Leukoplakia of the oral cavity: causes of the disease
The reasons causing the development of the disease include:
- Smoking. When using tobacco, the oral cavity is exposed to various irritants, including thermal (incoming smoke has a temperature of about 60 degrees Celsius) and chemical (nicotine, tar and combustion products). No less dangerous is chewing tobacco, which is also a provoking factor.
- Eating either very hot or very cold food on a regular basis for a long time.
- Mechanical trauma (bad bite, sharp edges of teeth, orthopedic structures installed with violations).
- Metal seals that cause galvanic currents.
- Inhalation of vapors of gasoline, benzene, varnishes and paints, as well as other resins.
- Hormonal imbalance, constant stress and lack of retinol.
Symptoms
The first signs of the disease often go unnoticed because they do not cause any pain or discomfort in the patient. Nevertheless, a specialist will be able to determine the onset of leukoplakia by the appearance of the mucous membrane, lips and the area where the teeth meet.
The first sign of the disease is the appearance of a keratinized gray area, which can appear on the palate (in smokers), in the corners of the mouth, on the inside of the cheek, etc. An easily removable white plaque forms in this area, but after a few days the formation makes itself felt again . The patient may feel tightness in the mouth, but, as practice shows, most people simply do not pay attention to this.
Plaques with a diameter of no more than 4 centimeters are formed. They may appear:
- on the inner surface of the cheeks;
- on the tongue (on the back or sides);
- in the sky;
- on the gums;
- in the corners of the mouth.
The process of plaque formation takes up to one month. At the first stage, the area of the future formation seems slightly swollen; when you feel it with your fingers, the compaction is not felt. However, over time, another symptom of oral leukoplakia appears - the mucous membrane at the site of the swelling loses its original shine and becomes rough, which is noticeable when touched.
There is no pain in this case: only sometimes a feeling of dryness at the site of the outbreak is possible.
Gradually, the color of the spots changes from gray to bright white. The spots in most cases have clear boundaries. Their increase is possible when the disease enters its second stage, called verrucous.
The disease often causes candidiasis and malignant cancers. In an advanced state, leukoplakia is very difficult to treat: the affected areas become even more keratinized, ulcers can form, and the infection gradually spreads to other areas of the mouth.
1.General information
The oral mucosa is characterized by a number of distinctive features.
It is located in close proximity to vital organs, endocrine glands, lymph nodes; serves as a covering for the “entry gate” for the digestive tract and respiratory tract; it is intensively innervated, supplied with blood, moisturized, and renewed very quickly. Therefore, this mucous layer, extremely sensitive to any physiological, hormonal, biochemical changes in the body, can serve as a reliable early indicator of a pathological process, which sometimes begins in a completely different zone and system. Moreover, it is specific changes in the oral mucosa, discovered, for example, during a dental examination or treatment, that often turn out to be the first and at that time the only sign of a particular disease, sometimes formidable and severe, but progressing asymptomatically until a certain stage.
A must read! Help with treatment and hospitalization!
Kinds
- The most common is simple or, as it is also called, flat leukoplakia . It is usually discovered by chance during an examination by a dentist, since the patient does not experience any subjective sensations. A burning sensation occurs extremely rarely, and the appearance of the mucous membrane may change. If the disease affects the tongue, loss of taste may occur.
- Hairy leukoplakia of the tongue resembles stomatitis. The shape of the spot that appears, as well as its size, can be different, the color - from pale gray to white. The surface of the mucous membrane at the site of the lesion becomes slightly rough, which can be felt to the touch. On the cheeks it appears as solid or broken lines. It can also be found on the lips, where it looks like thin paper pasted on.
- Verrucous leukoplakia is the second stage of the development of the disease. The keratinization thickens, the affected area seems to rise above the nearby tissues. When you touch it with your fingers, you feel a compaction.
- Erosive form . Untimely diagnosis of the two previous stages of the disease leads to a worsening of the situation - the person feels pain when exposed to any irritants, erosions or ulcers are visible in the mouth.
- Soft leukoplakia is a type of cancer. Its distinctive feature is peeling of tissue in the area of the lesion. To clarify the diagnosis, a histological method of studying cells is required.
