Facial nerve, anatomy
The facial nerve, nervus facialis , the 7th pair of cranial (cranial) nerves is a motor nerve.
The facial nerve innervates the facial muscles of the face (except for the musculus levator palpebre superioris), as well as the muscles of the auricle and skull, the posterior belly of the digastric muscle (musculus digastricus), the stylohyoid muscle (musculus stylohyoideus), the stapedius muscle (musculus stapedius), the subcutaneous muscle of the neck (musculus platysma).
The nucleus of the facial nerve is located on the border of the lower part of the pons with the medulla oblongata, outward and anterior to the nucleus of the abducens nerve. The axons of the cells of this nucleus rise in the dorsomedial direction to the bottom of the rhomboid fossa, then loop around the nucleus of the abducens nerve located here, forming the internal knee of the facial nerve in the area of the facial tubercle . The root of the facial nerve exits the base of the brain in the cerebellopontine angle between the pons and the medulla oblongata, lateral to the olive, then, together with its companions and the cochlear part of the 8th pair of cranial nerves, enters the internal auditory foramen (miatus acusticus internus), then the nerve and its companions enter facial canal (canalis facialis) of the pyramid of the temporal bone (fallopian canal). The canal initially has a horizontal direction (parallel to the apex of the temporal bone pyramid), then bends vertically. It then opens at the base of the skull with a stylomastoid opening (foramen stylomastoideum). The bend of the facial nerve in its canal is called the “external genu of the facial nerve.” In this place there is the knee ganglion (ganglium geniculi), where the cells of the first taste sensitivity neuron for the intermediate nerve are located. After emerging from the stylomastoid foramen, the facial nerve penetrates the parotid gland and divides into many terminal branches to innervate the corresponding muscles, forming the pes anserinus. The companions of the facial nerve in the canal are the parasympathetic lacrimal fibers - the greater petrosal nerve (nervus petrosus major) and the intermediate nerve (nervus intermedius), the 13th pair of cranial nerves, the Wriesberg nerve.
Parasympathetic lacrimal fibers originate from the secretory nucleus, which is located near the nucleus of the facial nerve. Together with the facial nerve, they enter the facial canal, then are the first to leave it as part of the nervus retrosus major, which innervates the lacrimal gland. Loss of function of the greater petrosal nerve is accompanied by the following symptoms - dry eye, eye irritation, lacrimation.
The intermediate nerve is mixed, consists of efferent parasympathetic salivary fibers for the sublingual and submandibular salivary glands, afferent taste fibers for the anterior 2/3 of the tongue. Salivatory fibers originate from the superior salivatory nucleus (nucleus salivatorius superior), leave the brain in the cerebellopontine angle and enter the facial canal next to the facial nerve, then leave the canal in its descending part as part of the chorda tympani (chorda tympani). Sensitive taste fibers begin from the cells of the knee ganglion, the dendrites of which go in the facial canal along with the facial nerve, then depart from it in the descending part of the canal, participate together with salivary fibers in the formation of the tympanic chord, then enter the system of the 3rd branches of the trigeminal nerve (nervus lingualis ) and reach the taste buds of the anterior 2/3 of the tongue. The axons of the cells of the knee bridle leave the pyramid of the temporal bone through the internal auditory foramen, pass through the cerebellopontine angle and end in the taste nucleus of the solitary tract (nucleus tractussoliterii), common with the glossopharyngeal nerve, located in the medulla oblongata. Damage to the intermediate nerve and the chorda tympani, which is its continuation, leads to hypofunction of the sublingual and submandibular salivary glands and impaired taste in the anterior 2/3 of the tongue. Between the two companions in the facial canal, motor fibers are separated from the trunk of the facial nerve, which form the stapedius nerve (nervus stapedius). The stapedius nerve penetrates the tympanic cavity and innervates the stapedius muscle, which provides a certain degree of fixation of the stapes and tension of the tympanic membrane, which creates conditions for the best audibility. Damage to the stapedius nerve is accompanied by a symptom such as hyperacusis. Hyperacusis is an increased unpleasant perception of sounds, especially low tones.
