- Causes of salivary gland cancer and risk groups
- Symptoms of the disease
- Diagnostic methods
- Classification: types of salivary gland cancer
- Stages of the disease
- Treatment
- Complications and relapses
- Life prognosis at different stages of cancer and prevention
The salivary glands produce saliva, a liquid found in the oral cavity that performs some important functions: wetting the mucous membrane, food, facilitating articulation, swallowing, protecting against pathogenic bacteria, etc. There are two groups of salivary glands:
- Large: sublingual, parotid, submandibular.
- Small ones have a microscopic structure, scattered throughout the oral cavity - there are several hundred of them in total.
Cancer can develop in all of these glands. Most often (in 7 out of 10 cases), benign and malignant tumors arise in the parotid salivary glands. Approximately 1–2 tumors out of ten occur in the submandibular salivary glands; in 50% of cases they are malignant. In rare cases, cancer develops in the sublingual or minor salivary glands.
Causes of salivary gland cancer and risk groups
A normal salivary gland cell becomes cancerous when a certain set of mutations occurs in it. The development of malignant tumors is caused by mutations in oncogenes (genes that activate cell reproduction) or tumor suppressor genes (suppress cell reproduction, “repair” damaged DNA, trigger programmed cell death - apoptosis). In each specific case, it is very difficult to judge the reasons for the mutations that occurred in cells. It is impossible to say why exactly they happened.
There are some risk factors that increase the likelihood of developing a malignant tumor:
- The older a person is, the more changes in his genes accumulate, the higher the likelihood of developing various types of cancer.
- Salivary gland cancer is more common in men than in women.
- Irradiation of the head. For example, this may be a previous course of radiation therapy, exposure to ionizing radiation in the workplace.
- There is evidence that the risk of salivary gland cancer is increased in people who have certain occupational hazards: contact with asbestos, nickel alloy dust, work in enterprises that produce rubber and woodworking.
The role of heredity is currently considered insignificant. Most patients do not have a family history (close relatives who have been diagnosed with the same type of cancer). The role of alcohol and tobacco has not been proven. These unhealthy habits are known to increase the risk of head and neck cancer in general, but no association has been found with salivary gland cancers.
Is a mobile phone dangerous? In one study, researchers found that heavy cell phone users were more likely to have parotid tumors (usually benign). But other studies have not found such a relationship.
Arteries and veins
Veins of the submandibular triangle
Arteries of the submandibular triangle
The main vessel in this area is the facial artery. It is the main supply line of the face. In the submandibular triangle, the vessel bends and passes along the upper and posterior surfaces of the gland, located next to the pharyngeal wall.
The facial vein is located in the thickness of the superficial layer of the second fascia. In the region of the posterior border of the triangle, it connects with the retromandibular vein and forms the common facial vein.
Pirogov triangle
This is a small portion of the triangle where the lingual artery can be found. The boundaries of the Pirogov triangle will be:
- hypoglossal nerve;
- digastric tendon;
- mylohyoid muscle.
The hyoglossus muscle acts as the bottom of the triangle. The Pirogov triangle can only be detected when the head is strongly thrown back and tilted in the opposite direction.
Important! The instructions that the doctor must follow when working with this area are extremely important, since the cost of an error is very high. Bleeding from the lingual artery can be fatal.
Symptoms of the disease
Benign and malignant tumors of the salivary glands present with similar symptoms. One of the main differences is that cancer grows much faster and more often leads to a number of symptoms associated with growth into surrounding tissues and compression of nerves.
You need to visit a doctor if you are bothered by the following symptoms:
- A lump or swelling has appeared in the mouth, cheek, jaw, or neck.
- You have noticed that your face has become asymmetrical.
- I am worried about pain in the mouth, neck, ear, cheek, jaw. It doesn't last long.
- Numbness of part of the face.
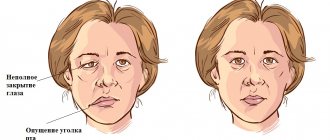
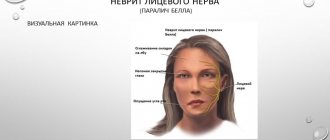
- Weakness in the facial muscles, because of this, half of the face may be “lowered,” which becomes especially noticeable when baring teeth or frowning.
- I can't open my mouth wide.
- Difficulty swallowing.
