Composition and properties
Borax in glycerin is an antiseptic, which in pharmacology is called sodium tetraborate. The drug is based on boric acid.
It is used in the pharmaceutical, perfume, cosmetology and food industries. Borax in glycerin is available in the form of a solution of 5, 10 and 20% concentration. The duration of treatment with the drug is determined by the attending physician.
During pregnancy, borax in glycerin is prescribed in the form of a 5% solution. The same concentration of the drug is indicated for the treatment of oral thrush in a newborn.
The taste of the drug is neutral. It is not recommended to administer a more concentrated solution to expectant mothers, as it may have a toxic effect and cause side effects in a pregnant woman.
Borax in glycerin simultaneously has antifungal, antiseptic, anti-inflammatory, antibacterial and insecticidal effects.
What diseases of the intimate area can occur during pregnancy?
Often, during pregnancy, the expectant mother is bothered by irritating discharge with an unpleasant odor, itching, and dryness. The cause may be one of the following infections:
- thrush.
Its appearance is caused by the proliferation of yeast fungi on the mucous membrane of the intimate area. The infection can be transmitted to the child during childbirth, affecting the mucous membranes of the mouth and genitals; - bacterial vaginosis.
Caused by pathogenic bacteria and manifests itself in the form of gray discharge with an unpleasant odor; - urinary tract infections
. Hostile microorganisms penetrate the urinary organs when urinating from the intimate area. Cutting and burning are the first signs of this condition. This does not harm the baby, but can lead to kidney inflammation, which is dangerous for the expectant mother.
If you see a doctor in time and undergo the necessary treatment, you can avoid dangerous complications.
Indications and method of use
Indications for its use are:
- thrush or vaginal candidiasis; Read more: thrush during pregnancy→
- treatment and prevention of upper respiratory tract diseases;
- skin irritation, diaper rash;
- prevention of mosquito and tick bites.
To use borax in glycerin to treat thrush, you need to take a sterilized gynecological syringe, draw a small amount of medicinal solution into it and douche the vagina.
If you don’t have a syringe, you can apply the drug to a self-made cotton-gauze swab and insert it into the vagina for 30-60 minutes, depending on the doctor’s recommendation. It is advisable to carry out manipulation with the introduction of a tampon while lying down.
Some women simply soak a sterile bandage in borax with glycerin and wipe the vaginal walls and external genitalia, trying to remove all the characteristic plaque from a fungal infection. In principle, this method is also acceptable, but its effectiveness will be several times lower, since the active substance, boric acid, comes into contact with the mucous membrane for a short time.
Treatment of the mucous membranes of the genital organs can be carried out only after their hygiene. It is not recommended for expectant mothers to get carried away with douching, so to cleanse the intimate area, it is enough to use a weak solution of potassium permanganate or chamomile decoction.
The duration of the course of treatment and the frequency of procedures is determined by the doctor. Usually, with advanced thrush, douching or inserting tampons is carried out 3 times a day; after the symptoms of the disease improve, the number of procedures is reduced to one. The average course of treatment does not exceed one week.
Borax in glycerin quickly and permanently eliminates itching and hyperemia of the external genitalia and relieves discomfort. After a few days, the symptoms of vaginal candidiasis may disappear completely, but there is no need to refuse further treatment if it was recommended by your doctor.
It is important to complete all procedures to avoid remission of the disease.
This remedy cannot completely get rid of thrush, since it acts locally, only at the source of infection, but it can effectively stop the growth and multiplication of a fungal infection.
During pregnancy, this drug can become a real lifeline when the use of other medications is undesirable.
Vaginal candidiasis and pregnancy
IN
Currently, the frequency of purulent-inflammatory diseases in obstetrics does not have a clear tendency to decrease. In many countries of the world, including Russia, there has been an increase in vaginal infections, which firmly occupy a leading place in the structure of obstetric and gynecological morbidity [1, 2].