The first to leave the facial canal is the facial nerve's companion, the greater petrosal nerve. The second branch of the facial nerve to leave the facial canal is the stapedius nerve. The third to leave the facial canal is the companion of the facial nerve - the intermediate nerve in the form of the chorda tympani.
There are features of connections between the facial nerve and the cerebral cortex - the lower third of the precentral gyrus. The upper half of the nucleus, which provides innervation to the facial muscles of the upper part of the face, has a bilateral cortical representation due to the partial supranuclear decussation of the corticonuclear fibers. Fibers to the lower half of the nucleus, from which the facial muscles below the palpebral fissure are innervated, originate from the opposite hemisphere. This point is an important criterion in making a topical diagnosis.
The main nerves of the face and types of damage when injecting fillers
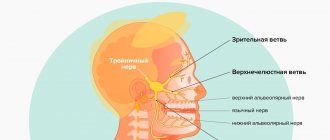
The main nerves that can be damaged during facial injection surgery are the facial and trigeminal nerves. The trigeminal nerve branches into:
- ophthalmic branch;
- maxillary branch;
- mandibular branch.
The trigeminal nerve passes through the openings of the skull and divides into independent sensory components.
Subscribe to our channel on Telegram !
The facial nerve , in contrast, has a single trunk, which passes through the stylomastoid foramen and, at the parotid gland, divides into two branches:
- cervicofacial;
- temporofacial.
The cervical and temporofacial branches are in turn divided into:
- temporal;
- zygomatic;
- buccal;
- marginal branch of the mandible;
- cervical
Nerve damage caused by dermal filler injections can be temporary, reversible, or permanent.
Damage can occur when drugs are administered using either a needle or a cannula. In addition to puncture or partial rupture of the nerve with a needle, it can be damaged as a result of :
- injection of filler directly into the nerve;
- tissue compression after filler injection;
- Too much massage after filler injections.
Nerve damage almost always results in neuropraxia , a loss of sensory and/or motor function.
Facial nerve: symptoms, lesion syndromes
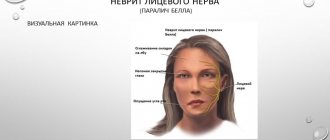
When the trunk of the facial nerve, the root of the facial nerve or the nucleus of the facial nerve is damaged, paresis of the facial muscles (muscle paresis) of the same half of the face develops - prosoplegia. Facial asymmetry occurs, which is pronounced even at rest. The entire affected side is motionless and mask-like. The forehead folds and nasolabial folds are smoothed. The palpebral fissure is widened. The corner of the mouth is downturned. Due to loss of function of the circular muscle of the eye (musculus orbicularis oculi), the eye does not close. This is lagophthalmos , or hare's eye. When you try to close your eyes, the eyeball on the affected side turns upward, the iris goes under the upper eyelid - Bell's symptom. With mild paresis of the orbicularis oculi muscle, the palpebral fissure closes, but less tightly than on the healthy side, the eyelashes remain visible (eyelash symptom). When the normal function of the lacrimal gland is preserved, lagophthalmos is usually accompanied by lacrimation, which is caused by difficulty in moving tears to the lacrimal canal due to insufficient adherence of the lower eyelid to the eyeball and impaired absorption due to displacement of the opening of the canal. Also, lacrimation is facilitated by the strengthening of the tear reflex due to the constantly open eye. Inflammatory phenomena, conjunctivitis, and keratitis often develop due to irritation of the eye membranes by air flow and dust.
