Causes of necrosis Symptoms Classification Treatment Prevention
Necrosis of the jaw is a severe inflammatory disease in which the bones of the facial skeleton are exposed and die.
Cell death provokes:
- Radiation therapy
. Moreover, necrosis of the jaw bone can develop some time after the end of irradiation, which complicates diagnosis. - Taking synthetic drugs
. Drugs destroy osteoblasts, the basis of bone tissue. - Taking bisphosphonate drugs
. These drugs are prescribed for osteoporosis (in small doses) and cancer that affects the skeletal bones (long-term, in large doses). - Decreased immunity
as a result of diseases (rheumatism, blood diseases, polyarthritis, diabetes) or chemotherapy. - Infectious diseases
- general and oral. - injuries
.
Causes of jaw bone destruction
The disease develops due to a combination of several factors. Under other identical conditions, patients are at risk:
- with poor oral hygiene;
- with periodontitis;
- after dental surgery, including tooth extraction;
- taking large doses of bisphosphonates for a long time;
- during chemotherapy and corticosteroid therapy;
- undergoing treatment with anticancer drugs;
- with diabetes;
- with poorly fitting, chafing dentures.
Infections of any etiology significantly increase the likelihood of getting sick. Untreated, carious teeth open the way for pathogens not only into the oral cavity. In advanced cases, when purulent discharge begins, the infection enters the general bloodstream and spreads throughout the body. On the other hand, sinusitis, otitis, and sore throats are a huge number of pathogens that provoke serious dental diseases. Complications in both cases can lead to osteomyelitis, and this can lead to necrosis of the jaw.
What is dental periodontitis?
Periodontal inflammation is the stage of infection spreading from a carious tooth. It follows pulpitis. The source of infection is located at the apex of the root. This is a small cavity that, in advanced cases, can be filled with pus.
As the disease develops, a cavity appears around the roots. It will open sooner or later. If the disease becomes chronic, it is accompanied by constant suppuration and outflow of pus through a fistula - ducts in which the walls do not fuse.
Symptoms and course
Unfortunately, the disease can occur without any symptoms for a long time. The patient does not experience pain, so he consults a doctor only when the infection has penetrated deep into the bone.
Signs of jaw necrosis:
- pain in an infected tooth or in the socket of an extracted one;
- loosening of teeth;
- swelling so severe that it disrupts the symmetry of the face;
- purulent discharge from the gums;
- putrid odor from the mouth;
- pain when swallowing, chewing, talking.
The main symptom of osteonecrosis of the jaw is bone exposure
.
Prevention
To reduce the risk of developing the disease, you should follow simple recommendations:
- Brush your teeth at least 2 times a day. It is advisable not to use hard brushes to avoid injury to the gums.
- After eating, rinse your mouth with warm, clean water or a special mouthwash.
- Use toothpicks less often.
- Visit your dentist regularly.
- Remove tartar twice a year and undergo professional cleaning.
- Get rid of bad habits. Alcohol and smoking greatly impair dental health.
Periodontitis is one of the most common dental diseases. If you take good care of your teeth and maintain oral hygiene, you can significantly reduce the likelihood of its occurrence.
Back
Classification
The course of the disease caused by infection can be acute, chronic or subacute.
According to location they are distinguished:
- osteonecrosis of the lower jaw;
- necrosis of the upper jaw.
By type of infection:
- endogenous - infection occurs as a result of dental diseases;
- hematogenous - pathogens enter the jaw through the bloodstream.
Also distinguished:
- medicinal (bisphosphonate);
- traumatic.
The American Dental Association defines the following stages of disease development:
Stage 0
– toothache that radiates to the temporomandibular joint or sinus. Mobility of teeth, with intact periodontium. The appearance of fistulas, cysts, fluxes.
Stage 1
– exposure of a section of bone without severe pain
Stage 2
– exposure of a section of bone, accompanied by pain and inflammation
Stage 3
- exposure of a section of bone that extends beyond the alveolar (the one in which the tooth is located) bone. With necrosis of the lower jaw, the jaw is affected down to the lower edge. Bone tissue atrophy occurs. This is the stage of pathological fractures. With necrosis of the upper jaw, the zygomatic arch and maxillary sinus are affected. Numerous fistulas are formed.
Ways to Prevent Bone Dystrophy
To stop the resorption process, it is necessary to let the body know that the tooth root has returned to its place. This can be done in the only way: to perform a dental implantation operation by installing a titanium implant in place of the missing root. The implant, replacing the tooth root, takes over its function and stimulates the jaw bone, stopping bone resorption, which inevitably begins after tooth loss. Implants allow you to restore the functionality of the tooth, providing a natural process of chewing food. The visible part of the tooth is replaced with an abutment, which serves as a support for the crown.
