incomplete opening;
- sharp pain while chewing;
- the appearance of extraneous sounds when the jaws work - crunching and clicking;
- sensations of dryness and soreness in the throat and root of the tongue;
- the appearance of a rash on the mucous membranes of the oral cavity;
- trigeminal neuralgia, which leads to acute pain covering one side of the face;
- the occurrence of paroxysmal pain in the head and ears.
At the initial stage of development of Costen's pathology, symptoms may be completely absent.
Treatment
Treatment is aimed at eliminating the underlying disease and normalizing joint function. In cases of malocclusion, orthodontic treatment methods are used (see), dental prosthetics. If habitual dislocation has developed, dentures with special devices are recommended.
Forecast
depends on the outcome of the underlying disease.
See also Bite.
Bibliography:
Rabukhina N. A. Recognition of degenerative lesions of the temporomandibular joint using layer-by-layer radiography, Dentistry, No. 2, p. 27, 1960; Rubin L.R. and Shargorodsky L.E. Pathological bite syndrome, ibid., No. 2, p. 75, 1965; Costen J. V. Syndrome of ear and sinus symptoms dependent upon disturbed function of temporomandibular joint, Ann. Otol. (St Louis), v. 43, p. 1, 19 34; aka, Mechanism of trismus and its occurrence in mandibular joint dysfunction, ibid., v. 48, p. 499, 1939.
V. D. Shorin.
Classification
Costen syndrome has four stages of development:
- the first stage is manifested by a gradual narrowing of the joint space and loosening of the ligaments;
- at the second stage, the ability of the temporomandibular joint to move is significantly reduced, and ossification of the condylar process of the mandible is observed;
- the third stage is characterized by degeneration of the cartilage disc and the occurrence of sclerosis of the joint surfaces, while the mobility of the lower jaw is gradually lost;
- the fourth stage is characterized by active growth of fibrous tissue, almost complete immobilization of the lower jaw.
Consequences of Costen's syndrome
This pathology can lead to significant consequences in the functioning of many systems of the human body:
- accumulation of fluid in the joint cavity, as a result - loose fit of the disc to the head and the occurrence of unpleasant sounds when chewing;
- weakening of ligaments;
- indigestion resulting from inadequate digestion of food.
Diagnosis and treatment
To diagnose Costain's syndrome, the gnathologist performs a visual examination of the Patient, and then prescribes a phalangeal test, ear tympanometry and a photo of the jaws.
To treat pathology use:
- medicinal method - consists of prescribing painkillers and anti-inflammatory drugs, as well as drugs that activate metabolism in tissues. Some Patients are additionally prescribed vitamin complexes and sedatives;
- physiotherapy – electrophoresis and UHF therapy;
- surgical intervention is a rather risky method and is used exclusively in advanced stages of the disease.
If you experience any discomfort in the jaw area, you should immediately visit a gnathologist to prevent the development of such an unpleasant disease as Costen syndrome.
Diagnostics
To determine Costen's syndrome, the dentist must carry out a number of mandatory procedures, since the presence of a variety of symptoms often complicates the diagnosis:
- Examination of the patient and clarification of existing complaints.
- Phalangeal test to detect Costen's syndrome. The essence of the method is that in the absence of disease, during the opening of the oral cavity, the phalanges of three fingers should be located unhindered between the teeth of the opposite jaws.
If this is problematic and only two fingers fit into the gap formed, the dentist concludes that there is temporomandibular joint dysfunction. - Tympanometry of the ear. The examination allows us to identify the presence or absence of middle ear pathologies in order to correctly diagnose the disease.
- An X-ray examination is carried out to determine the condition of the dentition and the structural anomalies present in it.
- Consultation with relevant specialists. To exclude diseases with similar symptoms, an examination by an otolaryngologist, orthodontist, or neurologist may be required.
Indications for compactosteotomy and surgical technique.
In this publication, see photos of tooth protrusion.
Follow the link https://orto-info.ru/zubocheliustnye-anomalii/zubov/kolichestva/skuchennost-i-sposobyi-ustraneniya-problemyi.html if you are interested in methods for treating crowding of the lower row of teeth.
Reasons for development
Dentists still have not agreed on what can trigger the development of the syndrome.
The most common factors contributing to the development of the disease are the following:
- incorrect design of the denture, causing uneven distribution of load during chewing;
- various jaw injuries;
- congenital or acquired pathological bite;
- excessively strong one-time or constant loads on the jaw joint;
- bruxism;
- collagen diseases.
The development of Costen syndrome can be caused by a combination of several factors or by one of the above reasons.
If you find any problems in the operation of the dentition, you should consult a dentist.
How can a pacifier affect a child’s bite, tips for selection and use.
Read here all the most important things about the small vestibule of the oral cavity.
At this address https://orto-info.ru/zubocheliustnye-anomalii/chelyustey/krivaya-ne-prigovor.html we will talk about methods for correcting a crooked jaw.
Risk factors
Dentists note that most often the development of Costen syndrome is observed in patients over 50 years of age. As a rule, the likelihood of its occurrence is higher in women than in men.
People who have a history of the following problems also fall into the risk category:
- injuries of the temporomandibular joints;
- unresolved violation of the structure of the dentofacial rows;
- absence of the last molars in each row;
- osteoarthritis.
Some dentists suggest that genetic predisposition can also become a factor in the development of pathology, however, this assumption has not been proven.