The asymmetry of the face increases sharply when teeth are shown. The corner of the mouth is pulled back and it is skewed towards the healthy side - this is the phenomenon of the exclamation point, it is associated with paralysis of the musculus risorius. Due to the weakness of the orbicularis oris muscle, whistling and stretching of the lips into a tube are impossible. The patient often has difficulty speaking and eating. Liquid food on the affected side spills out of the mouth, thick food gets stuck between the cheek and teeth. When frowning and wrinkling the forehead, folds do not form on the side of paralysis, it is impossible to puff out the cheeks, and there is no tension on the musculus platysma of the neck. The brow reflex, nasopalpebral reflex, corneal reflex, and conjunctival reflex are lost or weakened. If damage to the facial nerve occurs in a child of the first year of life, then the sucking reflex, proboscis reflex, and search reflex are reduced. As with any peripheral paralysis, atrophy of the facial muscles is possible. When studying electrical excitability and myography, a degeneration reaction is noted.
Peripheral paralysis of the facial muscles is sometimes accompanied by pain in the face, ear, and mastoid process. The pain is associated with the phenomenon of repercussion. Repercussion is the irradiation of excitation from the motor branches of the facial nerve to the sensory branches of the trigeminal nerve.
Prolonged peripheral paralysis can lead to the development of contracture of the affected muscles, which is manifested by a narrowing of the palpebral fissure on the affected side and a pulling of the mouth when baring teeth towards the affected affected side. Symptoms of incipient contracture are often pathological synkenesis of the facial muscles - ocular synkenesis. They are characterized by the following symptoms. The closing of the eyes is accompanied by movement of the corner of the mouth or baring of the teeth. Baring your teeth causes the eye on the affected side to close.
In pathological processes that cause irritation of the nucleus or fibers of the facial nerve, facial hemispasm is observed - this is squinting the eye and pulling the mouth and tip of the nose to the affected side with simultaneous contraction of the chin muscles and tension of the subcutaneous muscle of the neck. Signs of irritation of the facial nerve are also tics of facial muscles and Chvostek's sign.
Pathology
Primary and secondary lesions of the facial nerve
Defeat of L. n. is caused by various reasons and is usually referred to as “neuritis”. There are primary, or idiopathic, and secondary, or symptomatic, neuritis.
The most common neuritis is L. n., called colds or Bell's disease. In etiology, its main role is played by cooling the body, especially the head. Acute development of the disease over several hours or one day is typical. Its pathogenesis is explained by the fact that cooling, which is an allergic factor, causes vascular disorders in the nerve trunk (spasm, ischemia, edema) that disrupt its nutrition and function (ischemic paralysis). The developmental anomaly is also important - the congenital narrowness of the L. n. canal.
Symptomatic neuritis is observed in various inf., toxic diseases, in inflammatory, tumor processes at the base of the brain, in the cerebellopontine angle, in brain stem encephalitis, poliomyelitis, vascular lesions of the brain stem, in fractures of the base of the skull, the pyramid of the temporal bone, in damage to the parotid gland, in acute and more often chronic otitis, during hypertensive crises, etc.
There are cases of congenital paralysis of the muscles innervated by the L. n. (Mobius syndrome), and also describes hereditary and family cases, apparently associated with a genetically determined anomaly of the L. and. channel.
Topical diagnosis of lesions of L. n. is based on its different structure at different levels, therefore, damage to the nerve proximal to the origin of a certain branch causes loss of the corresponding function, and with distal damage, the function is preserved. This is the basis for diagnosing the level of damage along the L. n. canal, where three branches depart from the nerve: the greater petrosal nerve, which supplies fibers to the lacrimal gland, the stapedius nerve, which innervates the stapedius muscle, and the chorda tympani, which provides taste innervation of the anterior 2/3 tongue . Determining the degree of nerve damage is based on identifying the complete or partial loss of its functions and the dynamics of the development of symptoms.
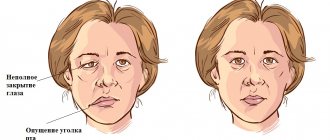
Disturbances in the motor function of the nerve, even with minor damage, can be determined visually by the asymmetry of the face; with complete damage to the nerve, a picture of peripheral paralysis develops: the face is mask-like, the corner of the mouth is lowered, the palpebral fissure is open, the eyebrow is lowered, motionless.
