Dental prosthetics is an invaluable invention that has impacted the quality of life of many dental patients. What is prosthetics? This is the only possible way to replace lost teeth, which restores the integrity of the dentition, which means it returns chewing function, comfort and a beautiful smile to people. In modern dental prosthetics, various highly effective methods, technologies, and high-quality safe materials are used. With the help of modern orthopedic structures, it is possible to restore the dentition with edentia of any complexity. However, under certain circumstances, after prosthetics, the patient may encounter complications. In this article we will talk about the risks of prosthetics and how they can be avoided.
What complications arise during dental prosthetics?
The most common problems that occur after dental prosthetics are:
- pain, discomfort in the mouth;
- irritation of the mucous membrane, denture stomatitis;
- dysfunction of the temporomandibular joint;
- galvanic syndrome;
- periodontitis;
- decementing and destabilization of fixed orthopedic structures;
- damage, chips of the facing material of crowns, dentures;
- failure of fixed dentures
- intolerance to orthopedic construction materials.
We will tell you in detail about each problem.
Complications after dental prosthetics
I warmly welcome you all. For all intents and purposes Marat Aslanovich. I want to tell you about the complications that arise after dental prosthetics.
Dental prosthetics is a procedure for restoring teeth using individual veneers, crowns or bridges. It requires careful preparation and compliance with the rules to restore the functionality of the dentition and aesthetics. Sometimes, after the final stage of prosthetics (fixation of permanent structures), complications may arise - unfortunately, no one is immune from this.
Why do complications arise after prosthetics?
The main causes of complications after prosthetics are: lack of a specific treatment plan, incomplete history taking and incorrect diagnosis.
In my opinion, the first consultation between a patient and a doctor is one of the most important procedures. On it, the dentist can collect as much information as possible to draw up a treatment plan, conduct an examination, assess the degree of hygiene, the condition of the oral cavity as a whole, collect a complete anamnesis and note the patient’s complaints, wishes, conduct a photo protocol and x-ray diagnostics (CBCT).
In ordinary cases, the doctor can immediately pre-orient the patient on what he needs to prepare for, in what time frame and finances the entire treatment will cost. In more complex situations, a second joint consultation with a therapist, surgeon or orthodontist with additional diagnostic tools may be necessary.
So what types of complications after dental prosthetics are there?
Stomatitis and Gingivitis (inflammatory processes of the gums.)
Diseases of teeth under dentures (caries, pulpitis, periodontitis.)
Periodontitis (inflammatory processes of all tissues surrounding the tooth.)
Allergic reactions to materials used in prosthetics.
Galvanic syndrome.
De-cementation and loosening of a fixed structure (poor quality fixation of the product)
Chips of the lining of artificial teeth and crowns, fractures of bridges.
Problems with the occlusal plane and changes in bite.
Let's look at them in more detail.
The development of inflammation of the gingival tissue - as a result, leads to gingivitis, stomatitis in acute and chronic forms.
As a rule, such a complication in the oral cavity occurs due to poor fit of the orthopedic structure or the doctor’s failure to comply with the rules of biological width, when the crown is buried deep under the gum. The process has the following course: in the first case, between the crown and the ledge of the tooth there is a gap where plaque accumulates, provoking local inflammation of the gums. In the second case, the structure puts pressure on the tissue, blood vessels die, there is no blood supply to the tissue, and inflammation develops. Both reasons can lead to rapid recession and eventual tooth loss.
How to solve a problem?
It is recommended in the first case to replace the fixed structure with a new one with an exact marginal fit to the tooth, and in the second case to also replace the structure, but with surgical correction.
Caries – as a result, the supporting teeth are affected by pulpitis or periodontitis
.
This usually happens if the caries has not been removed before the crown is installed. As a rule, so-called “secondary caries” can often be hidden under old fillings, which is often very difficult to identify at the time of treating the tooth for a crown or veneer without completely removing the old filling. Therefore, it is necessary to change all old fillings before dental prosthetics.
How to solve a problem?
If it is pulpitis or periodontitis, then it is necessary to remove the crown, treat endodontically the root canals of the causative teeth, preferably using an operating microscope, and install a temporary crown. After 6 months, carry out an X-ray control, if the dynamics are positive, install a permanent crown.
