"Levomekol" is an antibacterial combination drug for external use with a wide spectrum of action. Levomekol ointment prevents the spread of pathogenic microbes, eliminates swelling, accelerates wound healing, and also increases local skin immunity.
Levomekol for burns
This combination is provided by two active components in the ointment - Chloramphenicol (aka Levomycetin) and Methyluracil. Chloramphenicol is a natural antibiotic that actively blocks intestinal, pseudomonas and staphylococcal bacilli. And methyluracil accelerates the regeneration of the epidermis. The peculiarity of methyluracil is its ability to easily and quickly penetrate into the dermis, without affecting the membrane cell membrane. This process is associated with the removal of excess fluid from the intercellular space, which usually causes swelling and bruising.
What is Levomekol used for?
Levomekol has a multifaceted therapeutic effect:
- quickly reduces the inflammatory process, prevents its spread to healthy tissues;
- prevents the growth and reproduction of bacterial infectious agents;
- quickly eliminates swelling by normalizing microcirculation;
- ensures delivery of nutrients and biologically active substances, as well as molecular oxygen, to the affected tissues;
- stimulates the regeneration of inflammatory cells of all layers of the epidermis;
- increases immunity at the local level.
The ointment quickly removes all inflammatory processes on the skin
It is worth noting that the presence of purulent discharge and necrotic tissue does not prevent Levomekol ointment from performing its function. The drug can be used to disinfect and accelerate tissue regeneration.
Levomekol, ointment for external use, 40 g, 1 pc.
STADA, Russia
Price from 116₽
There are contraindications. Specialist consultation is required.
Indications for use of Levomekol ointment
Since Levomekol ointment has an antibacterial effect, and at the same time stimulates the restoration of tissue structure, the drug is indicated for the following diseases:
- infection of wounds with pathogenic microflora, ulcers and purulent abscesses on the epidermis;
- burns (mostly 2nd and 3rd degree);
- violation of tissue integrity due to injuries;
- necrotic processes;
- weeping and dry eczema;
- calluses;
- trophic ulcers;
- frostbite of the extremities (superficial layers of the skin);
- pimples, acne, carbuncles, boils;
- otitis and sinusitis (including with purulent discharge);
- treatment of sutures after surgery
- bedsores;
- haemorrhoids.
Levomekol ointment can be used for children
"Levomekol" can be used for children from 1 year. But before this, it is imperative to consult a pediatrician.
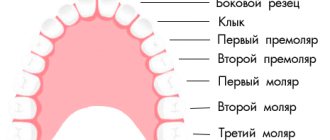
Types of wounds
They can be:
- Operating: applied deliberately for the purpose of performing an operation.
- Accidental: as a rule, these are household damages.
Depending on the nature and conditions of the damage, wounds are distinguished:
- chopped;
- I stab;
- bruised;
- torn;
- crushed;
- chopped;
- bitten;
- mixed;
- firearms.
In children , cut, puncture, bitten, mixed, and also superficial (abrasions, scratches, etc.) predominate. Particular attention is paid to bites that result from an animal or human bite (for example, another child), as they are the most infected. This is due to the large number of harmful bacteria in the oral cavity. They are most often complicated by infection.
According to the degree of infection there are:
- Freshly infected. As a rule, this damage occurs within 3 days from the date of its application. Defects with soil contamination are especially infected.
- Purulent. An infectious process develops in these lesions. Microbes, when multiplying, lead to increased inflammation, necrosis, and also contribute to the appearance of pus. Children with purulent manifestations develop symptoms of general intoxication: nausea, headache, dizziness, weakness, lethargy.
Contraindications
Like many drugs, Levomekol has contraindications:
- individual intolerance to the components of the medication;
- hypersensitivity of the body;
- fungal infections of the epidermis;
- tendency to allergic reactions;
- psoriasis.
The official instructions for use indicate that in pediatrics the ointment is prescribed starting from 3 years of age. However, many pediatricians, based on the harmlessness of Levomekol, allow its use from infancy.
Side effects
Levomekol is considered a universal drug and is usually well tolerated by patients. But in case of overdose (if the drug is used for more than a week), allergic skin reactions may occur.
