Acute toothache is a widespread symptom that signals damage to the nerve located inside the tooth or in the tissues adjacent to it. Painful sensations accompanying the development of the pathological process in such situations arise unexpectedly and cause the patient severe physical and psychological discomfort, negatively affecting his performance, diet, rest and sleep. It is impossible to cope with acute toothache and eliminate the causes that caused it at home: in all cases, without exception, victims require professional dental care. However, there are a number of methods that can quickly and effectively relieve pain for the time required to prepare a visit to the doctor.
Introduction
Facial pain (prosopalgia, orofacial pain) is a conventional collective clinical term that unites all pain syndromes localized in the facial area.
According to the International Classification of Diseases, 10th revision (ICD-10), facial pain is divided into those associated with pathology of the anatomical structures of the head and neck, cranial neuralgia and central pain; facial pain is coded G 50.1 - atypical facial pain [1]. According to the terminology of the International Association for the Study of Pain (IASP), orofacial pain is a type of pain that is felt in the face and/or oral cavity [2]. When discussing the problems of facial pain, there is increasing evidence that psychosocial factors have a significant impact not only on treatment outcomes, but also act as prognostic factors for the development of pain syndrome [3]. Many patients with this problem have comorbid conditions, and there are also mental or personality disorders that predispose to chronic pain and thereby affect the outcome of treatment [4]. The results of epidemiological studies indicate that, along with pain syndromes of various localizations, facial pain is one of the causes of disability. It should also be noted that prosopalgia mainly affects women of working age (from 27 to 50 years) [5, 6]. Only 46% of patients with orofacial pain seek medical help, with dentists, neurologists and family doctors prevailing among specialists [5, 7]. In 17% of patients, pain significantly limits their ability to work [8, 9]. Until now, many authors have pointed out the dominant role of trigeminal neuralgia among prosopalgia, while pain in the facial area is represented by a significantly larger number of nosological forms [10]. Thus, in the work of RW Evans (2006) it was shown that in patients with facial pain in 83% of cases there is an overdiagnosis of trigeminal neuralgia, in 100% of cases there is an unsatisfactory diagnosis of idiopathic persistent facial pain as a diagnosis of exclusion [11]. S. Marklund et al. (2010) in a population-based study, using strictly defined pain criteria and examining the neurological status of patients suffering from headaches, showed that trigeminal neuralgia is more common than chronic idiopathic facial pain, but both conditions are rare, and the prevalence of trigeminal neuralgia in lifetime is 0.3% compared to 0.03% for persistent idiopathic facial pain [12].
JS Koopman et al., using research databases of all primary care physicians in the Netherlands, reviewed all cases of trigeminal neuralgia and persistent idiopathic facial pain and found an incidence of 38.7% per 100,000 people [13]. The diagnosis was confirmed by pain diagnostic criteria and found that approximately 48% of patients were misdiagnosed by primary care physicians. Trigeminal neuralgia and cluster headache were the most common types. On the other hand, temporomandibular joint pain (TMJ) and myofascial facial pain syndrome (MFPS) are common in approximately 10–15% of the adult population [14, 15].
According to S. Wirz et al., among patients with chronic facial pain, persistent idiopathic facial pain is represented in 5.8% of cases and is one of the three most common causes of chronic prosopalgia [16]. In the last decade, many authors have reported a wider representation of both MFPS and TMJ dysfunction among patients with facial pain, indicating the dominant role (in 75% of patients) of the muscular-tonic and dysfunctional components in the formation of prosopalgia [6]. There is no doubt that mental health affects pain, with depression and anxiety being particularly significant. It is now known that there are markers of fear and anxiety that increase chronic pain [17, 18].
Patients with borderline personality disorder have been found to have higher levels of pain perception than other patients with the same pain [19].
T. Taiminen et al. reported that of 63 patients with burning mouth syndrome or atypical facial pain, more than 50% had a lifetime history of mental health disorders, including depression. The researchers indicated that these disorders preceded the onset of facial pain. According to the authors, these syndromes may be mediated by dysfunctional dopamine activity in the brain [3]. Recent recommendations for the rehabilitation of patients with temporomandibular disorders also emphasize the need to identify patients with mental health problems (so-called “red/yellow flags”) [20].
