How are cementum, tooth sensitivity and periodontitis related?
Loss of cementum contributes to a number of dental problems, such as tooth sensitivity, loss of enamel, and gum recession . When cementum is lost, the dentin underneath is exposed, and this, in turn, can cause tooth sensitivity. The latter manifests itself as short-term or acute pain in the area of one or more teeth. If you've ever winced and winced painfully after taking a sip of cold water or juice, you know the feeling!
While cementum loss can trigger the development of some dental diseases, other dental diseases can trigger cementum loss. Such diseases include, for example, periodontitis. Cementum loss occurs when there is irreversible damage to the bone and connective tissue fibers that hold the tooth in place. Such damage to bone tissue and cement is characteristic of progressive periodontitis and leads to tooth mobility, which in some cases even has to be removed.
Fixing crowns using a screw method: are there any disadvantages?
The peculiarity of this method is that the abutment is not used as part of the structure, and the crown is screwed to the implant directly, using a screw. In this case, the prosthetist pre-fabricates a special crown with a hole for the screw. It would seem fast and reliable, why not? However, this fairly advanced technology is not without its drawbacks, in particular:
- aesthetic. It will not be possible to preserve the integrity of the crown covering the tooth: the shaft through which the fastening element passes will have to be closed with a composite filling. On the front teeth it will most likely be visible, so the patient will have to give up the dream of a perfect smile;
- functional. Due to the nuances of installation, the hole may occur in an area that is constantly under load, for example, on the cutting edge or masticatory tubercle. In this case, chips, cracks and gradual “eating” of the filling composite material are possible.
In addition, the manufacturing process of bridges for implant-supported prosthetics often involves minimal inaccuracies. When using dental cement in this case, correction can be carried out using a solution.
But in the process of screw fixation, with visually imperceptible inaccuracies, there is a risk of “attracting” the crowns by excessively screwing in the screw. What does this mean? At best, it will result in unpleasant sensations of tension in the patient’s oral cavity; at worst, it will result in a broken fastener, which will then have to be removed from the implant, which is a rather complicated procedure.
What other problems are associated with dental cement?
In addition to the loss of cementum, which can be the result of periodontitis and at the same time cause tooth sensitivity, there are several other dental problems directly related to the condition of this tissue.
Cementoblastoma
This long word refers to a rare benign tumor on the root of a tooth. It occurs when specific cells, cementoblasts, grow in the area of the root apex. Typically, cementoblastoma affects one tooth root, but sometimes it can develop on several roots and spread to the surrounding bone. The growth of cementoblastoma is sometimes accompanied by dull pain, but often the disease is asymptomatic. Being a benign tumor, cementoblastoma, however, is constantly increasing in size; Over time, it can begin to interfere with the normal functioning of the teeth and affect the patient's appearance.
Adolescents and young adults under 30 years of age are at higher risk of developing cementoblastomas. Treatment of cementoblastoma involves surgical removal of the tumor and the affected tooth, which most often turns out to be a premolar or molar of the lower jaw. Sometimes several teeth have to be removed. Although tooth extraction is by no means the optimal solution, the risk of tumor regrowth makes it necessary. Although cementoblastoma is a rare condition, it is best to make sure that pain or strange thickening in the area of the tooth roots is not associated with it. To do this, you should contact your dentist.
Exposure of the cemento-enamel junction (CEJ)
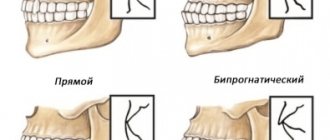
The cemento-enamel junction is a special zone around the perimeter of the tooth where the enamel covering the crown meets the cement protecting the root. In most cases, the cement partially extends onto the enamel, covering it, but in some people there is a thin strip of unprotected dentin between the hard enamel and the less mineralized cement.
sensitivity to cold and hot foods may occur The exposure of the CEJ is associated with recession, that is, drooping of the gums.
To confirm that the sensitivity is caused by gum recession, the dentist will need to measure how much the gums have receded. To do this, use a special tool, a periodontal probe, which the dentist inserts between the gum and tooth. This examination will determine whether the periodontal ligament is in good condition or whether there is a risk of infection, inflammation and further gum recession.