- hyperemia;
- burning;
- itching;
- urticaria;
- dermatitis at the site of application;
- local swelling;
- When using vaginal tampons, candidiasis may occur.
No incompatibility with other medicinal products has been reported. Make sure that the ointment does not get into your eyes, mucous membranes or inside. In case of contact with eyes and mucous membranes, rinse them immediately with running water. If swallowed, the stomach must be rinsed.
Main manifestations of wounds
Pain
In this case, pain occurs due to damage to the nerve endings that were located at the site of the injury. Over time, swelling may increase, which also leads to increased pain. The severity and degree of manifestation of pain depends on factors such as:
- location of the defect, concomitant damage to large nerve trunks;
- type of weapon or conditions of damage (asphalt, garden, bicycle, sharp object, etc.);
- psychological state of the child.
In essence, pain is an adaptive defense reaction of the body.
Bleeding
Any damage to the skin or mucous membranes is in one way or another accompanied by damage to blood vessels (capillaries, arteries, veins). The nature and degree of bleeding depends on the type of damaged vessel. The larger the vessel and the higher the pressure in it, the more massive the bleeding, and vice versa. It is worth highlighting those places on the body that are accompanied by more heavy bleeding: face, head, neck, hands . In these places, the tissues are better supplied with blood. The condition of the blood coagulation system plays an important role. If a child has a minor abrasion or scratch, which is accompanied by prolonged and heavy bleeding, then it is necessary to consult a pediatrician and pediatric hematologist in order to exclude a disease of the blood coagulation system. This may also be indicated by the appearance of a large number of bruises for no reason.
If a small abrasion is accompanied by prolonged and heavy bleeding, then it is necessary to consult a hematologist.
Hiatus
This phenomenon is associated with a reduction in the elastic fibers of the skin. As a result, the skin edges of the lesion diverge. Many surgeons know what Langer's lines are. They indicate the course and direction of the fibrous structures of the skin. For this purpose, incisions are made along these lines, which leads to rapid healing of the incisions and reduction of gaping. Accordingly, when a defect appears perpendicular to these lines, a wide divergence of the edges of the defect develops.
Levomekol in the treatment of burns
For burns, Levomekol is needed to prevent infection of the wound surface with pathogenic infections, as well as to accelerate tissue healing. Levomekol also copes with inflammation, which can lead to suppuration of the wound. The ointment cleanses the affected area well from both purulent discharge and necrotic cells.
The treatment system for a small area burn of 1-2 degrees is as follows:
- before applying the ointment, the wound is washed under running water;
- the ointment is applied to a sterile gauze pad, which is applied to the wound surface;
- the bandage is applied for a day;
- dressings are done every day - up to 5 times a day.
The burn is treated until the tissue is completely healed. The total duration of the course for minor household burns is 5 – 14 days.
Perineal injuries are one of the most common complications of childbirth, they occur in 40-65% of cases [1, 3]. Infectious complications develop in every 4-5th postpartum woman, leading to suppuration and divergence of the perineal sutures, wound healing by secondary intention. In addition to septic complications, poor healing of the perineal wound can subsequently lead to dyspareunia [5] and secondary genital diseases [4].
The wound healing process is divided into three main phases [2]:
- inflammatory or exudative phase, during which changes occur that determine the entire further course of wound healing;
- proliferative phase, which is the main phase in tissue restoration, aimed at the development of granulation tissue;
- differentiation (reorganization) phase, including maturation and scar formation.
When treating a perineal wound, the nature of its healing is of exceptional importance (N.A. Volkov, 1986). During wound repair, granulation tissue is formed in it based on the proliferation of capillary endothelium and fibroblasts. The main functions of fibroblasts are the synthesis of collagen from amino acids entering the cell. The resulting microvessels ensure the delivery of oxygen to the cells and represent a kind of biological basis from which the migration of collagen-producing fibroblasts occurs. As the wound defect fills, the granulation tissue becomes denser, the number of microvessels decreases, some of them become empty, and the number of cellular elements - macrophages, mast cells and fibroblasts - decreases. Epithelization of the wound begins, the speed of which is 1 mm along the perimeter of the wound in 7-10 days. The most important condition for successful wound healing is a strict pathogenetic focus of treatment, which determines the synchronization of epithelization processes, on the one hand, and the maturation of granulation tissue, on the other (N.A. Volkov, 1986). Traditionally, the leading role in solving this problem belongs to ointments. The therapeutic effect of the ointment is determined by the drugs included in its composition and the effects that the ointment bases have.