Periodontitis is an inflammatory lesion of the surrounding tissues of the tooth, leading to disruption and weakening of its ligamentous apparatus.
Often obvious destructive changes are noticeable around the crown: the gums acquire a bluish tint, swelling and bleeding of the tissue develops. As a result, this leads to exposure, mobility and loss of the tooth.
How to solve a problem?
First you need to check the depth of the lesion, take an x-ray (CBCT) and remove the crown. You will definitely need the help of a periodontist surgeon; hygiene correction is possible. There are also cases of penetration of cement residues into the periodontal sulcus when fixing crowns. Therefore, it is necessary to carefully clean out excess cement during fixation of orthopedic structures.
Rejection of the structure due to an allergic reaction.
It can manifest itself as swelling of the gums, itching, rash and redness in the mouth. In some cases, difficulty breathing and a constant feeling of dry mouth and fever may occur. Allergies may appear in the first few hours after installation of an orthopedic structure or after several weeks.
How to solve a problem?
It is necessary to establish which component of the prosthetic structure the patient is allergic to. It will be necessary to replace the crown with a new one, taking into account allergy tests. That is why, at the stage of planning prosthetics, it is important to study the medical history and make sure that the patient does not have an allergy to metal.
Development of galvanism - leads to the production of galvanic current
.
What usually happens when using structures with a metal frame is that saliva gets on the material, the patient feels a taste of iron in the mouth, a constant feeling of an acidic environment in the oral cavity, and discomfort. As a result, the crowns darken, aesthetics are impaired, and sometimes the problem is accompanied by a headache.
How to solve a problem?
Replace the prosthesis with a product made of ceramic material. When installing ceramic structures, galvanism does not occur.
Poor quality fixation of the product.
As a rule, crowns and veneers are fixed with special dental cement, the strength of which should be enough for at least 20 years. The denture can come off due to overload, but it must be simply prohibitive, incorrectly selected shape or size of the crown, or too small a tooth area. Also, the reason for the crown coming off may be due to moisture getting on the treated tooth during fixation.
How to solve a problem?
To establish the cause of decementation of the orthopedic structure and select the appropriate solution to correct this pathology. It is possible to either reinstall the same structure or make a new one.
Violation of the integrity of the orthopedic product.
These can be chips, cracks, breaks, breaks into halves or small parts. The denture can become deformed due to impacts to the jaw projection, accidents, falls, or eating too hard foods. Sometimes the product is deformed due to errors in prosthetic planning.
How to solve a problem?
If the deformation is minor, the structure can be repaired directly in the oral cavity. Sometimes removal and re-fixation may be necessary. If the damage is serious, the prosthesis will have to be removed and a new one put in its place.
Change in bite.
The height of dental crowns plays a big role. For example, with a lack of height, the quality of chewing decreases - a low-quality food bolus is formed. When the height of the crowns is high, the jaw is overloaded, which provokes dysfunction of the temporomandibular joint.
How to solve a problem?
Determine the main cause of the development of malocclusion, re-plan prosthetics with replacement of the structure.
If complications arise after prosthetics, what should you do?
First, be sure to contact the doctor who performed the treatment.
Secondly, follow all the specialist’s recommendations. For minor complications, the patient may be recommended local treatment: treating the cavity with solutions, using regenerating gels.
Thirdly, it may be necessary to adjust the orthopedic structures or completely replace the products, taking into account the existing negative experience with prosthetics.
Dear patients, there is no need to waste time - the complications that arise will not go away on their own. Also, do not rush into prosthetics. It is important to go through all stages of diagnosis and plan everything carefully and you will definitely get a high-quality and long-term result of your treatment. I wish you all Good and Health, with respect, Marat Aslanovich.
Discomfort from the prosthesis
This problem may arise due to errors during installation of the structure or in the event of a mismatch between the denture and the size and shape of the jaw.
What kind of discomfort can we talk about?
- 1
the prosthesis interferes with the normal pronunciation of words; - 2
there is a constant sensation of a foreign body in the oral cavity;
- 3
the prosthesis rubs contact surfaces (mucosa, gums);
- 4
salivation increases.
Discomfort from wearing a new denture for a few days to 2 weeks is normal. If discomfort in the mouth does not go away for a long time, you need to contact an orthopedic dentist to correct the orthopedic structure itself or correct installation errors.
