In surgical dentistry, one of the most common pathologies is osteomyelitis of the jaw - a purulent-necrotic pathological process that affects the bone tissue of the upper or lower jaw. This is a serious disease that, without timely treatment, can lead to serious consequences. Young men under 40 years of age are at risk.
Why this disease develops, how to recognize it in time and what the treatment is - we will look in more detail in our article.
What is it and how to treat it?
Osteomyelitis is an inflammation of the bone marrow with a tendency to progress.
This is what distinguishes it from the widespread dentoalveolar abscess, dry socket, and osteitis seen in infected fractures. Osteomyelitis affects adjacent cortical plates and often periosteal tissues. In the era of preantibiotics, osteomyelitis of the mandible was not uncommon. With the advent of antibiotics, the disease began to be detected less frequently. But in recent years, antimicrobial drugs have become less effective, and the disease has reappeared.
Osteomyelitis of bone: what is it?
Bone osteomyelitis in the concept of general surgery is an inflammation of bone tissue, which has a rather complex pathogenesis. In modern medicine there are many theories of its origin. However, it is impossible to determine the most reliable one, since each of the theories does not exclude the others, but complements them. Thus, osteomyelitis is a multifactorial disease, in the development of which not only the penetration of any infectious agent into the bone tissue plays a major role, but also the state of the human body’s immune system, local circulation disorders with deterioration of trophism.
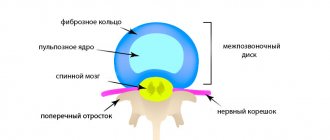
When an infectious agent enters bone tissue, a violent reaction of the body develops, manifested by purulent inflammation. To destroy the infection, leukocytes begin to actively migrate to the site of the lesion, which produce a huge amount of enzymes. They gradually destroy bone structures and form cavities filled with liquid pus, in which pieces of bone or sequestra can be found. Sometimes the inflammation spreads to the surrounding soft tissue, which leads to the formation of fistula tracts that open on the skin.
If the immune system of a sick person is active enough, then inflammation can be limited on its own and become chronic. But if there is an immunodeficiency in the body, then the infection spreads further with the development of severe purulent complications, such as sepsis, which often leads to disability or even death.
Osteomyelitis of the jaw. Causes
In the maxillofacial region, osteomyelitis occurs mainly as a result of the continuous spread of odontogenic infections or as a result of trauma. Primary hematogenous osteomyelitis in the maxillofacial region is rare, usually in very young people. Thus, osteomyelitis of the jaw occurs after tooth extraction, root canal treatment, or with fractures of the upper or lower jaw. This initial lesion leads to an inflammatory process caused by bacteria.
The incidence of osteomyelitis is much higher in the mandible due to the dense, poorly vascularized cortical plates and blood supply. Osteomyelitis of the maxilla is much less common due to the excellent blood supply from several feeding vessels. In addition, the maxillary bone is less dense than the mandibular bone.
Reduced patient protection, both local and systemic, may significantly contribute to the development of osteomyelitis. Osteomyelitis can be associated with a variety of systemic diseases, including diabetes, autoimmune conditions, malignancies, malnutrition, and acquired immunodeficiency syndrome. Medicines associated with the risk of osteomyelitis: steroids, chemotherapy drugs, bisphosphonates. Radiation therapy (causes so-called radiation osteomyelitis of the jaw), osteoporosis and bone pathology can change the blood supply to this area and become a potential springboard for the development of osteomyelitis.
Classification
According to the method of penetration of osteomyelitis infection on both jaws, a classification has been compiled:
- Hematogenous - pathogenic microorganisms move through the blood from other foci of infection. This feature is characteristic of secondary pathology of the upper oral part, which develops against the background of another disease (scarlet fever, diseases of the ENT organs). The bone elements of the oral apparatus are primarily affected, followed by the gingival tissue.
- Odontogenic – infection comes from a tooth, damaged pulp or root (pulpitis, periodontitis, cyst, alveolitis).
- Traumatic – advanced fractures and injuries of the maxillofacial area.
According to the symptoms, the process happens:
- spicy;
- subacute;
- chronic.
By distribution:
- local (with clear boundaries);
- vague (diffuse).
Osteomyelitis of the jaw. Symptoms
Like any infection of the maxillofacial area, osteomyelitis of the lower jaw and osteomyelitis of the upper jaw are accompanied by symptoms:
- pain
- swelling and redness on the surface of the skin
- adenopathy
- heat
- paresthesia of the inferior alveolar nerve
- lockjaw
- malaise
- fistulas
Pain from osteomyelitis is often described as deep and aching, which often does not correspond to the clinical picture.
In acute osteomyelitis, swelling and erythema of the overlying tissues are very often observed, which indicate the initial phase of the inflammatory process in the underlying bone.
Fever often accompanies acute osteomyelitis, whereas it is relatively rare in chronic osteomyelitis.