Hypercementosis
Hypercementosis is the process of formation of an excessively thick cement layer on the roots of teeth. Local thickening of the cement leads to a change in the size and shape of the root, which in some cases even begins to interfere with neighboring teeth.
Although the exact causes of hypercementosis are unknown, dentists typically diagnose it in patients with certain medical conditions, such as arthritis, rheumatoid arthritis, acromegaly, and Paget's disease. Researchers have also associated hypercementosis with vitamin A deficiency. Hypercementosis also occurs in patients with periodontal disease or dental trauma caused by occlusal disorders. For the most part, hypercementosis occurs in adults, and the risk of developing it increases with age.
That's how many new words you learned today! Of course, this amount of information is difficult to digest at once, but understanding the important role of cement will help you take a more responsible approach to protecting your teeth. Start with proper oral care to avoid lost or damaged cementum. By regularly brushing your teeth and using dental floss, an interdental brush or irrigator, and an antiseptic mouthwash, you can maintain the health of your teeth and all their tissues.
Securing crowns with cement: technology features, pros and cons
The traditional method used by dentists at the start of prosthetics with implants and which has not lost its relevance to this day is as follows.
After comprehensive preparation of the oral cavity in general and the area for dental implantation in particular, the patient is implanted with an implant simulating the root of a tooth, onto which an add-on is installed - an abutment. And already on the abutment, using the same technology as on your own tooth, a crown is installed, fixed with cement.
Among the advantages of this method, it should be noted, first of all, affordability, ease of implementation and preservation of the integrity of the crown. The disadvantages of fixing a crown to an implant using dental cement are:
- entry of excess solution formed during fixation due to extrusion into the space between the gum and abutment. It is impossible to notice this process from the outside, so neither the patient nor the dentist can be sure that the cement has not entered the gum. In this case, there is a risk of inflammation of the bone tissue adjacent to the implant - peri-implantitis. Treatment of such a disease is long, complex and not always successful. A negative prognosis is the loss of the implant and part of the bone tissue, after which it will require its augmentation, and then re-implantation;
- If at least minimal inaccuracies were made when taking an impression and making the crown, its fit to the abutment will not be tight, which means that the dental cement filling this gap will be washed away by saliva over time. Its place will be taken by soft plaque containing pathogenic bacteria. As a result of decementation, the crown will simply fall out, and due to the action of bacteria, the previously mentioned peri-implantitis may begin to develop, followed by loss of the implant and bone mass.
Characteristics of the main properties of zinc phosphate cement
Characteristics of the main properties of zinc phosphate cement
Zinc phosphate cements acquire their basic properties during their setting reaction and subsequent hardening. These properties further determine the effectiveness of the material. The most important properties of zinc phosphate cements are recorded in the above requirements of the international standard.
Consistency and film thickness . Depending on the purpose, there are two main consistencies of cement: type I - for fixing inlays and type II - for preparing gaskets or fillings. The third consistency of zinc phosphate cement, which is intermediate between the two above, is used for retention of orthodontic appliances and is called consistency for fixation of appliances.
The consistency for fixing inlays is also used for fixing various types of fixed dentures. Although the term “cement” usually implies adhesiveness, phosphate cements do not have this after complete hardening. If unhardened zinc phosphate cement is a rather sticky viscous substance, then the retention properties of hard cement are based only on the mechanical adhesion between the heterogeneous surface of the wall of the carious cavity of the tooth and the filling.