Diagnostics
Symptoms of osteonecrosis of the jaw are similar to other diseases: tumors, bone tuberculosis, actinomycosis. Therefore, the examination is carried out comprehensively:
- History taking
If the patient has had osteomyelitis, is taking high doses of bisphosphonates, has undergone radiation therapy, or has had a jaw injury, the doctor will conduct additional examination. It will confirm or deny the presence of necrosis.
- Dental examination
If the bone is exposed, then the diagnosis is easier to make, but if the disease is at stage zero, additional data is needed.
- Lab tests
Positive tests for c-reactive protein, leukocytosis, high ESR are reasons to suspect a necrotic process. The urine is also checked for the presence of protein and blood cells. In some cases, purulent discharge is analyzed to identify the pathogen before prescribing bacterial therapy.
- X-ray
X-ray, or better yet, CT (computed tomography) helps determine the area of the pathological process, the degree of damage, the presence of fractures, sequesters (dead bone fragments lying freely between healthy tissues).
Types of dental periodontitis
Based on localization, the disease is divided into the following types:
- Regional periodontitis. In this case, tissue damage occurs near the edge of the gums. Often occurs due to injury.
- Apical periodontitis. The tissues are affected near the apical part of the root or at the base. In some cases, it is misdiagnosed as pulpitis.
According to stage, the disease is divided into:
- acute form;
- chronic form.
Acute periodontitis
May be purulent or serous. The first type is especially dangerous, as it can lead to the destruction of periodontal tissue. As a result, the teeth become mobile.
Chronic periodontitis
The chronic form is divided into granulomatous, granulating and fibrous periodontitis. The first two types are the most dangerous, as they are accompanied by pronounced bone resorption.
Treatment
The dentist’s task is to stop the destruction of bone tissue, prevent sepsis, and alleviate symptoms.
For this purpose, therapeutic and surgical methods are used, such as:
- Drug therapy
Broad-spectrum antibiotics, antihistamines, and aseptic mouth rinses are prescribed. For pain, analgesics are prescribed.
- Surgical intervention
The doctor performs curettage of pockets or sockets of extracted teeth. Removes sequestration, opens and provides drainage of purulent foci, splints mobile teeth.
Depending on the stage of the disease, an operation is indicated in which the affected bone is completely removed, leaving only its healthy part.
In many cases, reconstructive surgery must be resorted to to fill the defect or correct the deformity. This could be a bone transplant or jaw restoration.
Treatment of jaw necrosis is a multi-step process that requires the participation of several doctors. Depending on the nature of the disease, the dentist works closely with an oncologist or general practitioner. For reconstructive operations under general anesthesia, the participation of an anesthesiologist and an oral and maxillofacial surgeon is required.
Decision making when endodontic treatment fails
Each clinician continually makes clinical decisions in their practice based on their knowledge, skills and experience. But over the years of practice, more and more clinical cases appear that put us in a somewhat difficult position, since they differ from the standards described in manuals and textbooks. However, making a decision about the fate of a tooth or choosing treatment tactics in some clinical situation still falls on us.
I would like to present to your attention a clinical case with somewhat unusual dynamics.
The patient presented with pain in the area of the 37th tooth. Percussion of this tooth was sharply painful; no changes were observed in the area of the transitional fold. History: The tooth was previously treated endodontically about 10 years ago and was covered with a crown. Radiologically, the condition of the coronary restoration is satisfactory, without visible defects or violations of the marginal seal. In root canals, the obturation material is located 2-3 mm shorter than the radiographic apex in the mesial and distal roots. A fragment of metal density is observed in the distal canal, in the apical part of the root (instrument fragment). Periapical destruction of bone tissue measuring 5 by 5 mm is determined (according to CBCT).
Diagnosis: chronic apical periodontitis of tooth 37 K. 04.5
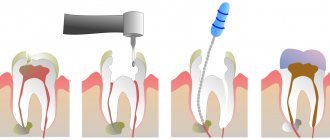
Treatment
The crown and restoration were removed under general anesthesia. Intraroot pins were removed, root canal desobturation was performed, a fragment of the instrument was removed, and apical patency was obtained with a large amount of purulent discharge. The working length was verified using a Morita apex locator, and chemomechanical treatment of the root canals was carried out to size 50 (ISO) in the mesial canals and 70 (ISO) in the distal canals. The canals were treated with a 3% sodium hypochlorite solution and a 17% EDTA solution. An aqueous suspension of calcium hydroxide was injected into the canals for 7 days. Subsequently, calcium hydroxide was replaced several times until the symptoms subsided and the exudation stopped. It took approximately 1.5 months. After this, the root canals were obturated with gutta-percha and ANplus sealer. The tooth is restored with a cast inlay and covered with a temporary crown.