One of the drugs that has a positive effect on the healing process is Pantoderm ointment (JSC Akrikhin). Pantoderm contains dexpanthenol (provitamin B5), which forms an active metabolite - pantothenic acid. Pantothenic acid is a component of coenzyme A, which is involved in acetylation processes, stimulates the regeneration and restoration of skin cells and mucous membranes, increases the strength of collagen fibers and has a weak anti-inflammatory effect.
The purpose of the study was to study the effectiveness, safety and tolerability of the use of pantoderm (ointment) in postpartum women with perineal dehiscence in the second and third phases of the wound process.
Material and methods
In the postpartum department of the Research Institute of AG named after. BEFORE. Ott RAMS examined 30 postpartum women with suppuration of the perineal sutures.
When treating purulent wounds of the perineum, we took into account the phases of the wound process. Thus, in the first phase (inflammation phase), treatment tactics were based on well-known surgical principles, requiring separation of the edges of the wound at the site of suppuration, drainage and regular treatment of purulent cavities with antiseptic solutions. The patients received antibacterial, detoxification therapy, physiotherapy and local wound treatment using various drainages and agents with these properties. After cleansing the wound and the onset of the granulation phase, the postpartum women were divided into 2 groups: 20 women (main group) had pantoderm (ointment) added to the treatment regimen, and 10 patients (comparison group) were treated with methyluracil ointment. After daily standard treatment, pantoderm or methyluracil ointment was applied to the wound surface 2 times a day; treatment was carried out in an open manner.
The effectiveness of drug treatment was assessed by dynamic changes and the degree of activation of reparative processes and took into account:
1) subjective factors: complaints of pain, discomfort and burning sensation in the wound area;
2) objective data: the condition of the wound was assessed, namely the nature of granulation, the rate of epithelization and the timing of wound healing;
3) laboratory data: clinical blood test parameters were assessed, the leukocyte intoxication index (LII), data from bacteriological examination of discharge from the wound were examined, histological and immunohistochemical examination of perineal tissue was carried out.
Results and discussion
The age of the subjects ranged from 19 to 37 years. Of these, 25 (83.3%) were primiparous, 5 (16.7%) were multiparous, and 9 (36%) were primiparous aged 27 years and older. All postpartum women had a history of various extragenital and gynecological (mainly inflammatory) diseases. In 82% of women during childbirth, the period of expulsion was shortened using perineo- or epizotomy due to a threatening perineal rupture, high myopia, disruption of fetal activity, operative delivery - the application of a vacuum extractor or exit obstetric forceps; 18% of postpartum women had perineal ruptures of I and II degrees. In the postpartum period, among the 30 examined postpartum women, 19 (63.6%) patients were diagnosed with partial dehiscence of the perineal sutures, 9 (30.0%) had a suppurating infiltrate, and 2 (6.4%) postpartum women had a complete dehiscence of the perineal sutures with subsequent application of delayed secondary sutures. Complications of the postpartum period are presented in table. 1.
The use of Pantoderm in postpartum women of the main group showed that the ointment has pronounced healing properties. When examining the wound in patients of the main group, a more rapid appearance of healthy granulations was noted, which were characterized by a bright pink or red color, were distinguished by a shiny surface and easy bleeding, which indicated the good reparative properties of pantoderm. On the 4-6th day from the start of treatment with pantoderm, the entire wound was treated with granulation, a reduction in the area of the wound and the appearance of marginal epithelization were noted. Final epithelization of the wound took 6-9 days (on average 8±1.2 days). In the comparison group, the clinical picture of the course of the wound process at similar times was comparable, however, the appearance of granulations and epithelization of the wound occurred 1-2 days later than in the main group (Table 2, Fig. 1).
Figure 1. Timing of the appearance of granulation and epithelization in patients of the main group and the comparison group.