The thickness of the zinc phosphate cement film is a determining factor in the fit of the inlay to the tooth wall and its marginal adaptation. The value of the inlay holding strength also depends on the thickness of the film. According to the international standard, zinc phosphate cement in inlay luting consistency (type I) has a maximum thickness of 25 microns. The thicker the consistency, the greater the thickness of the film and the less tight the seal is. Thus, the adaptation of orthodontic appliances to the tooth crown is a decisive moment in maintaining the appliance; The space between the tooth and the appliance is larger compared to the space between the cavity wall and a well-fitted inlay. This large spacing reduces the effectiveness of the thin cement liner. The thick consistency of cement is achieved by increasing the powder:liquid ratio. Ultimately, the film thickness of well-mixed non-clump cement depends, firstly, on the particle size of the powder and, secondly, on the concentration of the powder in the liquid or the consistency of the cement. Film thickness is also determined by the amount of force and the method of applying force to the prosthesis at the time of its fixation. Depending on the type of prosthesis being fixed, cement is squeezed out along the edges of the prosthesis. Fixation of a full crown is currently the greatest problem, since maximum cement extrusion occurs.
Obviously, the consistency of the zinc phosphate cement used to secure dentures is very important. An increase in the amount of powder introduced into the liquid leads to a thicker consistency of the cement mass. The diameter of the formed disk with a total load of 120 g per 0.5 ml of freshly mixed cement volume varies significantly depending on the powder:liquid ratio. Thicker than normal consistency cement for fixing inlays is more difficult to squeeze out, and this can lead to loose fixation of the inlay or crown. The final consistency should be so liquid that when taken from the plate with a spatula, the cement stretches at a distance of 2-3 cm from the mass behind the spatula.
The thicker consistency of zinc phosphate cement (Type II) is used for a dual purpose: as a thermal and chemical insulator between the deep layers of dentin and the permanent filling material, and also as a fairly durable temporary filling material. Such cement is more resistant to dissolution by saliva, abrasion during chewing and other oral factors over time. Cement in consistency for lining or filling is obtained by using a higher powder:liquid ratio than is usually used for fixing various inlays and devices. Although the technique for mixing cement with a cushioning consistency is similar to that described previously, larger amounts of powder may need to be introduced slightly longer than the usual 90 seconds.
Hardening time. The hardening time of cement is as important for the characteristics of cement as consistency. After mixing, there must be an appropriate period of time to apply and finalize the cement along the edge of the inlay, or fix the orthodontic appliance, or process the spacer and contour of the temporary filling. This time is called hardening time. According to the international standard, it is 5-9 minutes at a temperature of 37°C. The first 1.5 minutes are spent mixing the powder and liquid.
The hardening time of cement in a consistency for fixing devices or a spacer consistency is slightly less than that of cement in a consistency for fixing, because a larger amount of powder accelerates hardening.
The rate of hardening of zinc phosphate cement is influenced by several factors, which are adjusted during the production process or in the clinic during mixing. During the production process, these are the following factors: composition of the powder, degree of firing, particle size, buffering capacity of the liquid, water content in the liquid. In the clinic, the rate of hardening is controlled by the powder:liquid ratio, powder injection rate, mixing temperature, mixing method, absorption or evaporation of water from the liquid.
The curing time of zinc phosphate cement reflects the rate of reaction between the powder and liquid, usually measured from the moment mixing begins. The faster the reaction rate, the shorter the hardening time.
The powder into the liquid must be introduced over a short period; this prolongs the hardening time. The reactivity of the material is also reduced by introducing buffer compounds into the liquid during production. This procedure is not universally effective and depends on the composition of the liquid powders.
Strength. The compressive strength of zinc phosphate cement depends on the initial composition of powder and liquid, the powder-liquid ratio, the mixing method and the technique of applying the cement.
According to the requirements of the international standard, the minimum compressive strength of cement after 24 hours should be 700 kgf/cm2. The strength of zinc phosphate cement increases quickly. Thus, in a fixing consistency, the strength after 1 hour is 2/3 of the final strength.
Proper mixing technique ensures an optimal powder-liquid ratio to obtain the required cement consistency, and this increases the compressive strength of the cement mass. Cement in the laying consistency is more resistant to destruction than in the fixing consistency. The powder-liquid ratio increases, but with an excessive amount of powder, the strength does not increase, since a significant excess of unreacted powder is formed.