Such heterogeneity in the epidemiological features of orofacial pain can be explained by the complexity of the anatomical and functional organization of the face, the difficulty of objectively identifying the causes for most types of facial pain, the absence of a morphological cause of the disease, and concomitant psycho-emotional disorders, such as depression, in the group of patients under consideration.
What to do for acute toothache
Its appearance signals the need to visit the dentist as soon as possible. The doctor will listen to complaints, examine the oral cavity, “knock” the teeth, and prescribe tests to evaluate the internal tissues: CT scan, radiography or ultrasound.
When a potential source of pain is found, it can be further examined using a radiovisiograph. A targeted image gives an idea of the degree of carious lesions, pathologies of bone tissue or the presence of neoplasms.
A more advanced diagnostic method is a 3D image. All pathologies are visible on the three-dimensional model, which allows you to make the correct diagnosis.
Important! If a trip to the dentist is postponed, under no circumstances apply heat to the sore spot. This can increase inflammation and lead to complications.
Nociceptive pain
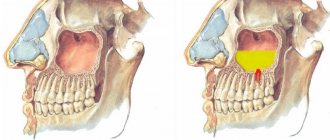
The most common causes of nociceptive facial pain are diseases of the teeth and periodontal tissue [5, 21]. Odontogenic pain is one of the most common and painful. It is capable not only of irradiation, but also of repercussion (reflection into other zones). Few dental diseases are chronic, but given their high prevalence, they should be diagnosed in patients with chronic facial pain [22, 23].
Thus, it is known that when a wisdom tooth is damaged or even difficult to erupt, pain can be felt in the ear and the TMJ area. When the molars of the upper jaw are affected, pain may occur, spreading to the temporal region and upper jaw. Damage to the molars of the lower jaw can cause pain reflected in the area of the larynx and crown, the sublingual area. With pathology of the incisors, pain is usually reflected in the area of the nose and chin [24]. Intraoral pain not associated with dental tissues also occurs (in case of damage to the oral mucosa, tongue, or periodontal tissue). Cases of nerve injury due to either dental procedures or trauma have been reported in the literature. Recently, an international group of experts proposed the use of the term “persistent dentoalveolar pain disorder” to classify persistent pain without local disease (other names such as “atypical odontology” or “phantom toothache” are also found) [25]. Terms such as post-traumatic trigeminal neuropathy, peripheral painful traumatic trigeminal neuropathy may be used in cases where there is a clear correlation between the injury and the development of pain [21].
Why is acute toothache dangerous?
A person who develops dental diseases, suffers pain, or tries to cope with it by taking painkillers can not only lose teeth, but also have problems with the jaw bones.
Pain itself makes a person nervous, exhausted, and his reactions slow down, which often leads to domestic injuries. But much more dangerous is the effect on the body of serious inflammatory diseases in which it occurs (up to sepsis or meningitis).
Neuropathic pain
Episodic neuropathic pain includes paroxysmal neuralgias, of which the most common is trigeminal neuralgia (TN). The main reason for its development is local demyelination of the trigeminal nerve due to mechanical compression (by a vessel) or an autoimmune process, for example, in multiple sclerosis. In the second case, local demyelination and the formation of ephaptic transmission are morphologically detected; It is known that TN may be the only early sign of multiple sclerosis. An epidemiological feature of TN is that its frequency is higher in women and elderly patients. The clinical picture of TN is characterized by short paroxysms of pain of a burning, shooting, lightning-fast nature (duration - several seconds), usually provoked by irritation of trigger points in the face. However, this is often limited to only the branch of the nerve involved in the pain syndrome. Characterized by a refractory period (from 30 s to 5 min) and antagonistic gestures when the trigger zones are irritated immediately after the end of the previous attack. Features of this pain syndrome are contraction of the muscles of the corresponding half of the face and retraction of the corner of the mouth. These muscle contractions are referred to as tonic and clonic convulsions, which appear as a result of the transmission of excitation from the trigeminal nucleus to the facial nerve [10].
Paratrigeminal Roeder syndrome is distinguished separately
, in which the orbital and maxillary branches of the trigeminal nerve are most often affected in combination with fibers of the anterior sympathetic plexus. One of the most serious causes of this syndrome is a tumor in the immediate vicinity of the Gasserian node. In this case, the nature of the pain differs from classical neuralgia: attacks are very sharp, shooting in the orbital area on the affected side, often begin in the morning and last continuously for several hours, sometimes accompanied by nausea or vomiting and Bernard-Horner syndrome [22].
