Indications for treatment of periodontitis
There are two main ways to treat periodontitis: conservative and surgical. Each of them has its own indications and contraindications.
According to modern dental standards, a doctor should give preference to conservative methods. They are indicated for both acute and chronic periodontitis, including the appearance of cysts and granulomas, loose teeth, and increasing inflammation.
However, orthograde treatment cannot be used in all cases. Indications for surgical intervention are:
- obstruction of the tooth root canals;
- the presence of a stump tab or pin that cannot be removed without damaging the roots;
- multiple perihilar cysts or cysts growing into the maxillary sinus;
- wide affected area (over 10 millimeters);
- perforation of the tooth cavity or root wall;
- ineffectiveness of conservative treatment methods.
Important!
When we talk about periodontitis, we often mean apical (also known as periapical or apical) periodontitis - that is, inflammation at the apex of the tooth root. The cause of this disease is endodontic problems. Another type of periodontitis, marginal, affects the gums in the cervical area of the tooth, but it already belongs to the field of periodontology. This material is devoted to the treatment of apical periodontitis only.
Periodontitis: how does the disease appear and how does it develop?
Periodontitis is a term dentists use to refer to an inflammatory process that affects the tissues that surround the tooth and help keep it in the socket. The causes of periodontitis may vary in etiology (origin) and the disease is classified into subtypes. Correct diagnosis of the subtype of periodontitis is of fundamental importance: on its basis, the specialist will select the most effective treatment methods. Below we will get acquainted in detail with the forms of the disease, and also consider in detail their characteristic symptoms.
Infectious periodontitis
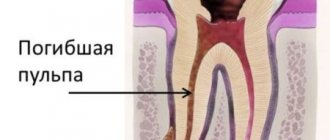
Dentists have to treat the infectious form of periodontitis in 90% of cases. The disease appears due to infection entering the root canals of the tooth and usually against the background of caries or pulpitis, the timely treatment of which was ignored. Infection in the canal cavities can also occur due to errors in endodontic treatment. The inflammatory process begins to actively develop from the moment pathogenic microflora enters the cavity of the dental canal. As inflammation spreads, not only soft but also hard tissues are destroyed; a granuloma can form, and if left untreated, a cyst.
IMPORTANT: The process of cyst formation can be asymptomatic, but the formation can grow to significant and dangerous sizes and lead to various types of pathologies, including deformation of the jaw joint.
Treatment methods for dental periodontitis
| Conservative treatment | Surgery |
Therapeutic:
Physiotherapeutic:
Conservative treatment of periodontitis is accompanied by the use of antibiotics. | Surgical treatment:
|
Important!
The probability of successful conservative treatment of periodontitis is 70 - 90%
Stages of periodontitis treatment
The number of visits to the clinic for the treatment of periodontitis depends on the stage of the disease (acute periodontitis, chronic, chronic in the acute stage) and the chosen technique. Often, therapy is carried out in several stages and requires at least 2 - 3 visits to the attending physician, since it is not recommended to install a permanent filling until the inflammation is completely removed.
- Preparation for treatment: diagnosis using an x-ray, anesthesia injection.
- Drilling a tooth to access canals, removing a nerve, or removing an old filling.
- If necessary, expand channels.
- Antiseptic treatment of canals, application of medications, physiotherapeutic procedures.
- Installation of a temporary filling.
- Removal of the temporary filling, antiseptic treatment of the canals (this stage is repeated until the source of inflammation is completely eliminated; sometimes this may take several months).
- Installation of a permanent filling, control x-ray.
In parallel, the patient is prescribed antibacterial and anti-inflammatory therapy, as well as home rinses with disinfectant solutions.
Symptoms of acute periodontitis
The acute form always occurs with pronounced symptoms. At the initial stage of inflammation, the disease is characterized by pain in the tooth when closing the jaws, a feeling of elongation or expansion of the tooth, darkening of the gums - the tissues acquire a bluish tint and swell, as if there is an increased blood flow.
If the patient has not consulted a doctor for treatment of acute periodontitis, the next stage begins: swelling of the tooth root, enlargement of the lymph nodes behind the ears, slight mobility of the tooth, swelling of the gums and even the cheeks. This occurs due to suppuration in the root area. In acute purulent periodontitis, the patient complains of a throbbing, aching pain that lasts constantly and intensifies at night. The patient suffers from insomnia and fever.