Inferior alveolar nerve paresthesia is a classic sign of pressure on the inferior alveolar nerve as a result of an inflammatory process in the bone marrow of the mandible.
Trismus may be present due to an inflammatory reaction in the muscles of mastication.
The patient usually experiences malaise or a feeling of general weakness, which can accompany any systemic infection.
Finally, both intraoral and extraoral fistulas are usually present in the chronic phase of maxillofacial osteomyelitis.
Prognosis and possible complications
With timely consultation with a doctor, accurate diagnosis and properly selected therapy, the prognosis is favorable.
Otherwise, the pathological process can spread along the descending and ascending paths. This threatens the development of the following complications:
- Meningitis
- Brain abscess.
- Phlegmon of the orbit.
- Sinusitis.
- Thrombophlebitis of the facial vein.
- Sepsis.
- Lung abscess.
- Mediastinitis.
These conditions have an acute onset and require immediate medical attention. Delay often ends in death for the patient.
The chronic form with sluggish inflammation negatively affects the condition of the soft tissues and bones of the jaw, and is accompanied by:
- fractures,
- deformation of the temporomandibular joint;
- formation of intra-articular adhesions;
- the formation of scar contractures of the masticatory muscles.
These pathologies significantly limit the mobility of the jaw or lead to its complete immobility.
Osteomyelitis of the jaw. Diagnostics
Patients are often given laboratory tests as part of their initial evaluation. In the acute phase of osteomyelitis, leukocytosis with a shift to the left is often observed, which is typical for any acute infection. But leukocytosis is relatively rare in the chronic phases of osteomyelitis.
The patient may also have an elevated erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP). Both ESR and CRP are very sensitive. Almost all patients will undergo maxillofacial imaging.
Computed tomography (CT) has become the standard of care in the evaluation of maxillofacial pathology such as osteomyelitis. It provides a three-dimensional image. CT can provide very detailed images of early cortical bone erosion in osteomyelitis. Often, along with pathological fractures, you can see the degree of damage and bone sequestration. CT scanning, like conventional X-ray examination, shows changes when bone demineralization reaches 30 to 50%, which significantly delays the diagnosis of osteomyelitis. Magnetic resonance imaging (MRI) is generally considered more valuable in assessing soft tissue lesions in the maxillofacial region. However, MRI can help in the early diagnosis of osteomyelitis. Thus, MRI can help in identifying the early stages of osteomyelitis.
Preventive actions
Prevention is important not only to prevent the development of purulent inflammation, but also to minimize the likelihood of complications. With the help of preventive measures, you can also speed up rehabilitation if it was not possible to prevent the disease:
- Timely elimination of carious formations, even if there are no clinical symptoms.
- Sanitation of various foci of infection.
- Physical activity, a balanced and nutritious diet, which contribute to the effective functioning of the immune system.
- Compliance with the doctor’s recommendations after injury, during recovery after surgery or tooth extraction.
In conclusion, I would like to emphasize that although modern medicine has made great progress, osteomyelitis of the jaw bone still remains a serious problem. Thanks to the timely detection of symptoms of pathology and proper treatment, it is possible to significantly increase the likelihood that the patient will be able to fully recover and the quality of his future life will not be affected.
Osteomyelitis of the jaw. Treatment
The first step in treating osteomyelitis is to correctly diagnose the condition. A preliminary diagnosis is made based on clinical assessment and radiological examination.
Treatment of osteomyelitis of the maxillofacial region requires both conservative and surgical methods. In later stages, antibiotic therapy is rarely effective, so the vast majority of cases of osteomyelitis require surgery.
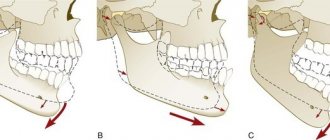
For osteomyelitis of the upper or osteomyelitis of the lower jaw, as a rule, classical treatment is used - sequestrectomy. The goal is to remove necrotic or poorly vascularized bone sequestration in the infected area and improve blood flow. Sequestrectomy involves removing infected and avascular pieces of bone—usually cortical plates—in the infected area. Visual assessment is critical at these stages, but radiation diagnostics, which shows the osseous extent of the pathology, also helps. It is often necessary to remove teeth adjacent to the area of necrosis.
Supporting the weakened area with a fixation device (external fixator or reconstruction plate) is often used to prevent pathological fracture.
What causes the disease
The main culprit of the disease is pathogenic microorganisms. These are mainly streptococci and anaerobic bacteria that are present in the human oral cavity. They are the ones who trigger the infectious process that affects the jaw. But how do pathogenic bacteria get into bone tissue? There are several ways:
- An advanced carious process that has destroyed the hard tissues of the tooth and reached the pulp.
- Tooth injury – crack, filling defect, fracture. But not every mechanical damage will become a source of infection. The damage must be serious and deep. This also includes a broken jaw. But in this case, the inflammation is usually caused by a staphylococcal infection.