The introduction of modern technologies into clinical microbiology has made it possible to expand research and show that the negative impact of environmental factors on the microflora of the macroorganism leads to a variety of pathologies of both inflammatory and non-inflammatory origin. Despite significant advances made in the diagnosis, treatment and prevention of vaginal dysbiosis, their frequency does not have a clear downward trend. The latter is also associated with the increase in immunodeficiency conditions against the backdrop of deteriorating environmental conditions, poor nutrition, frequent stress, and uncontrolled use of medications, primarily antibiotics. Most often, sexually transmitted infections are caused by several pathogenic factors - viruses, microbes, fungi, protozoa, which cause diseases that are similar in clinical course, but different in pathogenesis and treatment methods.
Vaginal infections are of particular importance in obstetric practice, as they are a common cause of inflammatory complications during pregnancy, childbirth and the postpartum period. Complications of the gestational period and childbirth associated with various disorders of the vaginal microcenosis include the threat of miscarriage, spontaneous miscarriages, premature birth, chorioamnionitis, untimely rupture of amniotic fluid, the birth of children with low body weight, chronic hypoxia and/or signs of intrauterine infection, the occurrence of wound infection birth canal, endometritis in the postpartum period.
Violation of vaginal microcenosis is most often associated with candidiasis infection. According to the literature, 75% of women of reproductive age experience at least one episode of vaginal candidiasis [3]. There are currently 196 known species of fungi of the genus Candida.
.
Of these, more than 27 species are isolated from human mucous membranes. According to summary data, Candida albicans
is found in the intestines of 20–50% of healthy people, on the oral mucosa in 20–60%, and in the vagina in 10–17% of non-pregnant women. Vaginal candidiasis in pregnant women occurs on average in 30–40% of cases, and before childbirth – up to 44.4%.
| 75% of women of reproductive age experience at least one episode of vaginal candidiasis. |
It should be noted that genitourinary candidiasis is 2-3 times more common during pregnancy than in non-pregnant women.
Such a high incidence of vaginal candidiasis during gestation is due to a number of factors: changes in hormonal balance; accumulation of glycogen in the epithelial cells of the vagina; immunosuppressive effect of high levels of progesterone and the presence of immunosuppressive factor associated with globulins in the blood serum. A direct relationship has been established between gestational age and the incidence of vaginal candidiasis. The main role in the occurrence of vaginal candidiasis belongs to fungi of the genus Candida albicans
, isolated in 95% of cases. Vaginal candidiasis during pregnancy is characterized by an asymptomatic course and frequent relapses. Due to the increasing number of risk factors and the wide spread of candidiasis infection, the emergence of new data on pathogenesis against the background of immunodeficiency states, the issues of prevention and treatment of candidiasis currently pose a very complex problem [1, 4, 5]. This problem becomes especially important during gestation due to the high risk of fetal damage. Pregnant and postpartum women with vaginal candidiasis can be a source of both intrauterine and postnatal infection of newborns. Over the past 20 years, the incidence of candidiasis among full-term newborns has increased from 1.9% to 15.6%.
It is important to know the pathogenesis of this infection. In the development of candidiasis, the following stages are distinguished: attachment (adhesion) of fungi to the surface of the mucous membrane with its colonization, penetration (invasion) into the epithelium, overcoming the epithelial barrier of the mucous membrane, entry into the connective tissue of the lamina propria, overcoming tissue and cellular protective mechanisms, penetration into blood vessels , hematogenous dissemination with damage to various organs and systems.
With vaginal candidiasis, the infectious process is most often localized in the superficial layers of the vaginal epithelium. At this level, the infection can persist for a long time due to the emergence of a dynamic equilibrium between fungi, which cannot penetrate into the deeper layers of the mucous membrane, and the macroorganism, which restrains them but is not able to completely eliminate the pathogen. Violation of this balance leads either to an exacerbation of the disease, or to remission or recovery.