Solubility and disintegration. The reaction of liquid and powder of zinc phosphate cement occurs in a relatively short time. Premature contact of water with cement, before the reaction completes and hardening occurs, leads to partial dissolution and leaching of the liquid from the cement. Therefore, when applying a cement spacer, or fixing fixed dentures and orthodontic appliances, it is necessary to carefully isolate the surface of the cement during the hardening process.
Prolonged contact with moisture of well-hardened cement leads to erosion and extraction of soluble substances from the cement. According to the requirements of the international standard, a maximum of 0.2% reduction in mass is allowed for samples in the form of disks with a diameter of 20 mm, having 1260 mm2 of open surface. The discs are kept for 24 hours in distilled water at 37°C. The consistency of filling cement, with a high powder-to-liquid ratio, causes a significant loss of material in the oral cavity over time. All this indicates that zinc phosphate cement can only be used as a temporary filling material. Abrasion, grinding and food influences accelerate the disintegration of zinc phosphate cement in the oral cavity. Greater resistance to dissolution and destruction is achieved by increasing the powder:liquid ratio. A thicker mass of cement is less susceptible to dissolution and destruction than a liquid mass.
It is interesting to compare the solubility of zinc phosphate cement and silicates under real conditions. Long-term observations have shown that in the oral cavity, silicates retain their properties and qualities as fillings for a longer time than zinc-phosphate cement, although the solubility of silicates in laboratory conditions is higher. The reason for this difference in the clinical effectiveness of zinc phosphate cement and silicate is the difference between active resistance to dissolution in the oral cavity and disintegration in distilled water in vitro.
Acidity. During the formation of zinc phosphate cement, when the powder and phosphoric acid liquid are mixed together, a change in pH occurs. At the beginning of mixing, the pH increases relatively quickly, reaching 4.3 after 15 minutes from the start of mixing. By the end of the 1st hour, this value increases to 6.0 and becomes close to neutral after 48 hours. Increasing the powder-liquid ratio at a standard consistency leads to a thicker mass of cement, but has little effect on both the rate of change in pH and the its 48-hour value. Along with this, the liquid mass of zinc phosphate cement, obtained at a lower powder:liquid ratio, has a slower rate of pH increase.
It is obvious that during cementation of inlays and placement of a cement liner, the existing acidity poses a potential danger to the pulp. Experimental studies show that the initial acidity of zinc phosphate cement at the time of its introduction into the tooth cavity can cause changes in the pulp, especially if a thin layer of dentin remains between the cement and the pulp. Therefore, to isolate pulp in deep cavities, thin polymer varnishes, calcium hydroxide and suspensions of zinc oxide or zinc oxide eugenol are used.
Significant decalcification that occurs under orthodontic appliances when using zinc phosphate cement is associated with the loss of fixing material between the appliance and the tooth, the result of exposure to dental plaque microorganisms. At the same time, it is likely that part of the decalcification may be due to the low initial acidity of the standard cement consistency and especially with a very liquid consistency with a low powder-liquid ratio.
Thermal and electrical conductivity. One of the main purposes of zinc phosphate cement is its use as an insulating gasket under metal fillings and inlays. Research has shown that cement used as a liner is an effective thermal insulator, although no more effective than dental dentin. If the presence of liquid does not significantly affect the thermal conductivity of cement; then the presence of moisture in clinical conditions reduces the electrical insulating properties of the material.
Clinical practice has shown that a zinc phosphate cement liner is especially desirable for protection against thermal trauma to the pulp when there is significant dentin loss associated with caries or resulting from trauma.
Methodology for using zinc phosphate cement in a laying consistency. Phosphate cements are mixed with a well-chromed or nickel-plated metal spatula on the smooth surface of a glass plate at a temperature of 18-20°C. The taken amount of powder is divided into four parts, one fourth is divided in half, and one eighth is divided in half again. The mixing process should begin immediately after applying the liquid. First, mix a quarter of the powder with the liquid, thoroughly mixing the mass on a small area of the plate with rubbing linear movements of a spatula, and then collect the mixture in one place. Having obtained a homogeneous mass, add sequentially, thoroughly mixing, the fourth, eighth and sixteenth shares of the powder. Mixing time should not exceed 1 1/2 minutes. The consistency of the cement mass for applying the gasket is considered to be prepared correctly if, when the spatula is torn off, it does not stretch, but breaks off, forming teeth no more than 1 mm high. Liquid should not be added to a thickly mixed mixture, but a new portion should be prepared.