Dynamic observation after 6 months. showed a complete absence of symptoms, but radiologically there was a significant increase in the periapical process in size, both on the targeted image and on CBCT.
Discussion
So, already at this stage of clinical control, we clinicians need to make a decision about the future fate of the tooth. According to the clinical and radiological criteria for “success” or “failure” of endodontic treatment according to Strindberg (1956), an increase in the periapical process can be classified radiographically as a “failure”, despite all the treatment, adequate obturation and restoration. The choice of further tactics for managing such teeth is either extraction, apical microsurgery, or observation for some time. It is quite difficult to perform apical surgery in this area due to the anatomical features. The remaining options are either removal of this tooth or further observation. And in this case, such a factor as the absence of clinical symptoms gives us a chance to make a choice in favor of further observation. Other arguments for such tactics are our knowledge of all aspects of the course of the inflammatory process in this tooth.
Lysis of bone tissue is one of the signs of the body’s immunological reaction to antigens of intracanal microflora. And most often it proceeds according to certain rules. The leading role in the lysis of periapical bone tissue is played by the activated macrophage, which, together with the T lymphocyte, secretes interleukins, which, in turn, activate osteoclasts that absorb bone tissue. Accordingly, the greater the number of activated macrophages, the greater the lysis of bone tissue. According to studies by Akamine A, Hashiguchi I, et al (1994), a numerical increase in macrophages occurs in the first 10 days of inflammation and within 60 days their number remains constant. After day 90, only the number of macrophages decreases so much that osteoclast activation no longer occurs and bone tissue building begins to work. But this is in a normal, routine clinical situation. In this clinical case, it is worth considering that the acute stage of the process lasted not ten days, but about a month, with continued exudation. Therefore, the number of activated macrophages most likely increased all this time and the process of bone tissue lysis began, which continued even after the symptoms subsided and the root canals were obstructed. According to Zvi Metzger, "...the prolonged healing of many periapical lesions suggests the possibility that activated macrophages in the lesion may maintain their activation state after the initial cause of their activation has been eliminated, namely, the activation state may outlive its beneficial purpose and become a burden. Macrophages are known to persist in tissues for many months and if their state of activation is maintained, they can inhibit fibroblasts, support osteoclastic activity and inhibit osteogenesis, thus preventing bone and connective tissue repair." (“Periapical Lesions of Endodontic Origin” - ZVI METZGER, ITZHAK ABRAMOVITZ).
Our great desire to see the beginning of the healing of the periapical process as early as possible after root canal treatment is understandable, as is the case with every specialist who expects positive effects from his work. However, the body lives according to its own laws and does not obey our desires.
Further clinical and radiological studies of this clinical case showed the correctness of my reasoning and the choice of tactics for further monitoring of the tooth in a rather difficult period of decision-making.
Main features
- Pain
In each case it can manifest itself differently. Sometimes it is pain when biting, sometimes it is continuous. It may get worse at night and subside with meals. It can radiate to the temple, ear, even nose. Being whiny or harsh.
- Redness
It may or may not be visible. This is a symptom that is more often detected by a doctor.
- Edema
Any inflammation is accompanied by swelling, but we cannot always determine this.
- Temperature increase
This doesn’t always happen, but fever is a sign of inflammation, so in this case you definitely shouldn’t put off going to the dentist.
- Tumor
This is also a dangerous signal; you need to see a doctor urgently.
If a tooth is inflamed and hurts, temporary measures will not help; you need a full diagnosis and treatment in a clinic. The alternative is tooth loss due to an advanced process.
What is osteitis of the jaw?
Osteitis of the jaw is an inflammatory process that occurs in the jaw bone tissue and spreads beyond the periodontium of one of the teeth to the spongy substance of the bones. This is a dental disease that develops along the neurovascular bundle, as well as through contact. It is often accompanied by periostitis (inflammation of the periosteum), less often osteomyelitis (inflammation of the bone marrow with the formation of fistulas, abscesses, and phlegmon).
Osteitis can be acute or chronic. Acute is characterized by destruction of dental bone tissue, and chronic develops in the presence of a chronic focus of infection in the periodontium of the tooth, followed by proliferation, when cells cannot perform a protective function, and the infection spreads deeply.
Main symptoms of jaw inflammation
There are symptoms of osteitis that occur at the beginning of inflammation in bone tissue. This:
- sudden pain that occurs in the affected area of the jaw;
- swelling (hyperemia) of the sore spot;
- difficulty chewing food;
- spread of pain throughout the entire oral cavity.
If the source of infection is a sore tooth, then difficulty occurs when opening the mouth. If the disease develops rapidly, an increase in body temperature is possible.
With further development of osteitis, the inflammatory process is accompanied by suppuration in the affected area. The general condition of the patient depends on the associated secondary damage surrounding the bone tissue (periostitis, abscess, phlegmon).