The number of allergy sufferers is growing and getting younger around the world.
. One, but very typical example: according to the English publication The Guardian, in the UK alone, the number of cases of hospitalization with anaphylaxis increased by 615% from 1992 to 2012. Moreover, for approximately 27% of hospitalized patients, anaphylactic shock was the first allergic reaction in their lives - before it they believed that they were not sick.
Modern research has revealed a connection between allergies and DNA. A predisposition to an allergic reaction can be inherited from parents, but it can also arise as a consequence of one’s own genetic changes.
Scientists do not yet know why and when hypersensitivity to a certain stimulus “wakes up.” But with the help of allergy tests they can find out to which product (food allergy), chemical substance, plant (hay fever), animal, etc. a violent immune reaction occurs in the body. Such an analysis will help to avoid contact with a potentially dangerous irritant, maintain health and even life.
Allergy tests can also be performed on people who have not had allergic reactions. Tests will help determine what may trigger an unwanted immune response.
Testing is carried out in 2 main ways - using skin allergy tests for a variety of allergens and blood tests. Tests are prescribed by a doctor depending on the purpose of the study, general condition and other factors.
Indications for the study:
- symptoms of food, contact or seasonal allergies are expressed: red spots, itchy rashes, stuffy nose, tears flowing, swelling of the hands, neck, face, oral mucosa, difficulty breathing, etc.;
- hereditary predisposition;
- if treatment of rhinitis, dermatitis, chronic bronchitis, conjunctivitis does not bring results;
- if you cannot tolerate certain foods, medications, or contact with certain animals;
- if you work in hazardous work and cough frequently/constantly, have shortness of breath, rhinitis, or other allergic symptoms;
- if you are undergoing treatment/removal of teeth, surgery with anesthesia.
Go to analyzes
Prescribing allergy tests for children: when and why to do it
Allergen testing is prescribed for children if they have the same symptoms as adults - sneezing, lacrimation, recurrent laryngostenosis, recurring bronchitis, adenoid hypertrophy, etc. If a child gets sick very often, this is also a reason to undergo allergy testing.
But even if an allergy is identified, testing is carried out only when absolutely necessary. If hypersensitivity does not cause any particular concern or complications, the study is carried out no earlier than 5 years of age.
This is explained by the fact that children’s immunity is just developing and there is a high probability that after some time the allergic reaction will change.
But if there is a serious need, skin allergy tests are carried out from 2-3 years of age, when the child can sit quietly for about 15 minutes. There is a special pediatric allergen panel for research:
- epithelium, pet hair;
- milk;
- mites living in house dust;
- egg yolk and white;
- pollen of birch and some herbs;
- other irritants depending on the region, place and lifestyle.
You should be aware that testing often gives false positive results. This is explained by the anatomical features of the child’s skin. The older the person, the more accurate skin tests are.
If the baby requires research (for example, when the parents are allergic), then from 4-6 months a blood test is prescribed, primarily for the level of immunoglobulin E (IgE total). Its increased concentration indicates that the child is prone to allergies. The norm of immunoglobulin E for children and adolescents:
- in children under 2 years of age - 0–64 mIU/ml;
- in children from 2 to 14 years old - 0–150 mIU/ml;
- in adolescents over 14 years of age - 0–123 mIU/ml.
To more accurately determine what the baby is hypersensitive to, a test is performed to determine specific IgE. Blood serum is brought into contact with different types of allergens:
- food;
- household;
- related to rodents, mold, fungi;
- plant pollen;
- others from the pediatric and general panels.
Unlike skin tests, blood tests are less sensitive to non-protein allergens, so sometimes a battery of tests is required.
Preparation for the procedure
• Tests to determine the reaction are carried out while the allergy subsides. • During the week before the test, if possible, eliminate sources that can cause allergies. • Cancel hormonal and antihistamines two weeks before the test. • Following a hypoallergenic diet, if it was prescribed earlier. Testing performed on an empty stomach may be inaccurate. • To take the test, it is important to refrain from eating 8 hours before the test. • If on the eve of the test you become ill with a viral or infectious disease, the test will have to be postponed.
The patient must strictly follow the doctor's recommendations. Violation of the rules entails false negative or positive results of skin tests. If the result is indeterminate, a repeat study will be required; allergens must be reintroduced, which entails discomfort for the patient.
Tests for food allergies
A food or nutritional allergy is a disproportionate and unwanted immune response to substances in vegetables, fruits, fish, etc. An allergy to food (as well as to other irritants) does not depend on the amount of food eaten - sometimes a few grams are enough for anaphylactic reactions to develop shock.
About 3% of adults suffer from the disease in an obvious form, in an erased form (they do not associate food and the symptoms after it with allergies, because the symptoms are minor and pass quickly) - about 6% of adults, children under 6 years old - about 8%. It is not yet possible to cure food allergies, but children “outgrow” it, and in adulthood, for many, the disease either becomes erased or does not manifest itself at all.