Wrong choice of product size
The knee endoprosthesis, as well as the hip joint prosthesis, is now available in a wide range of sizes, shapes and leg widths. Thanks to this, the surgeon can choose the most suitable design for each case.
But choosing products by size is a very responsible, serious process. Mistakes made in it can lead to serious problems:
- when installing a small product, rapid loosening of the elements is likely;
- a design that is too large leads to bone fractures.
Often, a negligent approach and a negative result of treatment are explained not so much by the actions of the surgeon, but by the limitations of a particular clinic (when the patient is fitted with structures that are in stock at the medical center, so as not to delay surgical manipulation).
Prosthetic stomatitis
Denture stomatitis is a consequence of the inflammatory process that develops in the gum tissue under the denture.
The cause of inflammation may be:
- improper fixation, excessive pressure of the structure on the gum, due to which blood circulation in the tissues is disrupted, bedsores appear, ulcers form, and the necrotic process begins
- diabetes;
- long-term use of steroids and some antibacterial drugs;
- low quality of oral hygiene.
In response to inflammation of the mucous membrane, the lymph nodes may become inflamed. The treatment program for prosthetic stomatitis will depend on its causes. If necessary, the installation of the prosthesis is corrected. As part of preventative treatment, proper, thorough hygiene is key. Additionally, the oral cavity can be sanitized with antiseptic drugs.
Loose contact between teeth: treatment errors.
Greetings, dear readers, Marat Aslanovich is with you. Today I want to talk about loose contact between teeth, which is one of the mistakes in dental prosthetics and implants.
Let's first figure out what contact between teeth is and what it is like normally.
Our teeth are located in the mouth in such a way that their lateral surfaces touch each other and thereby create a continuous arch, which is a single whole and forms a beautiful smile. This is provided that the person does not have any pathologies of the bite and maxillofacial system or there are no missing units.
The contact point is easy to detect if you pay attention to the interdental spaces - they have a triangular shape in the gingival region, and the tip or apex of the triangle is directly facing the point of contact of the teeth.
If you open your mouth and look in the mirror, you will see that each tooth on the outer side visible to you, in addition to the very frontal crown part, has a cutting edge, a neck and two contact surfaces on each side. In those places or points where the tooth comes into contact with its neighbors, a contact point is formed. Incisors, canines, premolars always have two adjacent contacts on both sides (medial and distal) and only the outer molars in the row have only one such contact point (we are talking about sevens or eights, i.e. wisdom teeth, if you have any There is).
Types of contact points:
- Spot. This type of contact is typical for children who have recently erupted teeth and for young adults. The crowns themselves in the area of contact have an almost ideal round or spherical shape, so they only contact each other pointwise.
- Planar. This type is typical for mature and elderly people, because... Over the course of life, the enamel gradually wears out and wears out, and the coronal part in the lateral areas gradually becomes flat as a result of friction and physiological mobility of the units. As a result, the lateral surfaces of adjacent teeth are no longer limited to point contact.
Why are contact points needed?
The importance of dental contact points cannot be underestimated, because the health of the oral cavity as a whole, the condition of the maxillofacial system, and the aesthetics of a smile depend on their correct structure and location.
So, let's take a closer look at what having an anatomically correct contact point gives:
- The teeth have the ability to lean on each other and provide each other with support.
- Each tooth occupies its designated place in the row and is protected from loosening and displacement.
- If there is a contact point, the chewing load is correctly redistributed.
- The gingival papillae that fill the interdental spaces remain protected from food particles and injury.
There are several methods for restoring contact points. We are interested in the example with crowns.
After prosthetics, the patient should have a dense planar contact point between the crown and adjacent teeth. Also, dental floss should pass smoothly between the teeth with a certain click, without losing its integrity.
Before fixing the crown, the doctor must check the contact points.
If the dental floss breaks when inserted between the teeth, then the contact is too tight and the doctor can use a special rubber band to remove excess ceramics and achieve good contact, but if the floss passes too freely between the teeth, even without particularly contacting the walls, then a crown correction is necessary dental laboratory.
There are also cases when good contact between the crown and the tooth can only be achieved by restoring the contact wall of the adjacent tooth (by replacing a defective filling with a new one, or by curing contact caries), this is the case when the contact wall of the tooth has a certain defect.