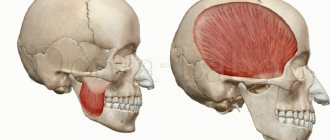
What is the problem
The joint connecting the lower jaw to the base of the skull is formed by the head of the mandibular bone and the fossa of the temporal bone, and is therefore called the temporomandibular joint. There is a disk inside it that divides the cavity into two sections. Thanks to it, the joint moves in three directions and performs the following functions:
- opening and closing the mouth (movement along the frontal axis);
- displacement of the lower jaw forward and backward (sagittal direction);
- lateral movements when chewing (vertical axis).
Although the extreme boundaries of the movements of the lower jaw are controlled by one major and two minor ligaments, when chewing food, speaking and facial expressions, too much load is placed on the joint. Because of this, it may stop performing its functions normally, and then various diseases develop. This may be arthritis, arthrosis, chronic subluxation of the lower jaw or myofacil syndrome, but otoneurological syndrome occurs more often.
The difference between a healthy joint and one affected by arthrosis
results
The duration of the disease until diagnosis ranged from 2 months to 16 years. Pain in the ear/temple/lower jaw area was characterized as aching, pressing and sometimes shooting, provoked by chewing or speech stress and relieved by NSAIDs or local thermal procedures. Congestion in the ear was position-dependent in 12 (27%) patients - 4 patients in each group; Position-dependent tinnitus was present in 3 (7%) patients in group 1 and 1 patient in group 3. Systemic dizziness occurred paroxysmally and was associated with the impact of the joint on the temporal bone or a myofascial trigger in the neck muscles, non-systemic, caused by asymmetric tone of the neck muscles, with head movement. A cracking sound in the ear and clicks in the TMJ (see table) during movement of the lower jaw were noted in all patients.
Complaints and objective symptoms of the examined patients before and after treatment
Note. * — differences are significant compared to groups 1 and 2 (p<0.05).
The triggering factor for the development of CVS in 24 (53%) patients was various dental procedures (extraction, restoration of teeth, installation of fillings, braces, crowns or implants), carried out in the period from 2 weeks to 6 months before the onset of the disease. A frequent trigger for CVS was an acute psychotraumatic situation with a negative emotional background in the future (n=10; 22%).
Pathology of the inner or middle ear was not detected in any patient; 17 (38%) had unilateral or bilateral obstruction of the auditory tube. Hidden unilateral or bilateral asymmetrical spontaneous horizontal nystagmus was detected in 36 (80%) patients (see table) . The examination made it possible to register unilateral or bilateral asymmetric horizontal nystagmus in all patients. MRI of the brain revealed no focal changes in the vestibular nerves and nuclei, cerebellum and cerebellopontine angle.
A neurological examination did not reveal any motor or sensory disorders or dysfunction of the cranial nerves. All patients performed coordination tests confidently, however, in the Romberg test, 11 (24%) patients were unstable; during tests with head turns, instability was recorded in 17 (38%). Manual testing made it possible to identify pain triggers in the neck muscles and masticatory muscles in all patients (see table) , and triggers, the compression of which caused the appearance of ear noise, a change in its intensity or tone, dizziness of a systemic or non-systemic nature, were found in 21 (47%) and 27 (60%) of those examined, respectively. In 16 (36%) cases, an ascending or mixed type of postural dysfunction was determined, and therefore the patients underwent individual foot orthoses.
As a result of the course of treatment in group 1, there was a decrease in the intensity of the pain syndrome according to VAS, a decrease in the frequency of ear noise with unchanged intensity, dizziness and nystagmus, signs of TMJ dysfunction (all differences are significant, p <0.05) (see table) . All types of muscle triggers were inactivated, but the degree of maladjustment associated with dizziness and personal anxiety did not change significantly. Symptoms resumed after 1.5-2.5 months, which was apparently determined by the persisting pathological relationships of the elements of the TMJ and the occlusal discrepancy of the dentition.
In group 2, therapy led to a decrease in the intensity of pain (see table) , tinnitus and dizziness, signs of TMJ dysfunction, but to a lesser extent than in group 1. Painful muscle triggers persisted, as did tinnitus and dizziness triggers. Hidden spontaneous nystagmus was detected with the same frequency, while nystagmus during the head shaking test was recorded 2 times less often than before treatment. The degree of maladaptation, personal and situational anxiety remained almost at the original level. The achievement of the effect was hampered by the preservation of hypertonicity of the masticatory muscles.
Combined treatment in the 3rd group made it possible to achieve significant results that differed significantly not only from the initial level, but also from the final indicators in the 1st and 2nd groups (see table) : in all 15 patients, facial and parotid pain were relieved and dizziness, spontaneous nystagmus regressed, all types of triggers in the masticatory muscles were completely inactivated. Only 1 patient retained tinnitus (less intense than before treatment) and nystagmus during the head shaking test; in this case, signs of TMJ dysfunction remained. The degree of maladjustment associated with dizziness and situational anxiety decreased to normal values (p<0.05).
According to the control MRI of the TMJ, no changes in the condition of the TMJ were recorded in group 1. In group 2, complete restoration of the relationships of the articular structures was achieved in 3 (20%) cases, partial - in 8 (53%); and only in the 3rd group the full effect was achieved in 14 (93%) patients.
Price
The cost of eliminating Costen syndrome depends on the severity of the pathology and treatment methods:
| Procedure name | Cost of carrying out, rub. |
| Fluctuarization | 800—1700 |
| Electrophoresis | 900—2700 |
| Diadynamic therapy | 500—1500 |
| UHF therapy | 600—1500 |
| Acupuncture | 3 000—4 000 |
| Massage | 1 700—3 200 |
| Surgery (arthroplasty) | 55 000—100 000 |
The large difference in prices is explained by the location of the clinic, the professionalism of the staff and the average cost of similar services in different cities of the country.
Additional information about the temporal joint anomaly is presented in the video.