Features of the treatment of periodontitis with fistula
Odontogenic fistula is one of the complications of periodontitis, mainly granulating. It consists of holes in the mucous membrane, which are formed due to the proliferation of granulations and destruction of the tissues surrounding the tooth. In severe cases, a fistula can appear not only in the gum, but also in the cheek, and even on the skin of the face. Purulent contents are released through the hole, which appears due to the inflammatory process in the periodontium.
On the one hand, the formation of a fistula facilitates the course of the disease, since inflammatory products are eliminated through it (which means that the patient most likely will not suffer from severe pain). On the other hand, non-intervention over time can lead to tooth loss.
You can get rid of a fistula only by eliminating its cause - damage to periodontal tissue. Treatment follows a standard scheme: mechanical treatment of the canals, disinfection and thorough filling. Due to the outflow of pus through the fistulous tract, treatment is most often successful and takes less time. After creating suitable conditions, the fistula goes away on its own, but in severe cases, surgical removal of overgrown granulations may be necessary.
How can a fistula on the gum be cured?
Of course, we treat it, we deal with it, we work for it. In order to cure a fistula on the gum, first of all, we should eliminate the reason due to which the fistula occurred. We should not
fight the pimple itself, smear it with various ointments and lotions, but must eliminate the cause of its occurrence.
We must
eliminate the chronic inflammation itself that led to this fistula.
The first treatment option for a fistula is endodontic
For such treatment, we provide the patient with high-quality endodontic treatment under a microscope when:
- the tooth canal itself is visible,
- its branches are visible
- and you can see if there are cracks in the tooth canal.
Our doctors perform minimally invasive treatment procedures under a microscope at a high level. Treatment of processes that led to a fistula, to a fistulous tract on the gum, to complications of various periodontitis. In the video - endodontist of the Scientific Research Center, winner of many international competitions in endodontics and dental restoration Melikov Azer:
In the clinics of the German Implantology Center, special materials are used that seal the apical part very well and for a long period, which are biocompatible with the tissues surrounding the tooth and which give a very good result.
That is, we have a therapeutic method of treatment - this time
. When highly qualified endodontists, using microscopes, special equipment and special materials, carry out canal therapy and eliminate the cause of the fistula.
The second treatment option for fistula is mixed
Second method
- This is a mixed treatment, when treatment is carried out jointly by a therapist and a surgeon. If the lesion is already quite strong, lysis of a certain part of the root apex has occurred, when the process has already been going on for quite a long time, then the therapist cleans the canals:
seals the apical part of the root with a special material, and the surgeon opens, makes surgical access and polishes the apical part of the tooth root.
We do not perform dental resections when the tooth is cut down in half. You often think, I often have patients come to me who have had a resection and you think the person has had ⅔ of the root cut off and this tooth is no longer tenable, it can barely hold on, and why did it have to be done? We do it minimally invasively. We polish the apical part of the root with special ultrasonic tips after the therapist has carried out the treatment, and we get very good long-term results.
The third treatment option is surgery.
There is also a surgical method - this is the third method
treatment when the inflammation is already chronic according to the principle “No tooth - no caries, no periodontitis, no nothing.”
That is, the tooth is removed
, the source of inflammation is removed:
and an implant is placed
:
Subsequent rehabilitation of the patient takes place on the implant.
The fourth treatment option is autotransplantation.
Autotransplantation is a type of third, surgical treatment option. But the patient’s own donor tooth acts as an implant. As a rule, wisdom teeth, which are not involved in the process of chewing food and are actually the body’s reserve for such cases, are excellent for this role. Wisdom teeth transplantation is suitable for posterior teeth and premolars (fourth, fifth, sixth and seventh teeth).
Advantage
This method of treatment is that the patient’s own tooth is transplanted, the patient’s own tissue, which is not foreign to the body, even in conditions of the inflammatory process with a fistula, significantly reduces the risk of tooth-implant rejection.
The specialists of the German Implantology Center have accumulated many years of clinical experience in such operations. You can see how the autotransplantation operation takes place in the following video. There, at the end of the film, the patient shares his impressions of the dental transplant (this is a review 1 year after
the transplant operation):
Treatment of chronic forms of periodontitis
There are three types of chronic periodontitis: fibrous, granulating and granulomatous.
- In fibrous periodontitis, the tissues surrounding the apex of the tooth are replaced by fibrous tissue. The patient usually does not feel pain, and the disease can only be determined by an x-ray.
- Granulating periodontitis is characterized by the growth of granulation tissue: the process of bone resorption (resorption) starts, fistulous tracts are formed, through which inflammatory products are separated. As the granulations expand, the patient begins to experience periodic aching pain.