And there are cases, especially with prosthetics on implants, when a tooth was removed several years ago, and the neighboring one leaned towards the defect, then in order to achieve tight contact the prosthetist will need the help of an orthodontist, who, using special microscrews, will return the leaning tooth to its place, and contact between the latter and the crown on the implant will be excellent.
I hope that this article was useful to you and that everyone was able to emphasize something new and educational for themselves. An orthopedic dentist from the Belaya Medveditsa clinic was with you, take care of yourself, see you soon, the main thing is don’t get sick.
Temporomandibular joint dysfunction
One of the most unpleasant and dangerous complications after prosthetics is disturbances in the functioning of the temporomandibular joints. The dentofacial apparatus is a complex system in which each tooth, facial muscles and joints play a huge role. Any problem with teeth (displacement, loss of one/several teeth) increases the load on the chewing muscles, which leads to their rapid fatigue and the appearance of uncomfortable tension during chewing and when speaking. As a result, we have increased stress on the temporomandibular joints and joint dysfunction.
It is impossible not to notice pathological changes, since with joint dysfunction the patient develops characteristic symptoms: the jaw crunches near the ear when opening/closing the mouth, when chewing, the jaw hurts and movement restrictions appear (it is not possible to open the mouth wide or there is a restriction when moving the jaw in one direction). side). With ANS dysfunction, painful sensations are not limited only to the masticatory apparatus. Patients complain that half of their face and neck hurt, and they often have a headache. A person constantly feels tired.
Pathological processes in the ANS cause the development of other pathologies:
- bruxism (strong teeth clenching, teeth grinding during sleep);
- stoop (due to constant tension of the sternocleidomastoid muscles).
How to avoid temporomandibular joint dysfunction?
The most effective way to prevent dysfunction of the ANS is a thorough diagnosis at the stage of preparation for dental prosthetics. To identify problems in the dentofacial apparatus, a special study is carried out (the so-called “orthopedic diagnostics”), which makes it possible to analyze the relationship of the lower jaw to the upper, the correct occlusion of the teeth, and the work of the masticatory muscles when closing the jaw. Based on the impression, the movement of the patient’s lower jaw is reproduced in a special device (articulator). Such a study provides the specialist with information about the state of the entire dental system, allows for precise prosthetics taking into account the structural features of the jaws and dentition, and eliminates complications from the temporomandibular joint.
Mistakes when using removable dentures
Dental prosthetics using removable dentures these days is one of the most popular ways to restore a beautiful smile, feel the taste of food and not have problems chewing any, even the hardest food.
This type of prosthetics is good for everyone - from the affordable price to the ability to remove the prosthesis, thereby reducing the load on the jaw and avoiding constant discomfort. However, if restoration of the integrity of teeth with removable dentures is performed incorrectly, quite serious errors can occur, the price of which is sometimes extremely high.
The Aviadent clinic is the best dentistry near the Komendantsky Prospekt metro station, where you can contact with any dental problems.
As a rule, the list of errors when installing removable dentures is quite standard and includes several categories of problems:
1. Choosing . An example would be the production of an arched prosthesis when a large number of teeth are lost. It should be noted that such an error can be eliminated through consultation with a more qualified specialist and alteration of the prosthesis.
2. Incorrect used as supporting teeth, or selection of unsuitable teeth. Often, such a nuisance occurs due to incomplete collection of anamnesis, neglect of X-ray data, or in the absence of studies of diagnostic models;
3. Inaccuracies made by the dentist when preparing the oral cavity for prosthetics or a complete lack of preparatory procedures.
4. Errors - taking an impression from only one jaw, or with alginal material; deformation of the print.
Affordable prices, modern technologies and an individual approach to the client. Favorable conditions for removable dental prosthetics for everyone!
5. Errors . There are situations when the dentist inattentively examines a removable denture, thereby missing various minor defects, which in the future can lead to serious consequences.
6. Inattentiveness - failure by the doctor to comply with the rules of asepsis and antisepsis or the principle of completeness of treatment.
It is quite possible to prevent the occurrence of all of the above errors when using removable dentures. All that needs to be done for this is to contact qualified specialists who know their business well, have extensive experience and the necessary equipment.