- Tappeiner's leukoplakia . This form of the disease affects people who abuse smoking. According to studies, daily smoking 10 cigarettes a day increases the chance of developing the disease by 50 times (as the number of cigarettes increases, the risk also increases)
The disease begins with the formation of lesions on the roof of the mouth (sometimes they appear on the gums). The mucous membrane changes its color to a pronounced gray or bluish, which is noticeable to the naked eye, folds appear on it. Reddish nodules may begin to appear, which is accompanied by infectious inflammation of the oral cavity (caused by the accumulation of salivary gland secretions in the tissues).
Diagnosis of oral leukoplakia
Treatment of any disease begins with diagnosis: leukoplakia is no exception in this regard.
During the examination, the doctor interviews the patient to determine the factors contributing to the development of the disease. These include regular exposure to tobacco smoke, working in hazardous conditions, recent dental surgery, etc.
Next, laboratory tests are prescribed. The following procedures can be carried out:
- tissue sampling (biopsy). Accompanied by anesthesia;
- examination of the collected material under a microscope. The method allows you to determine the presence or absence of cancer cells in the formation;
- a smear of the mucous membrane is taken;
- A Schiller test is done (the mucous membrane is stained with a solution consisting of water and iodine - foci of leukoplakia are not stained);
- blood is taken for analysis (an increase in ESR may indicate the presence of malignant neoplasms).
In addition, the doctor may additionally prescribe a urine test, conduct a biochemical blood test and request the result of fluorography. You may need to consult an oncologist (if cancer is suspected), a therapist (to rule out infectious diseases) and a dermatologist (to look for other foci of disease).
Leukoplakia of the oral cavity: treatment with medications
Treatment involves the complete elimination of irritating factors that led to the development of the disease:
- to give up smoking;
- grinding down sharp edges of teeth;
- sanitation of the oral cavity;
- replacement of fillings;
- use of products to protect the surface of the lips.
Additionally, a course of vitamin A is prescribed, lasting at least a month, which inhibits the process of tissue keratinization.
If the measures taken do not cause complete disappearance of the manifestations of the disease, surgical intervention is allowed: the lesion is excised, depending on the degree of development of the disease, cryodestruction or electrocoagulation is used.
Ulcers deserve special attention, as they can develop into cancerous tumors. For their treatment, drugs are prescribed that enhance the process of tissue regeneration and epithelization. If there is no positive dynamics, surgical intervention cannot be avoided.
A person with leukoplakia must constantly visit the dentist for examination to prevent malignant degeneration of the cells.
In addition to quitting smoking, the patient’s diet is adjusted: during treatment, spicy and too salty foods are excluded from the diet, and it is recommended to eat more vegetables and fruits.
Drugs prescribed:
- products that restore the epithelium (the most effective was 30 percent tocopherol acetate, which is applied to damaged areas three times a day for 15 minutes, after which it is washed off with water);
- antiseptics (after each meal it is recommended to rinse your mouth with a solution of chlorhexidine at a concentration of 0.05%);
- analgesics (their use is justified in the presence of pain. Lidocaine, applied to the mucous membrane before meals, has worked well).
Under no circumstances should you use drugs that have an irritating effect, as otherwise this can lead to the formation of cancer cells.
If there is no improvement within a couple of weeks, surgery is prescribed: this can be either excision with a scalpel or the application of cold in the form of a liquid stream of nitrogen.
Mechanical injuries of the oral mucosa in children.
Depending on the duration of the injury, its intensity, and the reactivity of the body, hyperemia of the damaged area, swelling, desquamation of the epithelium, erosion or ulceration of the mucous membrane are detected. Traumatic lesions are often called decubital (from the Latin Decubitas - bedsore).
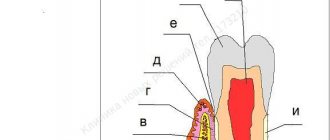
One of the causes of decubital erosions and ulcers in children in the first weeks or months of life is trauma to the teeth or one tooth that erupted before the birth of the child or in the first days and weeks after birth. Usually one or two central incisors erupt prematurely, mainly on the lower jaw.
