- Facial neuritis is an inflammatory disease that causes partial, unilateral paralysis or paresis of the face.
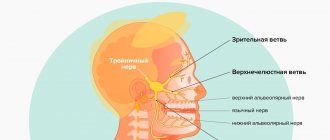
The facial nerve is responsible for contractions of facial muscles and consists primarily of motor fibers. It is one of twelve paired cranial nerves. It begins in the brain and, branching, innervates the face. Its inflammation can occur both at the base (in the core area) and throughout, involving one or more branches. Depending on this, the symptoms of the disease vary.
In most cases, treatment of neuritis of the facial nerve is carried out using conservative methods, and only in the most severe cases (for example, with injuries with a complete rupture of the nerve canal), if therapy is ineffective, surgical treatment is used.
At the Tibet Clinic, treatment of neuritis of the facial nerve is carried out without surgery, using reflexology and physiotherapy. Positive results are achieved in 97 - 98% of cases.
As a result of treatment, contractions of the facial muscles and facial symmetry are restored, spasticity and other symptoms disappear, and the inflammatory process is stopped. These results are long-term and persistent.
Symptoms
A common characteristic sign of the disease is immobilization and distortion of part of the face, in which it turns into a sedentary or completely motionless mask. Additional symptoms depend on where the inflammation occurs.
The facial nerve is a paired nerve; when it leaves the brain, it divides into two symmetrical branches. One of them is responsible for the innervation of the right side, and the other is responsible for the innervation of the left side of the face.
As a rule, inflammation affects only one of the two symmetrical parts, so the symptoms of neuritis are almost always unilateral. Contractions of the facial muscles become difficult or impossible, this manifests itself when trying to frown, smile, close an eye or raise an eyebrow. The face becomes distorted and asymmetrical.
The corner of the mouth and the edge of the eye are lowered, the nasolabial fold is smoothed out. When you try to close your eyelids, the eyeball turns upward (Bell's palsy). When you try to close your eyelids, a gap remains between them, this is called lagophthalmos or “hare's eye.”
Since the facial nerve consists primarily of motor fibers, inflammation of the facial nerve results in muscle symptoms. Sensitive, painful symptoms (in the form of neuralgia) are not typical for such neuritis.
However, the common nerve cord includes the intermedius nerve, which consists of sensory fibers and provides the sensation of taste to the outer two-thirds of the tongue, as well as the functioning of the salivary glands. Therefore, with neuritis of the facial nerve, symptoms such as disturbance, partial loss of taste, and increased salivation (drooling) are possible.
Another possible symptom is tear gland dysfunction, dry eye, or watery eyes. A combination of these two symptoms is possible - the so-called “crocodile tears”, when the eye becomes abundantly moisturized when eating, but remains dry the rest of the time (Bogorad syndrome).
Paresis or paralysis of the face usually develops within 24 hours after the appearance of pain behind the ear - the first sign of neuritis. As the disease progresses, symptoms such as hearing loss or intolerance to loud sounds (hyperacusis) are possible.
Ear pain with neuritis can radiate to the back of the head, temple, and be accompanied by loss of coordination, dizziness, and hearing loss. The complex of these symptoms is called Hunt syndrome.
Disruption of the innervation of the external eye muscle with neuritis of the facial nerve is manifested by convergent strabismus. Along with the characteristic signs of inflammatory damage to the facial nerve, symptoms of concomitant diseases may be observed, for example, shooting pain in the ear with otitis media. Or symptoms of cerebrovascular accident due to atherosclerosis.
From the point of view of Tibetan medicine, inflammation of the facial nerve, like other neuritis and neuropathies, refers to disorders of the governing basis Wind (Rlung - Tib.).
This is a light and cold base that has a great influence on other control systems of the body. Its disorder usually manifests itself not only with local symptoms (neuralgia, numbness, paresis, paralysis), but also with metabolic, immune, cardiovascular, respiratory, digestive, excretory, reproductive systems, as well as hormonal regulation.
Sanzhizhapova Avgustina Dondopovna Reflexologist, neurologist Experience 39 years
Risk factors
Only those who have had chickenpox can get shingles. But there are certain groups that are more susceptible to postherpetic neuralgia:
- Age – the chance of postherpetic neuralgia is higher in the older age group. (30% of people over 60 years of age who have had herpes zoster subsequently develop postherpetic neuralgia) and only 10% of the younger group develop postherpetic neuralgia.
- Localization of rashes - symptoms of neuralgia are more pronounced if the rashes were in the forehead or eyes.
- Concomitant pathology – The presence of a suppressed immune system (after chemotherapy or taking immunosuppressants) or diseases such as AIDS.