To determine the vegetative function of L. n. examine the functions of tear and salivation. Tear production is examined using the Schirmer test (ribbons of filter or litmus paper are inserted into the lower fornix of the conjunctiva of the eye of the subject, resulting in lacrimation; the intensity of tear production is determined by the length of the paper wetting in millimeters). Salivation is examined by radiometric determination of the concentration ability of the salivary glands and determination of the intensity of salivation by the amount of saliva received (while the subject is sucking a slice of lemon, saliva is collected separately from the pre-catheterized right and left parotid ducts for 1 minute). The study of taste sensitivity on the anterior 2/3 of the tongue is carried out using a chemical method. gustometry, in which the thresholds of the main taste sensations are determined - sweet, salty, sour and bitter by applying the appropriate solutions to the tongue, or electrogustometry, when the threshold values of the strength of the electric current are determined, causing a specific sensation of sour when it irritates the taste buds of the tongue (see Taste).
Rice. 2. A patient with symptoms of neuritis of the left facial nerve: 1 - facial asymmetry; 2 - smoothness of the nasolabial fold and increased asymmetry when teeth are bared; 3 - lagophthalmos, the eyeball is raised upward and retracted outwards (Bell's symptom); 4 - asymmetry of the frontal folds when raising the eyebrows.
The main symptoms of neuritis L. n. (Fig. 2) are caused by peripheral paresis, paralysis of the facial muscles of the upper and lower half of the face (prosopoplegia) on the side of the affected nerve. Already at rest, the mask-like appearance of the corresponding half of the face (the face of the sphinx) attracts attention - the eye is wide open, almost does not blink, the forehead is without wrinkles, the nasolabial fold is smoothed, the eyebrow and corner of the mouth are lowered. The patient cannot frown, raise his eyebrows, when closing his eyes the eyelids do not close completely, the palpebral fissure gapes (lagophthalmos), when trying to close the eye, the eyeball rises upward and deviates outward (Bell's phenomenon), while the sclera is not completely covered. When smiling or laughing, half of the face is motionless; when teeth are shown, the mouth deviates to the healthy side; when the cheeks are puffed out, the diseased side “sails.” While eating, food gets stuck between the cheek and teeth, saliva and liquid food are poorly retained in the mouth, the patient cannot spit or whistle. During the acute period, the patient clearly pronounces labial sounds (b, m). Due to the slight displacement of the mouth, the protruding tongue may deviate slightly in the healthy direction. Often, motor disturbances appear simultaneously with movement disorders, and sometimes they are preceded by usually mild and short-lived pain in the area of the mastoid process and the auricle. Other disorders may also be observed due to damage to the sweat-salivary and taste fibers of the nerve trunk, extending in the L. n. canal. at its different levels. When L. is affected and. in the canal above the origin of the greater petrosal nerve, in addition to paralysis of the facial muscles, there is a lack of lacrimation (dry eye), sweating (dry skin of half the face), unilateral loss of taste in the anterior 2/3 of the tongue, strong, unpleasant perception of ordinary sounds (hyperacusis). With damage below the origin of the petrosal nerve, increased lacrimation is observed, because due to the weakness of the lower eyelid, tears do not enter the lacrimal canal, but flow out; taste disorder and hyperacusis. With a lesion below the stapedial nerve, hyperacusis does not occur; with a lesion below the origin of the chorda tympani, the disorders noted above are absent, but lacrimation persists. When L. is affected. at the level of the geniculate node, Hunt's syndrome is observed - a combination of peripheral paralysis with herpetic rashes and excruciating pain in the area of the auricle, tympanum, back of the palate and the anterior half of the tongue (see Hunt's syndrome). Colds neuritis L. and. sometimes it can be bilateral (diplegia facialis).
An important diagnostic and prognostic value is the study of electrical excitability of the nerve, in which a partial or complete reaction of degeneration is detected, and complete is a prognostically unfavorable sign. An electromyographic study makes it possible to judge the speed of impulse conduction in the left leg. and its branches and the presence of nuclear destruction.