An allergic reaction to food occurs within 2 hours after ingestion of the irritant food, most often immediately after ingestion. The reaction manifests itself in:
- rash and itching;
- swelling of the tongue, lips, neck, face;
- difficulty breathing;
- cough;
- runny nose and lacrimation;
- abdominal pain;
- diarrhea of varying intensity;
- vomiting, nausea;
- general weakness, malaise;
- in children, additionally - flatulence, colic, constipation, which are usually combined with an immediate response to the allergen.
The reaction occurs due to an excessive response of the immune system to an irritant in the product. Specific immunoglobulins E are produced. When they interact with proteins, substances are released that can cause negative processes in the gastrointestinal tract, respiratory tract, dermis, etc.
If the allergen enters the body for a long time, immunoglobulins G begin to react and form a delayed, slow reaction. It develops over several hours or even days and usually manifests itself as a rash and itching. The delay makes it difficult to identify the allergen product, and then only tests help make a diagnosis.
Most often, allergies occur to eggs, peanuts, rice, fish, tree nuts, soy products, wheat, and milk protein. In diagnosing an allergen, 2 main methods are used - questioning and laboratory tests:
- general blood test: a reaction to food is often accompanied by an increase in the level of eosinophils—leukocytes;
- determination of the total level of IgE in the blood - in case of allergies it is increased;
- determination of specific immunoglobulins - to determine the specific food component that causes the allergy.
Since a blood test does not allow identifying all allergens, other methods are used:
- keeping a food diary: the patient writes down all meals, scrupulously recording the time, composition, symptoms after consumption (presence, absence, severity, etc.);
- elimination tests (brute force method): a product - a suspected allergen - is removed from the patient’s food and the result is observed;
- provocative tests: when the suspected allergen is removed from the diet, the allergy symptoms have disappeared, the allergen is specially administered to the person, under the supervision of a doctor, and the reaction is observed;
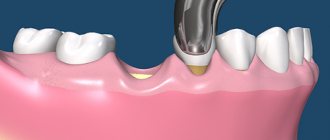
- skin allergy tests: a solution with an allergen is applied to the skin of the forearm, then the skin is lightly scratched (scarification test) or pierced to a depth of 1 mm (prick test), and the reaction is observed.
All these tests are necessary to accurately identify the allergen and eliminate it from food.
Most common allergens
Allergens are foreign substances that, when they enter the body, cause a hypersensitivity reaction (allergies). Most of them contain specific proteins, which cause a super-strong immune response.
In young children, the disease usually occurs in response to substances contained in food (dairy products, fish, eggs, products with synthetic colors and flavors).
In adolescents and adults, other types of allergens come to the fore:
- Household.
- Pollen.
- Animal allergens.
- Fungal.
- Bacterial and viral.
- Household.
Ordinary house dust can cause allergies, and it can be quite difficult to determine the specific substance that caused the reaction. This is due to the large number of components in its composition. These include:
- Fungal spores.
- Particles of human and animal skin.
- Plant fibers.
- Insect excrement.
- Dust mites.
Especially often, dust mites and their waste products lead to the development of allergies. These microscopic insects live in especially large numbers in upholstered furniture, mattresses, carpets and pillows.
Pollen allergens
These include pollen released during the flowering of a wide variety of plants. Most often, the reaction occurs to pollen from weeds, such as ragweed, dandelion, and wormwood. Often, allergies occur to pollen from trees (poplar, birch, oak) and cereal plants (timothy, wheatgrass, rye).
Depending on the flowering period of various plants, several peaks of allergic reactions are observed:
- April May. During this period, trees bloom en masse.
- June July. Associated with the flowering of cereals.
- Aug. Sept. Occurs when weeds bloom.
Fungal allergens
Mold spores are ubiquitous; dozens of varieties of different fungi can be found in the air of any room. Therefore, determining the exact cause of allergies can be very difficult.
It is important to understand that the reaction can be caused not only by fungi, but by food that is produced through fermentation. For example, yeast dough, beer, fermented milk products.
Animal allergens
Typically, the disease occurs upon contact with the epidermis and particles of fur of domestic dogs and cats, and less often with bird feathers, which are used to fill feather beds and pillows. It is possible to develop reactions to urine, saliva, and other waste products of animals.
To find out which animal allergen led to the painful condition, you need to take an allergy test .
Allergy tests for anesthetics, antibiotics
Testing for anesthetics and antibiotics has become very relevant. It is carried out before dental treatment, surgical interventions, and special treatment. The importance of such allergy tests is extreme: more and more people react acutely to medications - lidocaine, ultracaine, benzocaine, mepivacaine, diclofenac and others.
A test for anesthetics and antibiotics must be done for those who have:
- an acute reaction to local anesthetics has occurred before;
- any allergy diagnosed;
- there are symptoms of urticaria, itching, cough, lacrimation without an established cause.
To carry out the test, you need to donate blood from a vein. There is no special preparation for testing: 2 weeks before donating blood you need to stop taking antihistamines.
You cannot donate blood for a test if you have a fever, a chronic disease has worsened or an infection has been detected, during pregnancy and after childbirth, or if you have recently had an abortion.
Important!