The postpartum woman with complete dehiscence of the perineal sutures in the main group had a worse condition of the wound, which served as the basis for an earlier (on the 9th day of the postpartum period) operation of applying secondary sutures to the perineal wound than in the patient from the control group (11th day). In both cases there was a smooth course of the postoperative period.
Thus, the rate of wound healing in phases II and III of the wound process when using Pantoderm was more intense than in postpartum women in the comparison group.
The leukocyte index of intoxication on days 2-3 and 5-8 after birth in patients of the study groups exceeded that during the normal course of the postpartum period by 1.5-2 times. As a result of conservative and surgical treatment, it decreased and corresponded to normal values. The increase in LII was facilitated not only by the presence of an inflammatory process in the tissues of the perineum, but also by the addition of endometritis in 3 subjects (10%), uterine subinvolution in 12 patients (40%), and pathological lactostasis in 1 postpartum woman (3.3%).
During a bacteriological study of discharge from the perineal wound in postpartum women of both groups, gram-negative microflora was isolated in 64.5%, Staphylococcus aureus
- in 23%, anaerobes - in 12.5%. Every third patient had a mixed aerobic-anaerobic flora.
Treatment with Pantoderm was not accompanied by side effects: the ointment was well tolerated by the patients, in no case was there any local irritation or allergic manifestations, and the formation of keloid scars was not observed. The forming scar in patients of this group was more elastic than in postpartum women in the comparison group. This fact, in addition to its aesthetic appearance, characterizes better extensibility of the perineal tissue, which indicates less trauma during subsequent births. Due to the fact that the ointment contains lanolin, it was noted that under the influence of body temperature, lanolin lost its viscosity and the ointment easily filled the wound cavity.
Histological examination of perineal tissue in women from the comparison group (Fig. 2)
Figure 2. Pronounced proliferation of mature fibrous tissue in postpartum women from the comparison group. Staining with picrofuchsin using the Van Gieson method. Uv. 100, 200. In the stromal component, a more intense formation of mature fibrous tissue was noted, and therefore, in the clinical picture of healing of the perineal wound, deformation of the perineal skin with areas of retraction (scar changes) was observed in .1/3 of the patients. No such changes were detected in postpartum women of the main group (Fig. 3).
Figure 3. Mild diffuse subepithelial fibrosis in postpartum women of the main group. Staining with picrofuchsin using the Van Gieson method. Uv. 100, 200.
When quantitatively assessing mast cells in the underlying stromal component in postpartum women of the main group, their significant decrease was noted (Fig. 4),
Figure 4. Quantitative assessment of mast cells in the underlying stromal component in postpartum women of the examined groups. Note.*—differences between groups are significant (p<0.05). which indicated a lower activation of the immediate-type hypersensitivity reaction compared to that in patients of the comparison group.
The degree of cell proliferative activity was assessed by the expression of Ki-67 (an index of proliferative activity) in the basal layer of multilayered squamous epithelium. In the main group (Fig. 5)
Figure 5. Expression of Ki-67 in the layer of stratified squamous epithelium in postpartum women of the main group. Uv. 100, 200. When using Pantoderm, there was a significant difference in the proliferative activity of cells compared with that in the comparison group (Fig. 6),
Figure 6. Expression of Ki-67 in the layer of stratified squamous epithelium in postpartum women from the comparison group. Uv. 100, 200. which indicated a higher degree of wound epithelization in patients of the main group.
To study the degree of tissue vascularization, an immunohistochemical study of CD31 was carried out, followed by an assessment of the relative area in the preparations.
Figure 7. Expression of CD31 in the stromal component in postpartum women of the examined groups. Note. *—differences between groups are significant (p<0.05). The immunohistochemical study performed complemented the histological study of the perineal tissue and gave reason to believe that in the postpartum women of the main group, where Pantoderm was used, the degree of vascularization of the stromal component of the scar area was higher than in the postpartum women of the comparison group.
As a result of the study, it was proven that pantoderm (ointment) has a pronounced stimulating effect on regeneration processes in the wound, promotes the growth of granulation tissue and faster wound healing. When using it, more active epithelization of the perineal wound is observed compared to that in the comparison group (on average by 2 days). The ointment is well tolerated by postpartum women and does not cause side effects or allergic reactions.