Galvanic syndrome
If metal is present in the denture structure, it is very important that all subsequent dental prostheses are made from this metal. The fact is that different metals have different electro-mechanical characteristics, which can lead to the occurrence of galvanic currents upon contact with an electrolyte (saliva plays the role of an electrolyte in the oral cavity).
Symptoms of galvanic syndrome:
- 1
the appearance of a sour or metallic taste in the mouth, a feeling of soreness;
- 2
changes in taste sensations (for example, a feeling of bitterness when eating sweets);
- 3
burning sensation on mucous tissue, tongue;
- 4
increased saliva viscosity, dryness;
- 5
pathological changes in mucous tissue - the appearance of swelling, redness, numbness;
- 6
sensation of electric current flowing in the gum tissue, along the teeth, tongue or in the palate;
- 7
hypersensitivity of the gums and tongue;
- 8
change in color of dentures (darkening).
Galvanic syndrome causes not only local discomfort in the oral cavity, but can also cause a general deterioration in the patient’s well-being.
Complications during the period of reparative bone tissue regeneration
- Inflammation of the bone tissue around the implant (peri-implantitis).
- Implant rejection.
The cause of peri-implantitis is inflammation of the soft tissue in the surgical site, which leads to the destruction of the bone tissue surrounding the implant. This condition can be caused by the presence of a hematoma over the plug of the intraosseous element and its subsequent suppuration, as well as incorrect preparation of the bone bed, closure of the postoperative wound and the condition of the oral cavity, which leaves much to be desired.
Treatment of peri-implantitis is carried out as follows:
- Plaque is removed from the part of the implant protruding into the oral cavity.
- The implant cuff is detoxified using a citric acid solution for 1 minute.
- The gingival cuff is treated with antibacterial gel.
- Drug therapy is carried out.
- Hygienic care of the oral cavity is recommended (rinsing with antiseptic solutions).
If the measures taken did not produce results, and the inflammatory process could not be stopped, or after some time a relapse of peri-implantitis was discovered, then the implant must be removed.
Implant failure is essentially an inflammatory process that begins in the bone surrounding the implant and spreads to adjacent areas. Rejection can be caused by thermal damage to the bone tissue during the preparation process (which leads to the formation of granulation tissue between the implant and the bone), as well as osteoporosis of a specific area of the bone tissue and insufficient blood supply (which leads to necrosis of the bone around the implant). There is only one way to get rid of this problem - removing the implant.
Periodontitis (inflammation of the periodontal tissues)
The development of periodontitis after prosthetics is most often associated with improper formation of the stump for the prosthesis (without a ledge) and the wrong choice of orthopedic design. In this case, the gums acquire a bluish tint, begin to bleed, swell, and over time, recession of the gum tissue begins. This, in turn, leads to the exposure of the unaesthetic gray edge of the orthopedic structure, and can also have unpleasant consequences for the health of the tooth itself, since inflammation spreads to all periodontal tissues, leading to damage and atrophy of the jaw bone, and tooth loss.
Peeling off the permanent structure
Artificial teeth are fixed using special dental cements. High-quality cement ensures reliable and stable fixation. However, there are cases when the crown begins to wobble, which indicates decementing or peeling off of the orthoconstruction.
Why is this happening?
- due to heavy loads on the prosthesis;
- due to improper preparation (grinding) of the tooth for a crown;
- if the supporting tooth has several small or one large filling (then the fillings are glued to cement and removed together with the crown);
- due to the large length of the bridge structure;
- if cement of poor quality or expired was used.
Incorrect (inappropriate) type of fixation
Installation of a hip and knee endoprosthesis involves fixation in one of 2 ways – cemented or cementless. The doctor must decide which option to use in a particular case, taking into account the patient’s gender, age, weight and lifestyle, diagnostic results (density and shape of the bone canal), and the characteristics of the prosthesis components.
At the same time, in practice, some decision-making rules have already been formed:
- cemented knee joint prosthesis is considered preferable for women and older patients (60 years and older), as well as people with severe symptoms of osteoporosis, wide channels and thinned walls of the femurs;
- installation of an endoprosthesis without cement is more often suitable for men and young people without severe forms of osteoporosis.
Errors in choosing the type of fixation
Choosing a cement method instead of a cementless one, and vice versa, can lead to serious complications. So, if a cemented installation is more suitable for a patient, and the elements of the implant were fixed without cement, the likelihood increases:
- crack formation;
- bone fractures (especially if it is the installation of a hip joint endoprosthesis );
- the need for reoperation.