Operations
To remove the cyst together with P. g. An incision is made in the sublingual area. When isolating a cyst and gland, it is necessary to insert a probe or catheter into the duct of the submandibular gland to avoid injury to it. Isolation of pancreas. should start from the distal pole. In cases where part of the cyst is localized below the mylohyoid muscle, B. D. Kabakov proposed performing the operation in two stages. At the first stage, after dissecting the tissue in the submandibular or submental region, the cyst shell is isolated to its narrowed part at the mylohyoid muscle. This isthmus (the narrow part of the cyst) is ligated and divided. The part of the cyst separated from the surrounding tissue is removed. The wound is sutured in layers, leaving a small opening. At the second stage, the cyst is opened from the bottom of the mouth, widely excising the mucous membrane of the sublingual region covering the cyst, as well as the membrane of the cyst. After this, the cyst wall is sutured with knotted sutures to the edges of the mucous membrane of the sublingual region. The cyst cavity is packed.
See also Salivary glands.
Bibliography:
Kasatkin S.N. Anatomy of the salivary glands, Stalingrad, 1948; Guide to surgical dentistry, ed. A. I. Evdokimova, p. 226, M., 1972, bibliogr.; Sazama L. Diseases of the salivary glands, trans. from Czech., Prague, 1971, bibliogr.; Solntsev A. M. and Kolesov V. S. Surgery of the salivary glands, Kyiv, 1979, bibliogr.; Rauch S. Die Speicheldrusen des Menschen, Stuttgart, 1959.
I. F. Romacheva; V. S. Speransky (an., hist.).
Diagnostic methods
During the initial appointment, the oncologist talks with the patient, questions him, trying to find out risk factors, and conducts an examination. The doctor feels the tumor on the face and cervical lymph nodes, evaluates the sensitivity of the face and the work of facial muscles. After this, the patient can be referred for additional consultation to an ENT doctor.
Computed tomography and magnetic resonance imaging help assess the size, shape and location of the tumor, and detect lesions in the lymph nodes and other organs. The current gold standard for searching for distant metastases is PET scanning. If the tumor is located near the jaw, an x-ray is taken. A chest x-ray helps detect metastases in the lungs and evaluate the condition of the lungs and heart before surgical treatment.
The most accurate method for diagnosing salivary gland cancer is a biopsy. During this procedure, the doctor receives a fragment of pathologically altered tissue and sends it to the laboratory for cytological and histological examination.
The most common procedure is fine-needle aspiration biopsy. Tumor tissue is obtained using a hollow needle similar to the one used for injections. If the required amount of tissue cannot be obtained, the doctor performs an incisional biopsy: makes an incision and removes part of the tumor.
If tumor cells are found in the sample, the diagnosis of cancer is virtually certain.
Layers and fascia of the submandibular triangle
Fascia and muscles
The submandibular triangle consists of 4 layers:
- leather;
- subcutaneous fatty tissue;
- first fascia of the neck;
- second fascia of the neck.
| Layer | Its description |
| Leather | The skin of the submandibular triangle is thin, mobile, and easily stretched. |
| Subcutaneous fat | Subcutaneous fatty tissue has its own characteristics:
|
| First fascia of the neck | The first fascia of the neck is involved in the formation of the subcutaneous muscle of the neck, whose fibers run from bottom to top and from outside to inside. Muscle attachment points:
The nerve that innervates this muscle arises from the facial nerve and is called its cervical branch. |
| Second fascia of the neck |
|
The submandibular triangle contains a large number of important anatomical formations: the submandibular salivary gland, lymph nodes, muscles, blood vessels and nerves.
Classification: types of salivary gland cancer
The salivary glands are made up of different types of cells, any of which can give rise to a malignant tumor. Therefore, there are different types of cancer:
- Mucoepidermoid carcinoma of the salivary gland is the most common type. Most often it is found in the parotid salivary glands, less often in the submandibular and small ones. These tumors are rarely aggressive.
- Adenoid cystic carcinoma is characterized by very slow growth and rare metastasis. However, this malignant tumor can be very difficult to get rid of: it can recur a long time after treatment.
- Adenocarcinoma is a malignant tumor that develops from glandular cells. Different types of adenocarcinomas can occur in the salivary glands: acinic cell carcinoma, low-grade polymorphic adenocarcinoma, basal cell adenocarcinoma, clear cell carcinoma, cystadenocarcinoma, etc.