The enamel and dentin of these teeth are underdeveloped, the cutting edge is thinned and during sucking the breast injures the frenulum and the lower surface of the tongue, which leads to disruption of the epithelial cover and inflammation in the mucous layer itself. This form of damage is classified as erosion. If, as a result of injury, the mucous layer itself is destroyed, then such damage is called an ulcer.
A similar lesion on the tongue frenulum can also occur in older children during whooping cough or chronic bronchitis, since prolonged coughing attacks are accompanied by protrusion of the tongue and the tongue frenulum is injured by the cutting edge of the front teeth (Rigi's disease).
Decubital erosions and ulcers of the cheek or lip can occur during the period of changing teeth, when the root of a baby tooth, which has not resolved for any reason, is pushed out by a permanent tooth, perforates the gum and, protruding above its surface, permanently injures the adjacent tissues.
In children from 1 to 2-3 years old, thin and flat foreign bodies (pumpkin and sunflower seed shells, apple core plates, fragments of toys, etc.) are often observed stuck to the hard palate.
Mechanical damage is common in children who have uneven, sharp or damaged teeth and a bad habit of biting, sucking the tongue, mucous membrane of the cheeks and lips between the teeth.
CLINICAL PICTURE OF MECHANICAL INJURIES OF THE ORAL MUCOSA IN CHILDREN.
In case of mechanical damage to the oral mucosa, the general condition of the child is not disturbed, sleep is calm, body temperature is normal. In case of defects in the upper layers of the epithelium resulting from habitual biting of the mucous membrane, eating is painless, children do not complain and do not consult a doctor. The doctor detects such lesions by examining the oral mucosa during routine sanitation. The mucous membrane is of normal color, but in those areas where it is injured by the teeth (in the cheeks, lips, along the edges of the tongue), its surface is uneven, fragments of white epithelium are visible, reminiscent of plaque from thrush, and sometimes there are small hemorrhages. Palpation of the mucous membrane in such children is usually painless. Foreign bodies stuck to the palate are covered with plaque, the mucous membrane around them is somewhat swollen and hyperemic.
Traumatic erosions have an irregular shape, are covered with a thin fibrinous coating, whitish-yellow in color, the surrounding mucous membrane is slightly or moderately hyperemic. Decubital ulcers come in different sizes and depths, have dense edges raised above the level of the surrounding mucosa, the bottom of the ulcer is covered with plaque, the surrounding mucosa is swollen and hyperemic. A young child becomes restless, sucks poorly at the breast or refuses it altogether. In children of preschool and school age, especially with bad habits, an eroded or ulcerated area of the mucous membrane is less painful, since prolonged irritation disrupts the function of the nerve receptors of the mucous membrane, and children often consult a doctor only when the process worsens due to secondary infection and the inflammatory reaction of the surrounding tissue accompanied by edema, lymphadenitis, etc.
When differentiating traumatic lesions and other chronic diseases of the oral mucosa, it should be remembered that decubital erosions and ulcers are observed only in areas accessible to biting; they never occur on the palate, arches, in the depths of transitional folds, or in the central areas of the back of the tongue. From the anamnesis it turns out that most children are practically healthy, some have psycho-emotional instability.
A peculiar lesion of the oral mucosa in children in the first months of life is the so-called Bednar aphthae, which more often occurs in weakened children who are bottle-fed, suffering from congenital heart defects, or who have suffered any diseases in the first months of life. Hypertrophy is the background against which minor tissue trauma by a long horn or while wiping a child’s mouth is sufficient to disrupt the epithelial cover. Erosions are most often located symmetrically at the border of the hard and soft palate, respectively, according to the projection onto the mucous membrane of the hook of the pterygoid process of the main bone. The defeat can also be one-sided. The shape of the erosions is round, less often oval, the boundaries are clear, the surrounding mucous membrane is slightly hyperemic, which indicates a state of hypergia. The surface of the erosions is covered with a loose fibrinous coating, sometimes clear, brighter in color than the surrounding mucous membrane of the palate. The size of erosions ranges from a few millimeters to extensive lesions that merge with each other and form a butterfly-shaped lesion. If a secondary infection occurs, erosions can turn into ulcers and even cause perforation of the palate.