Early treatment of herpes zoster is important. Treatment started within 2-3 days after the rash appears can help reduce symptoms and avoid the risk of postherpetic neuralgia.
Causes
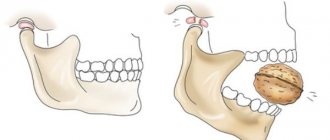
Inflammation of the facial nerve can occur due to its compression by a tumor, aneurysm of a vessel, or swelling of soft tissues with the development of “tunnel syndrome.” In this case, damage to both the root and the trunk of the nerve canal is possible.
The inflammatory process may spread to nerve tissue from the adjacent area. In particular, neuritis can occur against the background of inflammatory disease of the middle ear (otitis).
Often the cause of nerve damage is a viral or other infection, such as herpes or paramyxovirus (mumps).
An ischemic cause of inflammation is also possible, that is, a violation of the blood supply to the nerve due to vascular atherosclerosis or stroke. The provoking factor for the development of the disease is usually severe cooling of the face in a cold wind, rain or draft. This especially often occurs against the background of emotional experiences, stress, psycho-emotional overload or overwork.
Another possible cause of inflammation is trauma received, for example, during deep dental treatment or surgery.
Neuritis of the facial nerve occurs when there is an imbalance of the Rlung base, the main causes of which are poor nutrition, hypothermia (especially exposure to cold wind), stress, overwork, lack of sleep, psycho-emotional overload, negative emotions and mental trauma.
Wind imbalance can occur against the background of fasting, low-calorie diet, strict diet, abuse of dry, rough foods high in plant fiber.For example, a strict diet based on raw vegetables, greens, lettuce, citrus fruits can provoke an imbalance of Wind, which, on the one hand, manifests itself as restlessness, anxiety, irritability, insomnia, and on the other hand, increases the risk of neuritis and neuropathies, in particular the facial nerve.
Kulbuzhev Murat Sultanovich Reflexologist, neurologist Experience 30 years
Causes of inflammatory damage to the trigeminal nerve
Factors contributing to inflammation of the trigeminal nerve are:
- surgical interventions on the jaw bones;
- fractures of the base of the skull, lower and upper jaws;
- tumors;
- complex tooth extraction;
- hypothermia;
- surgery on the maxillary sinus;
- improperly administered anesthesia;
- incorrectly performed dental prosthetics;
- metabolic disorders;
- the presence of foreign bodies that irritate the nerve trunk or injure nerve endings;
- bacterial or viral infection;
- various types of intoxication of the body;
- hypovitaminosis;
- weakening of the immune system.
Classification
Neuritis of the facial nerve can be primary or secondary.
The primary form of inflammation occurs as an independent disease in a healthy person due to hypothermia. This type of neuritis is called catarrhal neuritis.
The secondary form of inflammation develops against the background of infection, otitis media or another disease.
In the vast majority of cases, the disease is acquired, much less often it is congenital.
The congenital nature of the disease may be indicated by Melkersson-Rosenthal syndrome - swelling of the face combined with folding of the tongue.
Types of neuritis
A distinction is made between local neuritis and polyneuritis.
Local neuritis
is an inflammation of any one nerve (facial, auditory, oculomotor, glossopharyngeal, radial, sciatic, peroneal, femoral, etc.).
Polyneuritis
is multiple inflammation of the nerves. If the effect of the factor that caused the inflammation is local, only one nerve is affected. Polyneuritis develops under the influence of a systemic factor, which, as a rule, leads to degeneration of the nerve sheath and nerve fibers.
Diagnostics
Thanks to the characteristic symptoms, establishing a diagnosis for neuritis of the facial nerve does not cause difficulties. Diagnostics is aimed mainly at determining the causes, nature of the inflammatory process, as well as concomitant diseases.
At the initial appointment, the doctor examines and palpates the face, assesses the degree of muscle spasticity and movement disorders. At the same time, he pays attention to the smoothing of natural folds (nasolabial, frontal, etc.), as well as to the non-closure of the eyelids (the inability to close the eye).
For this purpose, several standard tests are performed in which the patient is asked to close his eyes, try to smile, close his eyes, frown, wrinkle his forehead, puff out his cheeks, blow, wrinkle his nose, raise his eyebrows, and bare his teeth. In addition, the taste sensitivity of the tongue is determined.
If additional data is needed, the patient is sent for an MRI or CT scan to identify possible lesions of the brain, blood vessels (in particular, the presence of a tumor, hematoma, aneurysm, etc.), and the presence of inflammatory foci.
To assess the affected area and disturbances in the innervation of facial muscles, electromyography (EMG) is used - a method for studying bioelectrical activity. Using electroneurography, the speed of signal transmission through nerve channels (fibers) is assessed.