- Rare types of malignant cancers of the salivary glands include: squamous cell carcinoma, epithelial-myoepithelial carcinoma, anaplastic small cell carcinoma, undifferentiated carcinomas.
Stages of the disease
Salivary gland cancer, like other malignant tumors, is classified into stages according to the generally accepted TNM system. The letter T in the abbreviation denotes the characteristics of the primary tumor: the size and degree of its growth into surrounding tissues, N - spread to the lymph nodes, M - the presence of distant metastases. Depending on these indicators, the following stages are distinguished during salivary gland cancer:
- Stage 0 is “cancer in situ” (carcinoma in situ). The tumor is located within the layer of cells that form the salivary gland and does not grow into neighboring tissues.
- Stage I is a tumor that is located within the salivary gland and measures no more than 2 cm.
- Stage II - the tumor reaches a size of more than 2 cm, but not more than 4 cm.
- Stage III - a tumor that reaches a size of more than 4 cm and/or spreads into surrounding tissues, or a tumor of any size that has grown into surrounding tissues, has spread to one cervical lymph node on the same side, and the focus in the lymph node is no more than 3 cm and does not extend beyond its borders.
- Stage IV includes substages IVA, IVB or IVC. The first two are characterized by varying degrees of spread of the malignant tumor to the anatomical structures of the head, neck, and lymph nodes. If stage IVC is diagnosed, it means that there are distant metastases.
In addition to stages, there are three degrees of malignancy of salivary gland cancer:
- Grade I - low degree of malignancy. Such tumors are called highly differentiated. Tumor tissue is as similar as possible to normal salivary gland tissue. It grows slowly, and the prognosis for such patients is most favorable.
- Grade II are moderately differentiated tumors. Tumor tissue differs more significantly from normal tissue. This cancer is more aggressive and has a poorer prognosis.
- III degree - poorly differentiated tumors. Cancer cells almost completely lose the features of normal ones. Such tumors behave the most aggressively.
Determining the degree of malignancy helps the doctor predict how the cancer will behave and plan treatment correctly.
Treatment
The patient is treated by a team of doctors, which may include: a clinical oncologist, an ENT doctor, an oncologist-surgeon, an oral and maxillofacial surgeon, a chemotherapist, a radiotherapist, etc. The treatment program is determined by the stage of cancer, the histological type of the tumor, its location (which gland is affected) , age, general condition and concomitant diseases of the patient.
Surgery
If the tumor has not grown much into the surrounding tissue, then it is resectable, that is, it can be removed surgically. The surgeon’s task is to excise the tumor while capturing the surrounding tissue so that there are no cancer cells left on the cut line, that is, to ensure a negative resection margin. If tumor cells have spread to the lymph nodes, or a biopsy reveals aggressive cancer, the lymph nodes are also removed.
For parotid salivary gland cancer, surgery presents certain difficulties, because the facial nerve passes through the gland, which controls the work of facial muscles. If the tumor affects only the superficial lobe of the gland, you can remove it separately - perform a superficial parotidectomy. There is no risk of damaging the facial nerve. In some cases, it is necessary to remove the entire gland, and if the tumor has grown into the facial nerve, then it too.
For cancer of the sublingual and submandibular gland, the surgeon removes the gland itself and some of the tissue located around it, including, possibly, bone tissue. In some cases, it is necessary to excise the nerves that control sensitivity, movements in the lower part of the face, in the tongue, and the sense of taste.
For cancer of small glands, the affected gland and part of the surrounding tissue are removed. The extent of the operation depends on the size and location of the tumor.
Radiation therapy
Indications for the use of radiation therapy for malignant tumors of the salivary glands:
- To combat malignant tumors that cannot be removed surgically due to their location or size. Sometimes radiation is supplemented with courses of chemotherapy.
- After surgical treatment. This type of radiation therapy is called adjuvant and is sometimes combined with chemotherapy. Radiation after surgery helps destroy remaining cancer cells and prevent recurrence.
- For advanced cancer. In this case, radiation therapy is aimed at combating pain, difficulty swallowing, bleeding and other symptoms.
Radiation is typically given five days a week for 6–7 weeks. If radiation therapy is used for palliative purposes, the course will be shorter.