Testing with a negative result does not provide a 100% guarantee that an allergy to the medication will not occur during treatment. The mechanism of the occurrence of an acute immune response is still unknown to scientists. But the test reduces your risk to an absolute minimum!
Allergy symptoms
The following manifestations indicate the occurrence of an allergic reaction:
- Prolonged, profuse runny nose.
- Excessive lacrimation, itching in the eye area.
- Sneezing attacks, itchy nose.
- Itchy skin rashes.
- Labored breathing.
If you experience one or more of the above symptoms, be sure to consult an allergist. Only a specialist will be able to prescribe the correct test to determine allergies and effective treatment of the disease.
Immunoglobulin E (IgE) test
IgE are immunoglobulins that are normally found in the blood serum of every person. In adults, the norm is up to 113 mIU/ml. IgE can increase not only with allergies, but also with other diseases, therefore, if the diagnosis is difficult, the doctor may prescribe a comprehensive diagnosis according to indications.
However, even in cases of allergies, the IgE level is not always elevated - in 30% of people with atopic diseases it is within normal limits. In bronchial asthma with an acute reaction to 1 allergen, IgE is normal; only a test for specific IgE and a skin test help diagnose the disease. Angioedema and chronic urticaria do not increase the level of IgE, because in most cases they are of a non-immune nature.
A false negative test result occurs in the presence of antibodies of other classes that are specific to the allergen being tested.
We have given only a few cases where the result of one test may be inaccurate. In reality there are many more. Does this mean that allergy tests are of little effectiveness? No. An experienced allergist will always select a set of tests that will allow you to accurately identify the allergen, and your life will become much safer and more comfortable, because you will know what to avoid.
Prevention and recommendations
At the beginning of the twentieth century, allergies were a rare disease. And today, the European Academy of Allergy and Clinical Immunology (EAACI) predicts that by 2025, 50% of Europeans will suffer from at least 1 type of allergy.
Scientists associate this incredible leap with the sterility of life of modern man and the poor environmental situation in all its manifestations: the state of air, water, food, excessive enthusiasm for household chemicals, medicines, etc.
Allergen immunotherapy (AIT) is increasingly being used to treat allergies. For example, in the treatment of asthma, allergen immunotherapy achieved remission 7 years after the end of treatment. But this area is just developing, so most people still have to live with the disease.
To live comfortably and safely, you need to follow simple rules and manage your allergies:
- avoid allergens or reduce contact with them as much as possible - for this you need to know the allergens exactly;
- Take medications only as prescribed by your doctor. Never self-medicate;
- If you have had anaphylaxis or are at risk of anaphylactic shock, always carry an epinephrine auto-injector with you - the only treatment for a severe allergic reaction;
- keep a diary in which you write down what you eat, what plants, animals, substances you come into contact with, what symptoms arise after contact;
- wear a medical bracelet in case you may have a severe allergic reaction. The bracelet should contain information about your illness and the necessary actions in case you are unable to speak.
Features of skin tests
• Direct allergy tests - are done to diagnose diseases that develop due to hypersensitivity to a certain substance. In this study, allergens and the skin are in close contact: an application, a scarification test, and a prick test are performed. • Indirect skin testing is a testing method designed to detect an allergic irritant. First, the irritant is injected under the skin, then blood is taken from a vein to determine the level of antibodies. Allergens are identified after contact with the skin.
The following groups of allergenic irritants are used: 1) herbal (weeds, meadows); 2) household (presence of dust, chemicals); 3) pollen (seasonal irritant); 4) fungal; 5) animal origin (wool).
• For medications – must be carried out in a laboratory, since the examination uses the patient’s biological material (blood, saliva and others). The results of studies conducted in laboratories are the most informative; they directly depend on the medications taken and the stage of the allergic reaction.
• For urticaria – different types of studies are used: 1) blood test; 2) a smear of the mucous membrane of the nose and throat; 3) analysis of intestinal and stomach microflora; 4) the thyroid gland is examined; 5) identification of the allergen. • Provocative tests - used if information from other methods is insufficient or in case of false (positive or negative) test results. This method helps make a more accurate diagnosis when previous test results and symptoms do not match. A mandatory requirement for the test is that it be carried out in a hospital setting, since there is a high risk of a reaction occurring that requires urgent medical intervention. The allergenic solution is injected into the organ in which the strongest reaction is expected.
Commonly used types of tests: 1) Conjunctival - injected directly into the mucous membrane, a reaction is observed - redness of the eyes, lacrimation. 2) Nasal - injected into the nasal passages, a positive result in the form of difficulty breathing, sneezing, swelling. 3) Inhalation – used using an inhaler, observation is carried out over the bronchi and lungs. Difficulty breathing with whistling, wheezing indicate a positive reaction of the body. 4) Cold - allows you to detect the presence of urticaria by applying ice or cold to the forearm. The appearance of redness and blisters indicates a positive result. 5) Heat urticaria - hot water is applied to the forearm for no more than 10 minutes. 6) Food – the allergen is consumed in food. It is carried out in a hospital setting to provide timely medical care. 7) Exposure - the patient is placed in conditions under which the allergy appeared.