Bednar's aphthae can also occur during breastfeeding if the mother's nipple is very rough, for example, after irradiation with quartz. Erosion in this case is located along the midline of the palate. The child becomes restless. Having started to actively suck, after a few seconds he stops sucking and crying, which is usually the reason for contacting a doctor.
TREATMENT OF MECHANICAL INJURIES OF THE ORAL MUCOSA IN CHILDREN.
For traumatic lesions of the mucous membrane, treatment is reduced to eliminating the cause that caused the injury. Prematurely erupted milk teeth should be removed, since their structure is defective, they quickly wear out and, in addition to trauma to the mucous membrane, can cause odontogenic infection. Foreign bodies from the mucous membrane of the palate are easily removed with a dental spatula.
In case of aphthae of newborns, it is necessary first of all to establish feeding of the child: natural through a pad for rough nipples of the mother or artificial through a short horn made of hard rubber, which does not stretch when sucking and does not reach the eroded surface.
To treat the oral cavity of children in the first months of life, weak antiseptics are used (0.5% solution of hydrogen peroxide, decoction of chamomile flowers, St. John's wort, tea, infusion of sage leaves). Vigorous wiping of the mouth and the use of cauterizing substances are unacceptable. It should be borne in mind that Bednar's aphthae heal very slowly, over several weeks or even months.
In older children, in case of injury, the sharp edges of the teeth are carefully ground off, the oral cavity is sanitized, and if indicated, drugs that suppress the cough center are prescribed (after consultation with a pediatrician). The role of bad habits is explained to the child and parents. If a conversation with children and parents does not produce results and the bad habit persists, the child should be referred for examination and treatment to a psychoneurologist. In some children, mainly with cicatricial deformities of the mucous membrane of the cheeks, when the mucous membrane is pinched between the upper and lower dentition, the manufacture of orthodontic appliances with vertical extensions that protect the mucous membrane is indicated.
For decubital ulcers, in addition to antiseptic treatment, it is advisable to prescribe applications of mixtures that stimulate healing (for example, vitamin A 500,000 units, vitamin B1 0.5 - 1 g, insulin 50 - 100 units, sea buckthorn, olive or sunflower oil up to 100 g). You can also use such official keratoplasty agents as vinylin, caroolin, rosehip oil, tesana emulsion, etc. Gauze napkins soaked in keratoplasty agent cover the corresponding group of teeth, isolating them from the affected mucous membrane. Small children can be allowed to suck on the indicated products on a small cotton swab stitched with a silk ligature.
Oral leukoplakia: how to treat it at home
In addition to drug treatment, oral leukoplakia can be treated with traditional medicine.
There are many recipes, here are just the main ones:
- rinsing with herbs (infusions of oregano, chamomile, ginseng and other adaptogens that reduce the inflammatory process and increase the body’s resistance to harmful factors are suitable);
- regular consumption of nuts and tinctures based on them;
- rinsing with decoctions of calendula, St. John's wort, eucalyptus. Alternation works well - once the oral cavity is rinsed with a soda solution, after a couple of hours - with an infusion of herbs. This procedure should be repeated at least 5 times a day;
- lubricating the lesions with sea buckthorn and olives (the fruits must first be mashed in your hands so that the juice appears).
Timely detection of the disease and compliance with all doctor’s recommendations is the key to recovery in the shortest possible time and reducing the risk of complications. If you start treatment at the initial stage, you can reduce the likelihood of complications to almost zero.
Types of disease
The clinical picture of oral candidiasis is classified:
- For clinical and morphological.
- With the flow.
- By localization.
Clinical and morphological is divided into:
- Hyperplastic.
- Erosive-ulcerative.
- Pseudomembranous.
- Atrophic.
The clinical picture, classified according to the course, is divided into:
- Chronic.
- Spicy.
By localization:
- Cheilitis.
- Gingivitis.
- Glossitis.
- Stomatitis.
- Tonsillitis, etc.
Based on the clinical picture, oral candidiasis comes in several types:
- Chronic hyperplastic.
- Candida infection.
- Chronic atrophic.
- Acute pseudomembranous.
- Chronic pseudomembranous.
- Acute atrophic.