Chemotherapy
Chemotherapy is used quite rarely for malignant neoplasms of the salivary glands. Anticancer drugs can reduce the size of the tumor, but are not able to completely destroy it. They are most often prescribed for advanced cancer as palliative treatment or in addition to radiation therapy.
Depending on the type and other characteristics of the cancer, the doctor may prescribe combinations of different chemotherapy drugs: carboplatin, cisplatin, 4-fluorouracil, doxorubicin, paclitaxel, cyclophosphamide, vinorelbine, docetaxel, methotrexate. Chemotherapy for cancer is always given in cycles. The patient is administered the drug, then takes a “break” for several days. The course of treatment may consist of several cycles.
Rehabilitation
After treatment, some problems associated with nerve damage may persist: dysfunction of the facial muscles, speech disorders, swallowing, and cosmetic defects. Some side effects of chemotherapy and radiation therapy go away after treatment is completed, while others persist for a long time. In such cases, rehabilitation courses are indicated. The doctor draws up a rehabilitation treatment program individually, depending on the severity and nature of the disorders.
Histology
The parotid gland has a lobular structure. Connective tissue septa extending from the fascia of the stomach divide its parenchyma into lobules, which in turn form 5-7 larger lobes.
Rice. 5. Schematic representation of the histological structure of the parotid gland. A - at a magnification of 200 times: 1 - intercalary duct; 2 - striated duct; 3 - terminal secretory department; 4—fat cell; 5 - interlobular duct; 6 - interlobular septum; 7 - blood vessel; hematoxylin-eosin staining; B - with a magnification of 600 times: 1 - fat cell; 2 - serocytes of the terminal secretory section; 3 - striated duct; 4 — myoepitheliocytes; 5 - intercalary duct; hematoxylin-eosin staining.
O.J. is a complex alveolar gland (see Glands). Its lobules are formed from terminal secretory sections tightly adjacent to each other - acini and excretory intralobular ducts: intercalated and striated (Fig. 5).
The terminal secretory sections are formed by glandular epithelial cells - serocytes, located on the basement membrane, consisting of a dense network of reticular fibers. The serocyte has a pyramidal shape, its cytoplasm contains a basally located rounded nucleus, a well-developed endoplasmic reticulum with numerous cisterns, a lamellar complex and secretory granules of various types.
In the terminal secretory sections of the lake. secretory tubules are distinguished, which are located between serocytes and have the appearance of thin tubes without their own walls.
Intercellular secretory tubules are characteristic of glands with protein secretion. The apical pole of serocytes, as well as their surface facing the intercellular secretory tubules, are covered with microvilli.
The terminal secretory sections pass further into narrow intercalary ducts lined with cuboidal epithelium, and then into striated ducts, or salivary tubes, lined with single-layer columnar epithelium. The characteristic basal striation of the epithelium of striated ducts depends on the accumulation of mitochondria lying between the folds of the plasmalemma of the basal part of the cell. It is believed that the striated ducts play a role in changing the concentration of primary saliva.
Between the cells and the basement membrane of the terminal secretory sections, intercalary and striated ducts there are myoepithelial cells, or basket cells, which are contractile elements that contribute to the secretion of secretions and maintaining the tone of the gland ducts.
Intralobular ducts pass into interlobular ducts, which run in layers of connective tissue between the lobules of the gland, merge with each other, forming interlobular ducts and, finally, the parotid duct. Interlobular ducts of the lake. lined with double-row prismatic epithelium, which, as the excretory ducts thicken, becomes multilayered. Along the parotid duct the epithelium is multilayered cubic, and at the mouth of the duct it is multilayered squamous.
Complications and relapses
Even if the treatment is successful and the examination results show no signs of the presence of cancer cells in the patient’s body, a relapse may occur in the future. Therefore, you need to regularly see an oncologist, come for examinations, undergo various studies and take tests.
Typically, the doctor prescribes examinations once every few months for several years, then less frequently.
- If cancer recurs, treatment options may vary:
- If the tumor can be removed, surgery is performed followed by a course of radiation therapy.
- If the tumor cannot be removed surgically, the doctor prescribes radiation therapy in combination with chemotherapy.
- If there are distant metastases, chemotherapy becomes the main treatment method. Radiation therapy and surgery can be used to control some symptoms.
With advanced cancer with metastases, achieving remission becomes extremely unlikely. In this case, treatment will be aimed at slowing the progression of cancer, combating symptoms, and prolonging the patient’s life.