Histological and immunohistochemical studies confirm the effectiveness of using Pantoderm for the healing of infected perineal wounds. The examined patients showed an improvement in vascularization, which was reflected in an increase in the metabolic and functional activity of the damaged tissue. This led to a weakening of inflammatory cell infiltration in the underlying stroma, a decrease in fibrosis processes and a decrease in the formation of scar tissue changes. There was a higher mitotic activity of the basal layers of multilayered squamous epithelium, characterizing a high degree of epithelialization of the tissue.
conclusions
1. Pantoderm (ointment) has a pronounced stimulating effect on the regeneration processes in the wound, promotes faster wound healing.
2. When using pantoderm, more active epithelization of the perineal wound is observed, reducing the formation of scar tissue changes.
Levomekol in the treatment of acne
"Levomekol" has an antibacterial and wound-healing effect, therefore it is widely used in dermatology, in particular, in the treatment of acne. The course of treatment depends on the severity of the disease and the number of skin rashes.
Small pimples are treated by applying a thin layer of ointment to the affected area. This is done in the evening for several hours, and before bedtime Levomekol is washed off. Within two weeks, pimples disappear, facial skin becomes even, and small scars heal.
Treating acne with ointment
Levomekol is applied to isolated inflamed pimples in a thin layer, covered with a small piece of cotton wool and left for 2-3 hours. Therapy lasts 2-3 days.
As for opened pimples, the medicine is placed directly into the resulting holes.
To treat acne, Levomekol is applied to the affected area overnight. In the morning, the ointment must be washed off. Typically, the course of treatment takes 2 weeks, during which the inflammation subsides and the acne breaks out or resolves.
To eliminate subcutaneous acne, you need to do the following:
- after washing with soap, the skin is cleansed with any tonic or lotion;
- Apply the ointment in a thin layer on a sterile napkin and apply it to the area of skin with acne;
- the bandage is fixed with adhesive tape.
The duration of the treatment procedure is 3-5 hours. If deep, painful ulcers appear on the skin, keep the bandage on the body all night.
The duration of therapy is about 7-10 days, depending on the degree of damage to the dermis.
Drugs for the treatment of stomatitis
How to treat stomatitis in adults and children?
In the pharmacy you can find a huge number of drugs that help in the fight against stomatitis, the cause of its occurrence and symptoms.
Most of them are sold without a prescription, so anyone can purchase the drug. In the treatment of stomatitis, an integrated approach is used: it is necessary to influence the cause of the disease, as well as alleviate the severity of symptoms.
Painkillers
If the ulcers interfere with eating and talking, or cause great discomfort for the patient, it is considered advisable to prescribe painkillers for topical use. These include:
- Anestezin is available in tablet form for grinding into powder. It has a local analgesic effect on the mucous membrane in the affected area.
- Hexoral is an effective tablet for resorption in the mouth, helping in the fight against ulcerative lesions of the mucous membrane. They have a double result - the drug has an antibacterial and anesthetic effect.
- Lidocaine Asept is available in the form of a spray, which is convenient for topical use. The drug contains lidocaine and chlorhexidine: they provide a disinfecting and analgesic effect. This spray is preferable for ulcerative stomatitis.
- Lidochlor - this gel relieves pain and has an antibacterial effect on the oral mucosa, relieves inflammation.
Herbal remedies - a decoction of chamomile, calendula, sage, also have some antiseptic properties and have a calming effect on the mucous membrane. They help relieve inflammation and relieve swelling of the affected mucosa.
Antiseptics and anti-inflammatory drugs
These drugs are the basis for the treatment of stomatitis. They are produced in the form of tablets for resorption in the oral cavity, in the form of sprays for irrigation of the mucous membranes, ointments, gels, etc.
- Kamistad - contains chamomile, which provides relief from inflammation and a calming effect. Lidocaine has an analgesic effect on the affected mucous membrane.
- Cholisal is available in gel form. Has an excellent anti-inflammatory and antibacterial effect.
- Stomatidine (hexetidine) is an antiseptic drug widely used in dental practice.