- Granulomatous periodontitis is accompanied by the appearance of a granuloma - a neoplasm at the root apex. It is a chamber of connective tissue filled with granulations. If the disease is not treated, the growth of granuloma can even lead to a jaw fracture.
Treatment of chronic periodontitis is often carried out using conservative treatment methods. According to modern standards, doctors, as a rule, do not carry out separate treatment for granulomas, cysts and fistula tracts: if the canals are disinfected and properly sealed, the neoplasms will disappear on their own. In advanced cases, surgical intervention is permissible.
Diagnosis of chronic periodontitis
Unfortunately, without the necessary equipment, it is very difficult to identify chronic periodontitis. A visual examination performs a purely formal function, since even in the presence of symptoms (pain, swelling, etc.), it is necessary to determine the type and stage of periodontitis in order to draw up the most effective treatment plan. Today, diagnosis of the disease is carried out in several proven ways.
- X-ray examination. The most popular type of diagnostics. All types of chronic periodontitis can most often be detected on a regular targeted X-ray. In case of fistula formation, a narrow-profile X-ray examination - fistulography - is often prescribed.
- Radiovisiographic examination. A more modern and gentle x-ray examination, during which the image is transferred to a computer screen.
- Electroodontodiagnosis (EDD). Diagnosis of inflammatory processes in the dental pulp by monitoring its response to electric current.
- In the case of periodontitis, specialists use differential diagnosis to distinguish it from other dental diseases with similar symptoms.
Features of the treatment of periodontitis in the acute stage
Exacerbation of periodontitis goes through two phases: intoxication and exudation (appearance of discharge). As the disease progresses, the patient first experiences aching and episodic pain, and then constant throbbing and tearing pain, so treatment cannot be delayed.
Acute periodontitis can be serous or purulent. In the second case, purulent exudate accumulates in the apical part of the tooth root, and the main task for the doctor is to remove it. Sometimes this is enough to clean the tooth cavity and treat the canals, but in severe cases it may be necessary to cut the periosteum for drainage.
Pathogenesis of acute periodontitis
Acute periodontitis - inflammation of the periodontal tissues - occurs for two reasons: infectious infection and mechanical damage.
Sources of infection:
- advanced caries, which has turned into pulpitis - pathogenic bacteria gradually destroy dentin, pulp and reach the periodontium;
- periodontitis - the infection enters the tissue through the gum pockets;
- flu, sore throat - infectious infection occurs through the blood and lymph.
Sources of injury:
- damage received during treatment - root perforation, chips caused by the dentist;
- fractures and bruises of a tooth due to the patient’s negligence.
A separate group includes predisposing factors that can trigger the accelerated development of periodontitis in the presence of a source of infection or injury: allergic reactions, hypothermia, reduced immunity, hypovitaminosis.
Treatment of periodontitis at home
Periodontitis cannot be cured at home, since the disease is caused by bacteria that colonize the dental canals. The only way to get rid of them is to carry out antiseptic treatment and sealing of the canals, and this can only be done by a doctor, but by waiting for a visit to the clinic, you can alleviate the symptoms and reduce pain.
Disinfectants that do not irritate the mucous membranes can be used for rinsing 4 - 5 times a day. Doctors also recommend rinsing with a solution of salt and soda, including after treatment, to relieve swelling and reduce inflammation. Non-steroidal anti-inflammatory drugs are suitable for pain relief. All this will help relieve symptoms, but is not a cure.
You may experience pain after periodontitis treatment. Normally, they last 3–5 days and gradually fade away. If the pain does not subside or returns with renewed vigor, re-therapy is necessary.
Symptoms and manifestations
If pulpitis is diagnosed by acute pain upon contact with cold or hot food, then the characteristic symptoms of periodontitis are painful tapping or pressing on the tooth.
This diagnosis may be indicated by:
- swelling of the cheek or gum near the tooth;
- a feeling of fullness in the tissues of the organ;
- the occurrence of a fistula with the outflow of pus into the oral cavity;
- increased pain when eating or pressing on the causative tooth;
- the feeling of an “overgrown” tooth (due to compaction of the tissues under the root, the organ begins to bulge);
- pulsation in the root area;
- increased temperature in the area of the causative tooth.
The chronic type of this disease can be asymptomatic and detected only with the help of an X-ray examination. Therefore, the insistent recommendations of the dentists of the LeaderStom clinic to undergo a dental examination by a doctor once every six months are so important for the early detection of such diseases.