Peripheral muscle paralysis when L. is affected and. should be distinguished from central paralysis associated with damage to the supranuclear tracts, in which the electrical excitability of L. n. not qualitatively changed.
In diagnosis, purely wedge and signs are also important. With L.'s disease. the upper and lower groups of facial muscles are involved to the same extent. With central paralysis, the muscles of the lower half of the face suffer significantly more; paralysis of the muscles of the upper facial group is almost absent. The muscles of the upper parts of the face are innervated from that part of the nucleus of the facial nerve, which receives bilateral supranuclear (corticonuclear) pathways.
In most cases, the course and prognosis of primary neuritis L. and. favorable. Mild cases are observed with complete restoration of facial movements within 2-3 weeks, moderate cases last approx. 2 months, sometimes recovery occurs only after 5-6 months. First, the function of the muscles of the upper half of the face is restored, then the lower half. Complete restoration of facial muscles is observed in approximately 70% of cases. Some patients develop contractures of paretic muscles. On the diseased side, the palpebral fissure narrows, the corner of the mouth is pulled up, and on the healthy side, the nasolabial fold is smoothed out. During the study, it is established that the affected side is the one on which differentiated movements are difficult. Patol and synkinesis are observed. When smiling, laughing, or showing teeth, an even greater narrowing of the palpebral fissure occurs at the same time, the eye may close, and when closing the eyes, the corner of the mouth tightens. Tic twitching of the corners of the mouth, orbicularis oculi muscle, and cheeks appears. Mild synkinesis and isolated tic-like twitches may persist after complete restoration of the function of the facial muscles. Recurrences of catarrhal neuritis L. are possible. both on the same and on the other side. They are rare and in some cases they are more severe, in others they are milder than the initial disease.
Paralysis of the facial muscles is not difficult to establish; it is more difficult to differentiate primary neuritis of L. n. from secondary. Combined lesion of L. n. and other cranial nerves, pyramidal and other conduction disorders indicates the secondary nature of the disease. In all cases of neuritis L. n. An otological examination should be performed. Otitis, especially chronic ones, may be accompanied by damage to L. n. in the channel. Primary neuritis may be indicated by the acute development of the disease, its occurrence in connection with cooling, in some cases after a sore throat or flu. To identify early signs of contractures, a study of the state of electrical excitability of the affected nerve is carried out (see Electrodiagnostics).
Facial nerve damage
There are damages to L. n. for fractures of the base of the skull, wounds of the parotid region, surgical interventions on the ear, salivary gland and total removal of acoustic neuromas. In case of fractures of the base of the skull, the nerve is damaged at the junction of the horizontal section of the LN canal. to vertical. The degree of nerve damage varies. When a nerve ruptures, early paralysis of the facial muscles develops; when the nerve swells or the blood circulation in it is disrupted, late paralysis develops, appearing 10-14 days after the injury.
During ear surgeries, nerve damage can be primary or secondary, when the nerve is compressed by bone fragments or hematoma; open - when the integrity of the L. n. channel is violated. and closed. During operations on the parotid gland or injuries to this area, the extracranial part of the nerve distal to the stylomastoid process is damaged. With total removal of acoustic neuromas of the L. n. is damaged along the path from the brain stem to the internal auditory canal.
Diagnosis of the level of damage to the facial nerve
Isolated lesions of the nucleus of the facial nerve are observed quite rarely. It is manifested by total paresis of the facial muscles and occurs in the pontine form of polio.
More often, pathological foci localized in the pons are more common and lead to the involvement of the nucleus of the facial nerve, radicular fibers, and pyramidal tract in the process, which is manifested by alternating Millard-Hübler syndrome. Simultaneous damage to the nucleus of the abducens nerve is manifested by alternating Foville syndrome.