- Cametone – contains essential oils, has an antimicrobial and local anesthetic effect. Sold in pharmacy chains in the form of an aerosol or spray.
Ingalipt and Hexoral sprays are also used for topical use for stomatitis. They prevent the spread of infection in the oral cavity and speed up the onset of recovery.
Special products for the treatment of stomatitis in adults
Depending on the cause of the development of stomatitis - a fungus, a virus or a bacterium, specific medications are selected.
Acyclovir, Zovirax are used to combat herpetic stomatitis; in some cases, it is advisable to use interferons. When treating fungal stomatitis, the doctor may prescribe Mycozon, Levorin, nystatin ointment, etc. Bacterial stomatitis requires the prescription of antibiotics, taking into account the sensitivity of microorganisms.
Drugs that enhance regeneration
In this case, drugs that accelerate the healing process of damaged mucous membranes can help.
- Solcoseryl - this medicine is often used in the practice of a dentist. Available in the form of a paste, which must be applied to the lesions. Solcoseryl helps improve trophic processes and accelerates tissue regeneration;
- Sea buckthorn oil is an excellent natural remedy; it helps accelerate the healing of mouth ulcers;
- Vinylin is an antiseptic balm. The principle of action is to envelop the ulcers and heal them more quickly;
- Proposol spray - the effect of the drug is based on propolis.
In the case of an allergic form of pathology, the first step in treatment is the identification and exclusion of the allergen. Some people may experience an allergic reaction after getting braces or dentures, or when using a new drug. Since ulcers in this form of stomatitis are a symptom of the body’s reaction to an allergen, it is the allergy that must be eliminated first. Antihistamines are used for this purpose. You can take them in the form of tablets or applications to the mucous membrane.
There are contraindications. Specialist consultation is required.
Levomekol in the treatment of hemorrhoids
Levomekol ointment can be used as an addition to complex therapy for hemorrhoids during periods of exacerbation. It is recommended to use the ointment in cases where blood is released from the hemorrhoids. Since the drug has an antibacterial effect (wounds can be infected with feces), helps relieve inflammation and neutralize pathogenic bacteria, Levomekol is prescribed for the regeneration of anal tissue.
- it is necessary to wash the perineum and anus with soap and water and dry with a soft towel;
- apply a thin layer of ointment to the anus before going to bed;
- the area of influence from above is covered with a bandage and fixed with an adhesive plaster;
- When treating internal nodes, a tampon is soaked in ointment, which is then inserted into the anus.
Levomekol for hemorrhoids
The duration of therapy is 10 days. Since Levomekol is not a specialized antihemorrhoidal drug, after the inflammation has resolved, the decision to continue therapy and prescribe medications is made only by the attending physician.
Levomekol in the treatment of wounds
Levomekol helps heal damaged tissue and prevents infection of the wound surface. Moreover, it is not so important whether the wound has festered or not. If the wound is not purulent, then first the affected area is treated with an antiseptic. The ointment is applied in a thin layer overnight, then it must be covered with a sterile gauze cloth and secured with a bandage. Most often, wound treatment is required once a day.
If the wound festers, then using cotton-gauze swabs moistened with an antiseptic, the pus and secreted secretions are removed. Then Levomekol ointment is applied to the wound - it should be completely filled, but not too tightly. The affected area is covered with a gauze cloth, also soaked in ointment. As for the frequency of changing the bandage, it all depends on the amount of pus released. Usually a double dressing is sufficient.
And if the wound is deep and accompanied by an infectious lesion, then Levomekol is preheated to 35 degrees Celsius, then a sterile napkin is soaked in ointment (several can be used if the affected area is large) and injected into the lesion. If the affected area is large, use several napkins with Levomekol. It is important that the wound is filled completely, but not too tightly.
Note that to administer the medication into puncture and deep wounds, it is better to use a rubber drainage tube, and inject the heated ointment itself using a syringe.
The duration of therapy usually lasts from 5 to 10 days.
Use of Levomekol ointment in gynecology
Levomekol is successfully used in gynecology and urology.