Depending on the state of the vaginal microcenosis, 3 forms of Candida
– vaginal infections:
1. Asymptomatic candidiasis
, in which there are no clinical manifestations of the disease, yeast-like fungi are detected in a low titer (less than 104 CFU/ml), and lactobacilli absolutely dominate in the microbial associates of the vaginal microcenosis in moderately large quantities.
2. True candidiasis
, in which fungi act as a monopathogen, causing a clinically pronounced picture of vaginal candidiasis.
At the same time, in the vaginal microcenosis, Candida
(more than 104 CFU/ml) along with a high titer of lactobacilli (more than 106 CFU/ml) in the absence of diagnostically significant titers of other opportunistic microorganisms.
3. Combination of vaginal candidiasis and bacterial vaginosis
, in which yeast-like fungi participate in polymicrobial associations as pathogens. In these cases, yeast-like fungi (usually in high titre) are found against the background of a large number (more than 109 CFU/ml) of obligate anaerobic bacteria and gardnerella with a sharp decrease in the concentration or absence of lactobacilli.
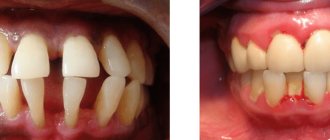
Clinical picture of vaginal candidiasis
usually characterized by the following symptoms:
• copious or moderate curdled discharge from the genital tract;
• itching, burning, irritation in the area of the external genitalia;
• increased itching during sleep or after water procedures and sexual intercourse;
• an unpleasant odor that increases after sexual intercourse.
Currently, it is customary to distinguish 3 clinical forms of genital candidiasis
:
1. Candidate carriers
2. Acute urogenital candidiasis
3. Chronic (recurrent) urogenital candidiasis.
One of the main features of the course of genital candidiasis is the frequent combination of candida infection with opportunistic bacterial flora, which has high enzymatic and lytic activity, which creates favorable conditions for the introduction of fungi into tissues.
Diagnostics
diagnosis of vaginal candidiasis should be clinical and microbiological, and among laboratory methods, priority should be given to the culture of vaginal discharge. This method makes it possible to establish the etiology of the disease, the species of the pathogen and give its quantitative assessment. Cultural examination is the method of choice for monitoring the effectiveness of treatment. Parallel microscopy of a vaginal smear stained with Gram allows one to assess the microflora accompanying the fungi (obligate anaerobes or lactobacilli), on which the choice of rational etiotropic therapy should depend.
Treatment of vaginal candidiasis
Drugs used in pregnant women for the treatment of vaginal candidiasis must meet the following requirements: lack of toxicity to the fetus and mother, high efficiency, good tolerability, minimal incidence of resistance in pathogens, etc. Intravaginal use of antimycotics should be considered preferable due to the very low systemic absorption of drugs, which minimizes the possibility of undesirable effects [1, 4]. In addition, a decrease in clinical symptoms and recovery occurs faster. There are many medications and treatment regimens for vaginal candidiasis during pregnancy. However, there is no optimal drug yet that would meet all the requirements and be 100% effective.
Drugs for the treatment of vaginal candidiasis
are divided into the following groups:
• antibiotics (nystatin, levorin, pimafucin, amphotericin B);
• imidazoles (clotrimazole, ketoconazole, miconazole, gino-pevaril);
• triazoles (fluconazole, itraconazole);
• combination drugs (Polygynax, Klion D, Pimafukort, Macmiror complex);
• drugs of different groups (dafnedzhin, polyvinylpyrrolidone iodate, griseofulvin, flucytosine, nitrofungin).
In the treatment of vaginal candidiasis, the effectiveness of clotrimazole is 70–82%, miconazole - 80%, ketoconazole - 68%, polygynax - 85.5%, gino-pevaril - 86.7%, dafnedzhin - 93.5%, fluconazole - 93.3 % [1, 3, 4, 5]. However, the use of some antifungal drugs (for example, fluconazole) due to their possible teratogenic effects during gestation is contraindicated.