When the pathological process is localized in the cerebellopontine angle, the symptoms of damage to the facial nerve are combined with damage to its companions (the intermediate nerve and the greater petrosal nerve) and the vestibulocochlear nerve. Paralysis of facial muscles in these cases is accompanied by dry eyes - xerophthalmia, impaired taste in the anterior 2/3 of the tongue on the affected side. Xerostomia may be felt - dry mouth, but more often it does not occur due to the functioning of other salivary glands (parotid, sublingual, submandibular on the healthy side). Hyperacusis does not occur due to concomitant damage to the cochlear nerve. Hearing loss or deafness is more common. There may be signs of dysfunction of the trigeminal nerve and abducens nerve located in the immediate vicinity, as well as cerebellar disorders.
When the facial nerve is damaged in the facial canal above the origin of the greater petrosal nerve, dry eyes, taste disorders and hyperacusis develop simultaneously with paralysis of the facial muscles.
The lesion after the departure of the greater petrosal nerve is accompanied by increased lacrimation, taste disturbance, and hyperacusis.
When the facial nerve is damaged below the origin of the stapedius nerve, but above the origin of the chorda tympani, paralysis, lacrimation, and taste disturbance are observed.
Damage to the nerve in the bony canal below the origin of the chorda tympani or after exiting the stylomastoid foramen causes only paralysis with lacrimation.
When the process is localized in the area of the outer knee of the facial nerve with involvement of the knee node, Hunt's syndrome can be detected - this is paresis of the facial muscles (facial muscles), severe pain and herpetic rashes in the area of the auricle (ear).
Sometimes there are cases of bilateral damage to the facial nerve. Bilateral damage to the facial nerves is called diplegia facialis. The patient's face is mask-like, his eyes are half-open, it is impossible to form his lips into a tube or close his mouth.
Forehead area: nerve anatomy
Knowing where the nerves are located in the highly sensitive area of the forehead is important to ensure not only safety, but also patient comfort during the procedure.
The following are subject to anesthesia:
- supraorbital nerve;
- supratrochlear nerve.
The supraorbital nerve is one of the terminal cutaneous branches of the frontal nerve, which in turn arises from the ophthalmic branch of the trigeminal nerve. N. supraorbitalis provides sensitivity to the forehead and anterior scalp.
The supratrochlear nerve originates from the supraorbital notch, which can be identified by palpation in the area of the supraorbital margin.
Facial nerve: treatment in children
Damage to the facial nerve in children is more common than damage to other cranial nerves, which is due to its anatomical features. The facial nerve is supplied with blood from the external carotid artery system, therefore, when the head is hypothermic, spasm of the external carotid artery leads to nerve ischemia, swelling and compression of the facial nerve. Compression of the facial nerve develops especially easily when the process is localized in the narrow canal of the temporal bone pyramid. The facial nerve canal is connected to the tympanic cavity and the pneumatic cells of the mastoid process. The outflow of lymph from the trunk of the facial nerve occurs in the cervical lymph nodes. In childhood, damage to the cervical lymph nodes is often observed.
Facial nerve: causes of damage, causes of neuritis, neuralgia, neuropathy, paresis, paralysis
The main causes of damage to the facial nerve a are inflammatory diseases (diseases) leading to primary damage to the facial nerve and its involvement in the process secondary to pathological changes in adjacent formations. Meningitis, arachnoiditis of the cerebellopontine angle, inflammatory processes in the area of the eustachian tube (eustacheitis) and mastoid process (mastoiditis), inflammation of the ear (otitis), jaw arthritis, lymphadenitis, mumps can cause the development of neuritis, paresis, paralysis, inflammation of the facial nerve. Also the cause of damage to the facial nerve are primary and secondary polyradiculoneuritis. Traumatic damage to the facial nerve occurs during traumatic brain injury with a fracture of the base of the skull in the area of the temporal bone, during surgical operations on the ear. The cause of paralysis and paresis of the facial nerve in children can be birth trauma, the application of obstetric forceps, or facial presentation. The facial nerve suffers from various tumors of the cerebellopontine ganglion region. Neuroma of the facial nerve, Recklinghausen's neurofibromatosis, tumor of the parotid salivary gland, infiltration due to leukemia are also causes of damage to the facial nerve.