Phosphate cement in a plastic state is introduced in 1-2 portions with careful condensation to the walls of the formed cavity. To make the cement stick less to the plugger, it is advisable to pre-treat the tool with alcohol. When applying the gasket, the consistency of the mass should be such that, during condensation, the permanent filling material (amalgam, Gallodent-M, etc.) is somewhat pressed into the cement, but the gasket should not be squeezed out and protrude onto the surface of the tooth. Care must be taken to ensure that no saliva gets into the cavity when applying the pad.
Before applying a permanent filling, use a sharp excavator or fissure bur to free the edges of the cavity from phosphate cement. Before applying a permanent filling, it is advisable to dry the cavity with warm air.
Hydrophosphate cement. Hydrophosphate cement is known, or as it is also called, water-hardening cement. Hydrophosphate cement was first proposed in 1963 in Japan, and in 1968 in the USA. Its liquid is water (hence the name cement), but about 35% phosphate anhydride is added to the powder composition. After combining with water, phosphoric acid is formed, which causes the hardening reaction. The main purpose of cement is the same as conventional zinc phosphate cements - fixation of fixed dentures and application of a spacer. The physical and mechanical properties of hydrophosphate cement, determined by the methods used for zinc phosphate cement, are slightly lower than the corresponding values of compressive strength, film thickness, solubility and disintegration. The acidity of such cements is close to the acidity of zinc phosphate cements, therefore, in deep carious cavities it is advisable to use an appropriate cavity varnish or a therapeutic lining. Although hydrophosphate cements are of some interest, they do not offer clinical advantages over zinc phosphate cements and therefore are not widely used.
Bactericidal and modified cements
— Unitem (Vladmiva) is a universal, improved zinc-phosphate dental cement with high mechanical strength and chemical resistance. The powder consists of zinc oxide, with modifying additives, and the liquid consists of orthophosphoric acid of reduced activity.
— Unicem bactericidal (Vladmiva) is a universal improved zinc-phosphate dental cement containing the optimal amount of a bacteriostatically effective form of silver. Used in pediatric dentistry for filling temporary teeth.
— -Adhesor (Spofa Dental) – zinc-phosphate cement, Adhesorfine (Spofa Dental) – modified zinc-phosphate cement with a fine structure.
— Phosphate cement containing silver. To improve the bactericidal properties, silver (1.547%) is added to the powder composition. The material is recommended as an insulating gasket when filling molars with metal and other fillings, for filling canals, in pediatric dentistry for filling temporary teeth. Analogs: Bactericidal Unitem (Vladmiva).
— Visphat cement refers to zinc phosphate cements. Its powder contains about 3% bismuth oxide. It hardens faster, is stronger than phosphate cement, and is less soluble. It is used as an insulating lining when filling teeth with metal fillings, silicate cements, acrylic and epoxy resins.
— Dioxyvisfate Dioxidine is included in the composition of this cement. Dioxyvisfate powder is a mixture of visfate and dioxidine, the liquid is orthophosphoric acid, partially neutralized with zinc oxide and aluminum hydroxide. Cement has bactericidal properties, has high mechanical strength, is slightly soluble, and is intended for filling temporary teeth, as a therapeutic and insulating spacer, for fixing inlays, pin teeth, and bridges.
Homework to understand the topic of the lesson:
Control questions:
1. What is the chemical composition of zinc phosphate cement powder and liquid?
2. What is the chemical composition of polycarboxylate cement powder and liquid?
3. What is the purpose of zinc phosphate cements?
4. What is the purpose of polycarboxylate cements?
5. Name the materials from the group of zinc-phosphate cements of domestic and foreign production.
6. Name the materials from the group of polycarboxylate cements of domestic and foreign production.