, pimafucin has become widely used for the treatment of vaginal candidiasis during pregnancy.
(natamycin), which is an antifungal polyene antibiotic from the macrolide group with a wide spectrum of action.
It has a fungicidal effect. Natamycin binds sterols of cell membranes, disrupting their integrity and functions, which leads to the death of microorganisms. Most yeast-like fungi are sensitive to natamycin, especially Candida albicans
; dermatophytes are less sensitive to this drug. Important characteristics of the drug are the absence of resistant strains, as well as the absence of toxicity, which allows its use at any stage of pregnancy and lactation.
Clinical trials of the drug were carried out in the treatment of a large number of patients suffering from cervicovaginitis and vulvovaginitis caused by protozoa and fungi. The effectiveness of pimafucin was proven; in all studies, a high percentage of complete recovery was noted with the disappearance of clinical symptoms and normalization of the results of bacterioscopic and bacteriological tests.
Using pimafucin for the treatment of vaginal candidiasis in pregnant women over the past 5 years, we have confirmed its high effectiveness and safety. At the same time, the principle of an individual approach to each pregnant woman was observed, taking into account the gestational age, clinical form of the disease, and the results of microbiological analysis. Pimafucin was prescribed after 12 weeks of gestation, for acute form of VK - 1 vaginal suppository (100 mg natamycin) once a night for 6 days, for relapse of chronic infection - in the same dosage, lasting 9 days. At the same time, they warned about the need for treatment for the spouse (for example, 2% pimafucin cream - topically). Data from a survey of patients showed that already on the 2nd–3rd day of treatment there was an improvement in their condition. After completing the course of therapy, the vast majority (94%) of pregnant women showed improvement. Clinically, it was expressed in the disappearance of discharge, hyperemia and swelling of the vaginal mucosa, burning sensation and itching. Mycelium threads and yeast cells were not found in smears and bacteriological culture. In vaginal smears, leukocytosis was up to 8–10 per field of view.
Thus, pimafucin is a highly effective antifungal drug for the treatment of vaginal candidiasis during pregnancy, which does not have a negative effect on the condition of the fetus and newborn.
Natamycin -
Pimafucin (trade name)
(Yamanouchi Europe)
Literature:
1. Prilepskaya V.N., Ankirskaya A.S., Bayramova G.R., Muravyova V.V. Vaginal candidiasis. // M.: 1997.– 40 p.
2. Mardh PA The vaginal ecosystem. // Amer. J. Obstet. Gynecol. – 1991. – Vol. 165, No. 4, Rt. 2. – P. 1163–1168.
3. Perry S., Whittinton R., McTavish D. Fluconazole. An update of its antimicrobial activity, phannacokinetic properties and therapeutic use of vaginal candidiasis. // Drugs.–1995.– Vol. 49. No. 6. – P. 994–1006.
4. Akopyan T.E. Bacterial vaginosis and vaginal candidiasis in pregnant women (diagnosis and treatment): Diss... cand. honey. Sciences. – M. – 1996. – 141 p.
5. Mirzabalaeva A.K. Basic principles of treatment of chronic genital candidiasis in women. // Bulletin of Dermatology and Venereology. – 1994. – No. 2. – P. 20–22.
Is this product safe?
Borax in glycerin is successfully tolerated during pregnancy. But the development of the following side effects is possible:
- local irritation of the skin;
- in case of overdose, it has a toxic effect on the woman’s nervous system, which can manifest itself in convulsive syndrome.
If, after using borax in glycerin as a douche or inserting a tampon, a woman experiences a burning sensation, she must immediately stop contact of the mucous membranes with the drug and rinse them thoroughly with running water.
The same can be advised in case of diarrhea and twitching of the muscles of the face and limbs - most likely, the drug is not suitable for a woman, you should immediately stop using it and seek advice from a doctor.
You also need to remember that sodium tetraborate can accumulate over time in bone tissue and in the liver, causing a damaging effect on them.