Euroonco doctors undertake cancer treatment at any stage. For us there are no hopeless patients. You can always help, and we know how to do it correctly, we have all the necessary technologies, the latest generation drugs.
Pathology
Rice.
2. A patient with chronic sialadenitis of the left submandibular gland: the contours of an enlarged submandibular gland are visible in the submandibular region. The main symptoms indicating a pathological process in the submandibular gland are dysfunction (decrease, increase, delay, as well as a qualitative change in the secretion released from the duct), an increase in the size of the gland (Fig. 2). With a decrease in secretion, patients feel dryness in the oral cavity (see Xerostomia); the delay in secretion is manifested by the so-called salivary colic (tingling, bursting pain in the area of the gland that appears during eating), with increased secretion, salivation occurs (see Salivation).
Damage
Submandibular glands are rarely observed. According to E. E. Babitskaya, during the Great Patriotic War, damage to the pancreas. with the formation of external salivary fistulas (see) was observed in 2% of cases of injuries to all salivary glands. There are cases of damage to the submandibular duct by a disc during the preparation of teeth for crowns. Wound of P. and its duct can lead to the formation of a parenchymal defect, stenosis or complete obliteration of the submandibular duct. A sign of impaired patency of the submandibular duct is swelling of the pancreas, especially during meals. The localization and degree of damage to the gland or its excretory duct is established using sialography (see). To eliminate narrowing of the duct, bougienage with a special probe is used. Obstruction of the duct in the anterior sections is eliminated surgically. In this case, the central end of the duct is prepared, split longitudinally over 1-1.5 cm from the site of fusion and sutured to the mucous membrane of the sublingual region.
Reactive-dystrophic changes
P.J. occur with certain diseases: Mikulicz's disease (see Mikulicz syndrome), Sjögren's syndrome (see Sjögren's syndrome), damage to the endocrine glands, collagen diseases (see), etc.
Acute inflammatory diseases of the pancreas. (see Sialadenitis) occur when they penetrate into the duct of the pancreas. a foreign body, for example, fruit peels, blades of grass, with phlegmon of the submandibular and sublingual areas (due to the spread of the process from surrounding tissues), with an atypical course of mumps (see Epidemic mumps). In these cases, the disease is acute, with a deterioration in general health, an increase in body temperature, discharge of pus from the duct, pain and swelling of the pancreas; purulent melting of the pancreas is not excluded. In the complex to treat. procedures for acute sialadenitis include the introduction of drugs (antibiotics, bacteriophage, proteolytic enzymes) into the ducts of the gland, novocaine blockade of the gland area. In case of viral infection, it is recommended to irrigate the oral mucosa with interferon.
Rice. 3. Sialogram of the left submandibular gland with chronic sialodochitis: the ducts of the gland are unevenly dilated, their contours are clear (indicated by arrows).
Chronic inflammation of the submandibular gland mainly occurs as calculous sialadenitis (see Sialolithiasis). Less common is non-calculous hron, sialadenitis: interstitial (the so-called inflammatory tumor of Küttner or damage to the pancreas in Mikulicz's disease) and parenchymal (in Sjögren's syndrome). Sialodohit P. zh. It is less common than the parotid gland and can be bilateral. Patients complain of periodically appearing swelling in the submandibular region, tingling, bursting pain in the gland area during eating, and the release of salty saliva into the oral cavity. The disease lasts for years with periodic exacerbations, during which severe pain and purulent discharge from the duct are observed. For the diagnosis of chronic sialodochitis of the pancreas. sialography (Fig. 3) or pantomosialography is used. For calculous sialadenitis, treatment is surgical (see Sialolithiasis). For non-calculous sialadenitis and sialodochitis, treatment is aimed at increasing the body's resistance, as well as eliminating concomitant diseases.
Specific inflammatory diseases of the pancreas. (tuberculosis, syphilis and actinomycosis) occur relatively rarely (see Syphilis, Tuberculosis, Actinomycosis).
Relatively rare in P. There are retention cysts that arise as a result of atresia of the salivary ducts. Salivary duct atresia can be congenital or occur as a result of injury or inflammation. Surgical treatment: the cyst is removed along with the pancreas.
Damage to the submandibular gland by the tumor process is observed much less frequently than the parotid gland (see Salivary glands).