In rare cases, congenital aplasia of the facial nerve nucleus and congenital narrowness of the facial nerve canal occur.
Central palsy - facial nerve
Central paralysis of the facial muscles (facial muscles) is observed as a result of damage to the corticonuclear fibers going to the nucleus of the facial nerve. Central paralysis is characterized by dysfunction of the muscles of the lower half of the face, which have unilateral cortical innervation. The main symptom of central paralysis is the smoothness of the nasolabial fold on the side opposite to the lesion. In some patients with central paralysis of the facial muscles, mild deficiency of the orbicularis oculi muscle can be detected. Central paresis of the facial muscles is usually observed in combination with central hemiparesis, or hemiplegia. In contrast to peripheral paralysis, with central paralysis of the facial muscles, the conjunctival reflex, brow reflex, and corneal reflex are preserved, and there is no degeneration reaction.
Symptoms
Symptoms of facial neuropathy make it possible to immediately suspect the disease. Signs arise from the affected nerve. Patients note:
- acute pain: it usually begins in the ear area and gradually spreads throughout the face and begins to radiate to the occipital region;
- intense lacrimation, less often dry mucous membranes of the eyes;
- discomfort or ringing in the ear due to sharp sounds;
- disturbance of the sense of taste in the anterior parts of the tongue.
As the disease progresses, signs of damage to the motor fibers of the nerve appear:
- smoothness of skin folds, especially nasolabial folds;
- swelling of the cheek when exhaling or trying to pronounce a consonant sound;
- lack of complete closure of the eyelids, rotation of the eyeball upward and outward (lagophthalmos);
- leakage of fluid from the corner of the mouth;
- food getting stuck between the gum and cheek when eating;
- limitation of facial expressions: the patient cannot frown or smile.
If the cause of neuropathy is an infectious process, the characteristic signs are accompanied by symptoms of general intoxication:
- high body temperature;
- headache;
- nausea and vomiting;
- weakness.
Primary neuritis of the facial nerve
Primary facial paralysis is caused by herpes viruses, mumps, enteroviruses, and adenoviruses. Bell's palsy can develop with general or local hypothermia of the face. Bell's palsy is characterized by acute development within 3 to 24 hours. The leading role in the development of Bell's palsy belongs to ischemia, which develops due to vasospasm, or vasodilation with the development of swelling of the facial nerve and compression of the nerve.
Often, neuritis of the facial nerve occurs for no apparent reason against the background of absolute complete health. Sarklinik observed many cases where the first symptoms of facial neuritis appeared after a person slept, at the moment of awakening. This may be due to the activation of chronic infection with weakened immunity, the development of various allergic reactions.
Diagnostics
Neurological disorders characteristic of facial neuropathy can also occur with other diseases, in particular with stroke. That is why, if any similar symptoms occur, you should urgently consult a neurologist.
Diagnosis of pathology includes:
- collection of complaints;
- taking an anamnesis, during which the doctor clarifies the time and circumstances of the onset of symptoms, records previous and chronic diseases, injuries and other important details;
- neurological examination, during which a specialist checks skin sensitivity, motor function, muscle strength, quality of reflexes, functioning of the central nervous system, etc.;
- tests: general blood and urine analysis, biochemical blood test with mandatory determination of glucose levels, determination of antigens and antibodies to infectious diseases if their presence is suspected;
- X-ray of the chest organs: allows you to diagnose tuberculosis, tumors;
- MRI or CT scan of the brain: helps visualize tumors, areas of acute ischemia, hemorrhages, consequences of injuries and strokes;
- CT scan of the temporal bone;
- electroneuromyography: assessment of the speed of impulse transmission along nerve fibers and muscles, allows you to determine the level of damage and severity of the disease;
- consultations with specialists: therapist, otorhinolaryngologist, endocrinologist, infectious disease specialist, if necessary.