In gynecology, therapy is carried out using tampons with ointment applied to them. A similar method is indicated for the treatment of the following conditions:
- inflammatory erosion of the cervix;
- inflammation of the uterine appendages (ovaries, fallopian tubes);
- divergence of vaginal sutures after ruptures during childbirth or operations.
The treatment system consists of the following sequence of actions:
- before use, a woman must thoroughly wash and dry the skin of the treatment area and perineum;
- if therapy is used after the divergence of vaginal sutures or after operations, then the sutures must be treated with a weak solution of potassium permanganate or furatsilin;
- you need to make a small cotton swab, put an ointment on top of it measuring 15 mm x 15 mm, and 5 mm high;
- insert into the vagina at night and remove in the morning;
- if therapy is used after the divergence of vaginal sutures or after operations, then the ointment is applied to a gauze bandage and applied to the sutures. Then put on clean underwear (if necessary, you can additionally use a pad). The dressing remains on for 2 to 6 hours.
Using the method described above, the active substance of the ointment is delivered to the affected area and absorbed into the surrounding vaginal tissue.
In urology, Levomekol is used in the treatment of balanitis and balanoposthitis in men, as it has anti-inflammatory and antimicrobial effects. The treatment system consists of the following sequence of actions:
- before applying the ointment, the head of the penis is washed with a weak solution of potassium permanganate or furatsilin, removing pus and dead tissue;
- Levomekol is applied to the affected area in a dense layer.
The remedy is applied 1-2 times a day until complete recovery. After the inflammation is relieved, Levomekol is applied for another week, 1 time per day - in the evening, before bedtime.
Ointments for gums - anti-inflammatory drugs for the treatment of periodontitis
- Article reading time:
1 minute
The shelves of pharmacies are full of packages of therapeutic and preventive oral care products; advertising banners are smiling at people who, apparently, have overcome periodontitis with the help of those very bright boxes. But what is the reality? Patients are especially interested in ointments for teeth and gums in this regard, because the first thing that usually comes to mind when there is pain and redness is: “I need to anoint it with something...”. And then a fatal mistake is made! In the pharmacy you should look not for ointments for healing gums, but for gels, since the fatty base of ointments does not allow the active substances to penetrate the mucous membrane and have the desired effect. Gels are not so quickly swallowed with saliva and have time to act on the inflammatory focus. Any means for treating gums can only help with inflammation of the marginal gums (gingivitis), but if bone structures are affected, these drugs are used only in complex therapy. Applications and rinses alone will only smooth out the picture of inflammation, the disease itself will progress, and the patient will complain that the remedy helped and suddenly stopped working. The best effect will be achieved if you have your teeth professionally cleaned by a dentist before using the gels. The specialist will remove soft and hard dental deposits, which play a significant role in the development of gingivitis and periodontitis.
Popular remedies for treating gums
For a patient with periodontitis, it is important that the drug purchased acts quickly, is used sparingly and, preferably, is inexpensive. The price of ointments and gels for gums can vary within different limits, and a mini-review will help you figure out the rest of the properties.
- Holisal.
A combined action gel that has an analgesic, anti-inflammatory and antiseptic effect. It begins to act within 2 minutes after application and lasts for 3-8 hours. A tube of 10 g costs 300-400 rubles, but the product is very effective and efficient. An analogue is Mundizal gel, its price is less - 260 rubles. Both drugs are consumed quite economically.
- Kamistad.
Popular as a gel for gums during teething, it relieves pain in both the gums and tongue. The main components are lidocaine and chamomile extract. It is significantly inferior to Cholisal in anti-inflammatory properties, but is successfully used in infants, who do not require such a strong effect. A 10-gram tube can be bought for 250 rubles.
- Metrogil Denta.
The tandem of the antibiotic metronidazole and the antiseptic chlorhexidine is in itself quite effective, but still the dosage of metronidazole in the gel is not sufficient to completely relieve inflammation without additional treatment. In addition, the drug does not penetrate into tissues as well as Cholisal, so Metrogyl Denta is used in the initial stages of the disease. 20 g of gel in a bright, recognizable package costs 180 rubles, it lasts a long time.
- Solcoseryl gel.