Tolosa-Hunt syndrome (painful ophthalmoplegia).
The disease was described by FJ Tolosa (1954) and, in more detail, by WE Hunt (1961) [26]. Currently, the cause of this syndrome is considered to be an infectious-allergic lesion of the dura mater in the area of the superior orbital fissure involving the orbital, abducens, trochlear, oculomotor nerves, the wall of the internal carotid artery (periarteritis) and the sympathetic fibers lying on it. The picture of the pain syndrome has a bright vegetative coloring; pain of a constant nature in the forehead, orbit, and retrobulbar space is described as “braining,” “gnawing,” “drilling.” Sensory disorders are often detected, such as symptoms of prolapse - hyposthesia in the area of innervation of the first branch of the trigeminal nerve. Occasionally, when the process spreads to the apex of the orbit, there is a decrease in visual acuity with signs of atrophy in the fundus. The duration of the disease ranges from several days to weeks [26].
SUNCT syndrome
(eng. Short-lasting, Unilateral, Neuralgiform headache with Conjunctival injection and Tearing) - short-term unilateral, neuralgic type headache with redness of the conjunctiva of the eye and lacrimation. This rather rare form of primary headache was first described by the Norwegian researcher O. Sjaastad in 1978 [27]. SUNCT syndrome is characterized by paroxysmal, unilateral pain, localized peri- or retroorbitally, lasting about 60 s, accompanied by local autonomic disorders. It is known that this disease most often occurs with remissions and exacerbations: up to 20 pain attacks are observed per day, most of which occur during wakefulness, although night attacks of pain are also possible (1.2%) [27].
Neuralgia of the tympanic nerve
. Described in 1933 by F. Reichert [28]. It is quite rare. It is considered as a type of neuralgia of the glossopharyngeal nerve, which is due to its anatomy. The etiology and pathogenesis are not reliably known. Localization of pain is the external auditory canal, the TMJ on the affected side and the area adjacent to it, sometimes in the depths of the ear. Painful paroxysms in this pathology occur spontaneously, without provoking factors, and are characterized by the absence of trigger zones; Moreover, after an attack, patients note itching and dull pain in the external auditory canal.
Myogenic pain and myofascial pain syndromes
It is known that myofascial disorders in the facial muscles develop according to the same mechanisms as in skeletal muscles and cause 10–20% of pain syndromes on the face [12]. With long-term fixed local hypertonicity in the masticatory, temporal and pterygoid muscles, secondary local disorders arise, such as vascular, metabolic, inflammatory, and they are regarded as trigger points. The most common etiological factors causing myofascial disorders on the face include malocclusion (Costen syndrome), characterized by pain in the TMJ area and specific sound signals in the inner ear (squelching, squeaking, ringing) that occur when opening the mouth and swallowing, as well as reflected pain from the muscles of the neck and upper shoulder girdle and the well-known psychophysiological phenomenon - bruxism [29].
Psychogenic pain.
Psychogenic pain is a diagnosis of exclusion. Facial psychalgia can occur with a depressive disorder, including “masked” depression. The pathogenesis of this type of pain is not completely clear; there is probably a decrease in the activity of antinociceptive systems of the brain [6].
In the treatment of such patients, cognitive behavioral therapy is used, as well as various relaxation techniques [30].
Is it possible to numb a tooth at home?
You can alleviate your condition at home, but only to “stick it out” until you visit the doctor. It is important to eliminate the cause of the problem as quickly as possible, otherwise the pain may become so severe that no home remedies will help. The longer you delay treatment, the more difficult and expensive it will be, so if you start to feel acute toothache, immediately make an appointment at the OneDent clinic.
Nonsteroidal anti-inflammatory drugs relieve symptoms. The best medications for toothache are those based on ibuprofen, ketoprofen, ketorolac, nemesulide, but before taking it, it is better to consult a doctor by telephone and get recommendations on the choice of drug and dosage.
IMPORTANT! If you have a toothache, you should never apply warm compresses or rinse with hot infusions, since heating can only worsen the condition.