To avoid this, you should not abuse the use of borax in glycerin and allow an overdose of the drug, and also use it for people known to suffer from osteoporosis and liver pathologies.
What kind of drug is this
Sodium tetraborate in glycerin, popularly known as borax in glycerin, is a drug in the form of a thick solution that has antiseptic and antifungal properties, helping in the treatment of colpitis, stomatitis in newborns, bedsores, etc.
Due to its characteristic insecticidal properties, sodium tetraborate is used to kill small insects and is classified as toxicity class 4 (low-hazard substances). The solution can only be used for external treatment of affected areas.
Contraindications
The use of the drug during pregnancy is permitted, since its absorption into the bloodstream through intact skin is reduced to a minimum.
Therefore, borax in glycerin does not negatively affect the development of the fetus and the course of pregnancy. But if the expectant mother has damage to the vaginal mucosa, cervical erosion or fissures, the use of this drug is contraindicated.
This is due to the ability of sodium tetraborate to easily penetrate through microtraumas into the general bloodstream and have a toxic effect on the body. That is why borax in glycerin should be prescribed by the attending physician, who will make sure that the woman has no contraindications.
Sodium tetraborate should also not be used by persons who are hypersensitive to the drug. In addition, borax in glycerin is contraindicated in diseases characterized by metabolic alkalosis - the accumulation of alkaline substances in the blood.
You should immediately seek emergency medical help if the following clinical symptoms occur:
- nausea and vomiting;
- increased sweating;
- dizziness;
- convulsive syndrome, for example, tremors of the limbs;
- rashes or redness of the skin;
- swelling;
- increased heart rate.
It is important to carry out all therapeutic procedures using borax in glycerin after consultation with a specialist in order to avoid possible complications and side effects.
Thrush causes many problems during pregnancy, and if before conception a woman could quickly cope with the infection by drinking one of the modern drugs without thinking about the consequences, then while carrying a child, most modern medications are prohibited.
Borax in glycerin is a complex medicine that is effective against fungal infections, pathogenic microorganisms and insects. During pregnancy, this drug can be used as prescribed by a doctor, taking into account indications and contraindications.
Author: Olga Rogozhkina, doctor, especially for Mama66.ru
When should it not be used?
Local use of the product is allowed at any stage of pregnancy, as it does not enter the bloodstream. For this reason, the drug cannot negatively affect the development of the fetus. But if there is damage to the mucous membrane (cracks, ulcers, erosions), the use of this remedy for the treatment of pregnant women is strictly prohibited.
If there is damage, there is a risk of the drug entering the bloodstream, and in this case, the drug may have a toxic effect on the fetus. For this reason, treatment with borax can only be carried out after consultation with a doctor. In addition, the product is prohibited for use:
- if you are intolerant to the ingredients of the drug;
- in conditions accompanied by metabolic alkalosis - a violation of the acid-base state of the extracellular fluid.
Side effects
When using borax dissolved in glycerin to treat thrush and other diseases, side effects are rare. However, irritation at the application sites cannot be ruled out. Therefore, if after inserting a tampon a burning sensation or other discomfort occurs, you should immediately remove the tampon and stop treatment with this remedy.
But with an overdose or improper use of the drug (for example, when taken orally), the risk of developing unpleasant side symptoms increases significantly. There may be:
- nausea, vomiting and other digestive disorders;
- dizziness;
- convulsive syndromes: nervous tics, hand tremors;
- tachycardia;
- skin rash;
- the appearance of edema.
If any of these symptoms appear, you should immediately seek medical help.
The use of a drug such as sodium tetraborate is ambiguously assessed by doctors. On the one hand, this is a time-tested product that has proven its effectiveness and safety, subject to the rules of use.
On the other hand, today this remedy is considered outdated, since there are more effective drugs approved for the treatment of candidal colpitis in pregnant women. In any case, you should not use the product without consulting a doctor; only a specialist can decide on the advisability of its use.