In addition, a general urine and blood test and a biochemical blood test are performed.
Important! Eastern medicine views the human body as a single system. Inflammation of the peripheral nerves in this context represents a particular, local manifestation of a general imbalance, almost never the only one.
Therefore, when diagnosing neuritis, a doctor of oriental medicine assesses the degree of imbalance as a whole, identifies concomitant diseases, disorders, functional disorders of the nervous, hormonal, reproductive, immune and other systems.
A treatment plan is designed to address the common causes of all these disorders.
Diagnosis
If pain occurs after an episode of rashes or sensory disturbances, you should consult a doctor. Diagnosis is based on medical history, examination and laboratory tests (necessary to exclude other diseases). Instrumental diagnostic methods (CT, MRI, EMG, ultrasound) are prescribed only if there is a need for differential diagnosis.
Forecast
Exercise therapy, physiotherapy and drug treatment in most cases help reduce symptoms and restore quality of life. Especially if treatment is carried out in a timely manner.
Surgery
Surgical treatment of facial nerve neuritis is usually carried out to restore its integrity, damaged by injury (rupture of nerve fibers). For this purpose, the nerve is sutured.
In addition, surgery may be performed if the cause of nerve inflammation is compression by a tumor, aneurysm, scar tissue, or other neoplasm. The cause of the compression is removed (an example of such an operation is neurolysis - removal of connective tissue proliferation).
Another type of surgical treatment is replacing the damaged portion of the facial nerve with a graft. Such operations are usually performed for injuries. The section of nerve to be transplanted is taken from the leg. The volume of plastic surgery is determined by the surgical plan. In particular, the transplant can be sutured to the facial nerve on the healthy half of the face. In this case, the signal from the brain will arrive to the facial muscles simultaneously on the right and left sides.
Surgical treatment is indicated in cases where conservative therapy does not bring results. It can be carried out within 12 months from the onset of symptoms of neuritis. Carrying out the operation later does not make sense, since by this time the facial muscles have time to atrophy.
Prevention
Certain antiviral medications may help prevent or reduce the effects of shingles, thereby reducing the risk of postherpetic neuralgia:
- Chickenpox vaccine – The varicella zoster virus vaccine (Varivax) is now a routine childhood vaccine, but may also be recommended for older children and adults who have never had chickenpox. This vaccine does not guarantee that a person will not get chickenpox or shingles, but it may reduce the duration and severity of symptoms and the risk of complications such as postherpetic neuralgia.
- Shingles vaccine - (Zostavax) can be given to people over 60 years of age (who have had chickenpox but not shingles). Zostavax is not recommended for use in certain groups of people (for example, those undergoing cancer treatment or those who are immunocompromised).
- Antiviral medications – Antiviral medications such as acyclovir, valocyclovir, famciclovir, when taken within the first 72 hours after the shingles rash appears, can help shorten the duration of shingles and reduce the chance of developing postherpetic neuralgia.
Physiotherapy helps reduce pain and relieve inflammation. Various techniques are used (including transcutaneous electrical stimulation).
Exercise therapy helps restore the elasticity of ligaments and muscles. Exercises can be carried out both on simulators and in the form of gymnastics.
Acupuncture. This method is quite effective in restoring conductivity and reducing pain.
Facial nerve, anatomy
The facial nerve, nervus facialis , the 7th pair of cranial (cranial) nerves is a motor nerve.
The facial nerve innervates the facial muscles of the face (except for the musculus levator palpebre superioris), as well as the muscles of the auricle and skull, the posterior belly of the digastric muscle (musculus digastricus), the stylohyoid muscle (musculus stylohyoideus), the stapedius muscle (musculus stapedius), the subcutaneous muscle of the neck (musculus platysma).
The nucleus of the facial nerve is located on the border of the lower part of the pons with the medulla oblongata, outward and anterior to the nucleus of the abducens nerve. The axons of the cells of this nucleus rise in the dorsomedial direction to the bottom of the rhomboid fossa, then loop around the nucleus of the abducens nerve located here, forming the internal knee of the facial nerve in the area of the facial tubercle . The root of the facial nerve exits the base of the brain in the cerebellopontine angle between the pons and the medulla oblongata, lateral to the olive, then, together with its companions and the cochlear part of the 8th pair of cranial nerves, enters the internal auditory foramen (miatus acusticus internus), then the nerve and its companions enter facial canal (canalis facialis) of the pyramid of the temporal bone (fallopian canal). The canal initially has a horizontal direction (parallel to the apex of the temporal bone pyramid), then bends vertically. It then opens at the base of the skull with a stylomastoid opening (foramen stylomastoideum). The bend of the facial nerve in its canal is called the “external genu of the facial nerve.” In this place there is the knee ganglion (ganglium geniculi), where the cells of the first taste sensitivity neuron for the intermediate nerve are located. After emerging from the stylomastoid foramen, the facial nerve penetrates the parotid gland and divides into many terminal branches to innervate the corresponding muscles, forming the pes anserinus. The companions of the facial nerve in the canal are the parasympathetic lacrimal fibers - the greater petrosal nerve (nervus petrosus major) and the intermediate nerve (nervus intermedius), the 13th pair of cranial nerves, the Wriesberg nerve.