The list of studies can be adjusted depending on the specific clinical situation.
Neuritis of the facial nerve secondary
Secondary neuritis of the facial nerve is most often of otogenic origin, observed after or during otitis, mastoiditis, eustacheitis. In these cases, reactive inflammation of the nerve trunk develops. Also, the inflammatory process can penetrate directly into the facial nerve itself due to the penetration of infectious agents into it. This is often observed with purulent epidemic partitis, lymphadenitis of the stylomastoid area. Secondary neuritis of the facial nerve can occur with infectious mononucleosis, toxoplasmosis, typhus, tuberculous meningitis, acute leukemia, cranial polyneuritis, polyradiculoneuritis.
Neuritis of the facial nerve occurs with fractures and cracks of the base of the skull passing through the pyramid of the temporal bone (post-traumatic neuritis of the facial nerve). Hereditary factors and congenital developmental anomalies play a major role in the occurrence of paresis of the facial muscles. There are aplasia of the facial nerve trunk and aplasia of the nucleus of the facial nerve. In this case, there may be unilateral and bilateral violations.
The occurrence of neuritis of the facial nerve is facilitated by a narrowing of the fallopian canal and an increase in the size of the styloid process.
Damage to the facial nerve can be one of the signs of such syndromes as Melkersson-Rosenthal syndrome, Mobius syndrome.
Neuritis of the facial nerve diagnosis
Diagnosis of facial nerve neuritis is based on an analysis of the symptoms preceding and accompanying diseases of the nerve damage. Neurologists, neuropathologists, and reflexologists distinguish such forms of damage as neuritis of the facial nerve and neuropathy of the facial nerve. According to pathogenesis, neuritis is divided into primary and secondary.
Neuritis of the facial nerve must be differentiated from isolated damage to the motor nucleus of the nerve, a variety of common pathological processes in the area of the cerebellopontine angle. Damage to the nucleus of the facial nerve is accompanied by isolated paresis of the facial muscles of the same half of the face without autonomic and sensory disorders, which occurs mainly in the pontine form of poliomyelitis or poliomyelitis-like diseases, tick-borne encephalitis.
When the lower parts of the bridge are damaged, which occurs with tumors, encephalitis, vascular diseases, along with the nucleus of the facial nerve, the pyramidal tract is involved in the pathological process. In such cases, peripheral paresis of the facial muscles is combined with central hemiparesis of the opposite side (Millard-Hübler syndrome). If the nucleus of the abducens nerve is affected, then paresis of the external rectus muscle of the eye (Fauville syndrome) is added to the above symptoms.
Isolated neuritis of the facial nerve is differentiated from processes in the area of the cerebellopontine angle, which develop, for example, with arachnoiditis, tumors of the vestibulocochlear nerve, which is manifested by decreased hearing, deafness, paresis of the facial muscles, sometimes dysfunction of the trigeminal nerve, contralateral spastic hemiparesis.
Polyneuritis and polyradiculoneuritis often involve lesions of the facial nerve. Usually the lesion in these cases is bilateral, often asymmetrical, accompanied by limited or diffuse damage to other parts of the human peripheral nervous system.
Symptoms of trigeminal neuritis
The maxillary trigeminal nerve consists of three types of nerve fibers:
- vegetative;
- motor;
- sensitive.
The symptomatic picture of neuritis may vary depending on which fibers were affected by the inflammatory process.
Damage to sensory fibers
In particular, with inflammation of the sensory fibers, the patient may complain of a tingling sensation, numbness, and weakened sensitivity in the area innervated by the trigeminal nerve.
Damage to motor fibers
When motor fibers are damaged, there is a partial or complete decrease in strength in the innervated muscles, their atrophy and deterioration of tendon reflexes.
Damage to vegetative fibers
When the vegetative fibers are inflamed, the patient experiences cyanosis and swelling of the skin, dryness and thinning of the skin, and the potential risk of developing a trophic ulcer increases.