- Chronic infectious focus in another organ. Harmful bacteria can make their way to the jaw through the lymph nodes or blood vessels from a nearby organ (ear, throat, nose).
Most often, the disease is diagnosed in the lower jaw, since the teeth of the lower row are more susceptible to caries and various traumatic effects.
The risk of developing osteomyelitis increases in the presence of an immunodeficiency state, as well as diseases of the circulatory system. This is due to the fact that a person with such pathologies has poor wound healing, and the body is not able to resist infections.
Other factors provoking the disease include:
- smoking;
- alcohol abuse;
- diabetes;
- fasting or poor nutrition;
- syphilis;
- chemotherapy courses.
If the acute development of the disease is not completely cured, then chronic osteomyelitis of the jaw develops. It is more difficult to respond to conservative therapy and also more often leads to complications.
Alveolitis
Inflammation of the walls of the socket.
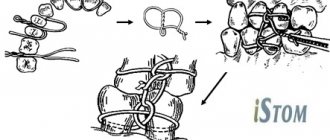
- In the initial stage of alveolitis, an intermittent aching pain appears in the socket, which intensifies while eating;
- The general condition is not disturbed, the body temperature is normal;
- The tooth socket is only partially filled with a loose, disintegrating blood clot.
With further development of inflammation:
- The pain intensifies and becomes constant;
- Transmitted to the ear, temple, corresponding half of the head;
- The general condition worsens, malaise and fever appear.
Development factors
The main causes of the development of the disease are hypoxia, acute respiratory viral infections and infectious diseases, and reduced immunity. Many factors lead to the development of these reasons:
- Spread of infection to bone tissue from nearby foci (gingivitis, caries, pulpitis, etc.).
- Extraction, dental implantation and other traumatic dental procedures.
- Infections that enter the jaw bone by hematogenous or lymphogenous route.
- Therapy with steroids, monoclonal antibodies, bisphosphonates.
- Purulent otitis, tonsillitis and other ENT pathologies.
- Chemotherapy and radiation treatment of oncology.
- Osteoporosis.
- Poor oral hygiene.
- Nutritional deficiency.
- Alcohol or drug addiction.
- Blood diseases.
- Burns and injuries to the jaws.
Treatment with biosphosphonates and monoclonal bodies plays a decisive role in the development of the anomaly. These drugs are intended for the treatment of osteopenia, osteoporosis and are prescribed for cancer.
Prevention measures
In order not to learn from personal experience what osteomyelitis is, you must:
- undergo preventive examinations at the dentist’s office every year;
- promptly treat emerging dental diseases;
- lead a healthy lifestyle;
- Avoid traumatic activities that may result in head injuries.
If the gums become inflamed, the tooth begins to ache, you need to immediately go to the doctor and take an X-ray. The sooner the correct diagnosis is made, the sooner and easier it will be possible to overcome the disease.
General information about the disease
With osteomyelitis, destructive changes in the bone tissues of the oral cavity are observed. It is this diagnosis that most often forces dental surgeons to pick up a scalpel. In terms of prevalence, it can be compared with periodontitis and periostitis.
If the disease is not treated, the bone tissue will bend, become thinner, and become incredibly fragile. Painful fistulas will begin to form. A person will still not be able to tolerate such symptoms for a long time, so there is no need to lead to complications.
General concept
Osteonecrosis of the jaw (ONJ) is a pathological process of death of osteocytes and destruction of jaw bone tissue. Also known as: dead jaw syndrome, avascular or avascular necrosis.
This is a complication of inflammatory diseases of the oral cavity. International classification code – K10.2.
The outcome of the disease depends on the form, degree of development and adequacy of treatment. For mild cases of the disease, it is sufficient to prescribe antibacterial and anti-inflammatory drugs. In severe cases, there is a risk of bone exposure, atrophy and decay of the jawbone, and separation of bone segments. The patient experiences intense pain, loses dental elements, and the functionality of the dental apparatus decreases. In difficult cases, the patient is at risk of disability or death.
The severity of the course is determined by the cause of the development of the pathology. The disease is difficult to diagnose in the early stages.
The risk group includes men under 30 years of age. Fortunately, the disease rarely develops.
Toothache after caries treatment
Constant pain after filling can occur for many reasons. A common cause of discomfort is the application of an insulating lining made of glass ionomer cement (GIC) and filling on the same day with a composite. The polymerization times of GIC and composite differ, which can result in displacement of the gasket and its pressure on the pulp.
If the pain is short-term in nature as a reaction to cold, sour or sweet and quickly passes after removing the irritant, it may be due to the fact that during the treatment there was a mechanical effect on the pulp. After 2-3 days, the pulp will return to normal functioning and the pain will stop.
If you experience pain when biting, you need your dentist to grind the filling to fit your bite.