An analogue of Actovegin, created from purified blood extract of young calves. It has a wound-healing effect, improves the trophism of damaged tissues, and is more often used after surgical interventions in the oral cavity and in case of injury from dental structures. For the treatment of periodontitis, it is still better to prefer narrowly targeted gum products. A 20-gram package can be found for 250 rubles.
- Asepta gel.
A product based on propolis, which has an antiseptic, regenerating and soothing effect. We cannot talk about the very high effectiveness of the drug, because it does not belong to the medicinal category. Rather, it can be used when it is not possible to get an appointment with a dentist and you don’t have any other means with you. The gel costs about 160 rubles.
- Asepta balm.
Although the drug is called a balm, in the oral cavity, thanks to special binding substances, it turns into a viscous gel and can be used for applications. The composition of the product is similar to the Metrogyl Dent formula, but the price of the balm is much less - 170 rubles. for 10 g
How can we sum it up? According to patient reviews, the drug Cholisal performed best; if you have financial difficulties, you can purchase Mundizal. A good solution would be to use special anti-inflammatory pastes such as Parodontax, antiseptic rinses and sprays in complex therapy, which reduce tissue bleeding and accelerate their regeneration.
How to properly use gels and ointments for gums?
All drugs for the treatment of periodontitis using the application method have their own characteristics of use and frequency of application, but the main rule remains unshakable - treatment of the gums should be done with clean hands (you can use a cotton swab). After eating, brush your teeth and squeeze a little gel onto your finger. Gently apply it to the affected area and avoid food or water for at least 30 minutes. There is no need to try to generously lubricate the gums - this will not increase the effect, but it is quite possible to get nausea from swallowing an antibiotic in the gel. The use of any ointments for gums at home does not replace qualified dental treatment, so it is reasonable to consider them as an aid to relieve symptoms and, of course, to prevent gingivitis and periodontitis.
Levomekol or Vishnevsky ointment. What's better?
Let's start with the fact that Vishnevsky ointment and Levomekol, although they are used in similar cases, still have a multidirectional spectrum of action. Thus, Vishnevsky ointment is effective when the wound is in the process of regeneration. Therefore, it cannot be used when the wound is suppurated or severely inflamed. Yes, the drug contains an antiseptic, but its concentration is not enough to provide a bactericidal effect. Moreover, tar and castor oil stimulate blood circulation in the affected area, which worsens the situation.
This is why Vishnevsky’s ointment is not as effective, since Levomekol has higher antibacterial activity due to the presence of an antibiotic in it and accelerates the process of outflow of pus from the wound. Also important are the following distinctive features that determine the superiority of Levomekol ointment:
- no unpleasant odor;
- higher repair characteristics;
- does not provoke irritation in the treatment area;
- when treating boils, Levomekol quickly initiates an abscess and opening of the abscess, followed by wound healing.
But if Vishnevsky ointment helps the patient, then there is little point in changing it.
Products for treating wounds in children
Below we list the most popular and affordable means for treating superficial wounds in children:
- Iodine. Suitable for superficial abrasions, but not for deeper injuries.
- Diamond green.
- Hydrogen peroxide. It is the drug of choice for first aid in the treatment of superficial abrasions in children. Allows you to clean abrasions and scratches well. An equally important property is stopping bleeding.
- Furacilin. To prepare a solution for topical use, dissolve the tablet in water.
- Miramistin. It is also an antiseptic for topical use. Allows you to prevent suppuration. If a purulent process occurs, it allows you to fight it. A pleasant bonus will be the possibility of using this remedy for acute respiratory viral infections, sore throats and pharyngitis in children.
- Chlorhexidine.
An antiseptic helps prevent suppuration.
To speed up healing, ointments and creams can be used such as:
- Levomekol;
- Betadine;
- Vishnevsky ointment;
- cream Bepanten plus.
Analogs
Analogs of Levomekol ointment have a bactericidal and healing effect. But the difference lies in the active ingredient of the drug. So, among the analogues one can name Fugentin, Levosin (additionally has an analgesic effect), Protegentin, Fastin-1, Salicylic-zinc paste.
Synonyms, that is, drugs with the same substance (but in higher concentration) as Levomekol ointment, can be considered Netran and Levomethyl. Substitute medications can only be prescribed by the attending physician.