Parasympathetic lacrimal fibers originate from the secretory nucleus, which is located near the nucleus of the facial nerve. Together with the facial nerve, they enter the facial canal, then are the first to leave it as part of the nervus retrosus major, which innervates the lacrimal gland. Loss of function of the greater petrosal nerve is accompanied by the following symptoms - dry eye, eye irritation, lacrimation.
The intermediate nerve is mixed, consists of efferent parasympathetic salivary fibers for the sublingual and submandibular salivary glands, afferent taste fibers for the anterior 2/3 of the tongue. Salivatory fibers originate from the superior salivatory nucleus (nucleus salivatorius superior), leave the brain in the cerebellopontine angle and enter the facial canal next to the facial nerve, then leave the canal in its descending part as part of the chorda tympani (chorda tympani). Sensitive taste fibers begin from the cells of the knee ganglion, the dendrites of which go in the facial canal along with the facial nerve, then depart from it in the descending part of the canal, participate together with salivary fibers in the formation of the tympanic chord, then enter the system of the 3rd branches of the trigeminal nerve (nervus lingualis ) and reach the taste buds of the anterior 2/3 of the tongue. The axons of the cells of the knee bridle leave the pyramid of the temporal bone through the internal auditory foramen, pass through the cerebellopontine angle and end in the taste nucleus of the solitary tract (nucleus tractussoliterii), common with the glossopharyngeal nerve, located in the medulla oblongata. Damage to the intermediate nerve and the chorda tympani, which is its continuation, leads to hypofunction of the sublingual and submandibular salivary glands and impaired taste in the anterior 2/3 of the tongue. Between the two companions in the facial canal, motor fibers are separated from the trunk of the facial nerve, which form the stapedius nerve (nervus stapedius). The stapedius nerve penetrates the tympanic cavity and innervates the stapedius muscle, which provides a certain degree of fixation of the stapes and tension of the tympanic membrane, which creates conditions for the best audibility. Damage to the stapedius nerve is accompanied by a symptom such as hyperacusis. Hyperacusis is an increased unpleasant perception of sounds, especially low tones.
The first to leave the facial canal is the facial nerve's companion, the greater petrosal nerve. The second branch of the facial nerve to leave the facial canal is the stapedius nerve. The third to leave the facial canal is the companion of the facial nerve - the intermediate nerve in the form of the chorda tympani.
There are features of connections between the facial nerve and the cerebral cortex - the lower third of the precentral gyrus. The upper half of the nucleus, which provides innervation to the facial muscles of the upper part of the face, has a bilateral cortical representation due to the partial supranuclear decussation of the corticonuclear fibers. Fibers to the lower half of the nucleus, from which the facial muscles below the palpebral fissure are innervated, originate from the opposite hemisphere. This point is an important criterion in making a topical diagnosis.
Treatment at the Energy of Health clinic
Facial nerve neuropathy requires the fastest and most accurate diagnosis and comprehensive, comprehensive treatment. Only in this case can a rapid restoration of impaired functions be achieved. Neurologists at the Energy of Health clinic use the most effective techniques:
- modern drug regimens that affect the cause of the disease and relieve symptoms;
- physiotherapy courses for tissue restoration;
- massotherapy;
- training in facial gymnastics techniques;
- taping the affected areas;
- observation throughout therapy, adjustment of dosages and medications if necessary;
- a full range of measures for quick and complete rehabilitation;
- organization of sanatorium-resort treatment for the most complete recovery.
Central palsy - facial nerve
Central paralysis of the facial muscles (facial muscles) is observed as a result of damage to the corticonuclear fibers going to the nucleus of the facial nerve. Central paralysis is characterized by dysfunction of the muscles of the lower half of the face, which have unilateral cortical innervation. The main symptom of central paralysis is the smoothness of the nasolabial fold on the side opposite to the lesion. In some patients with central paralysis of the facial muscles, mild deficiency of the orbicularis oculi muscle can be detected. Central paresis of the facial muscles is usually observed in combination with central hemiparesis, or hemiplegia. In contrast to peripheral paralysis, with central paralysis of the facial muscles, the conjunctival reflex, brow reflex, and corneal reflex are preserved, and there is no degeneration reaction.