When cementless fixation is required according to indications, and the implant is installed in a cemented composition, the patient will not simply require re-installation due to frequent dislocations or fractures. The revision operation will become significantly more complicated.
Errors when attaching components
An important point: even the correct method of fastening (cemented, cementless) does not eliminate the likelihood of complications associated directly with the process of installing a hip joint endoprosthesis, namely:
- insufficient amount of cement, which must be used to fill the acetabulum and femoral canal when installing a hip joint endoprosthesis using the cement method;
- uneven distribution of medical cement around the elements of the prosthesis (again, we are talking about a cement installation);
- incorrect choice of fixation site (orientation in the space of the bone bed). This error is possible with any method of fixation - cemented or cementless.
LEFT: Normal cement-metal interface (yellow arrow). However, there is weakening at the cementum-bone interface (orange curved arrow). RIGHT: Weakness at the cement-metal interface.
Chips in the lining of orthopedic structures
The outer layer of orthopedic products is made of ceramics. Thanks to the veneer, dentures and crowns look like real teeth – natural and aesthetically pleasing. The facing layer is quite durable, and subject to high-quality prosthetics and proper operation, orthopedic structures retain their original appearance and integrity for many years.
Chips of the aesthetic layer are possible for two reasons - errors at the planning stage, manufacturing of the orthopedic structure, and the patient’s violation of the ban on cracking nuts and gnawing bones.
In case of a chip, depending on the nature and size of the damage, you can correct the situation in two ways:
- 1
Replace the ortho construction.
- 2
Restore the facing layer without removing the prosthesis.
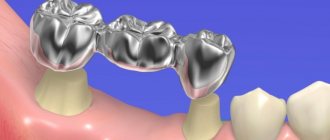
Failure of bridge orthopedic structures
This problem can occur with temporary plastic and permanent stamped-soldered products due to intense stress. The main reason is technical errors at the stage of modeling and production of the prosthesis. As for stamped-soldered structures, today their failure occurs extremely rarely, since very durable materials are used in the manufacture of dentures.
If a temporary plastic prosthesis breaks, there will not be a big problem, since it can be quickly replaced.
Individual intolerance
An allergy can be to both metal and plastic elements of the orthostructure.
If an allergic reaction occurs, patients complain of an unpleasant sensation in the mouth:
- the gums under the denture become sensitive and itchy;
- burning sensation under the crown;
- pain in the prosthetic bed;
- the appearance of dry mouth.
Moreover, sensitivity of the mucous membrane can occur both in the presence of signs of tissue inflammation, and in the complete absence of external symptoms of the inflammatory process. Allergic rashes around the mouth, difficulty breathing and other symptoms may appear.
Intolerance to materials used in the manufacture of dentures is a complication that is very rare in modern prosthetic dentistry. In case of individual intolerance, the best solution to the problem is to replace the denture with a product made of other materials that do not cause an allergic reaction in the patient.
What are the reasons for complications during prosthetics?
Most complications can be prevented even at the stage of preparation for prosthetics if you know the main causes of these problems.
We invite you to understand the reasons why complications arise after prosthetics:
- Insufficient preparation – if before the prosthetic procedure the patient refused to carry out the necessary treatment, therapeutic and preventive, hygienic procedures (caries treatment, professional hygiene).
- Error in size. If an error was made in the manufacture or selection of the type of orthopedic structure or prosthesis, wearing it will cause discomfort to the patient.
- Unprofessional, poor-quality installation of orthopedic structures. In this case, the patient may encounter various problems - from the accumulation of food debris in the elements of the prosthesis to the development of inflammatory processes in the oral cavity, or breakdown of the prosthesis itself.
- Allergy, the body's immune reaction to denture materials.
- Mobility, displacement of teeth - leads to displacement of the denture structure.
- Poor quality of oral hygiene after installation of a denture.
Solution
Errors in dental prosthetics usually occur due to improper work of the dentist. Any neglect of the necessary procedures preceding the actual prosthetics leads to irreversible complications. It will be impossible to correct/correct anything - you will have to remove the prosthesis (even permanent crowns and onlays), prescribe full treatment for the problem, and then repeat the prosthetic procedure again.
The dentist should never make concessions to patients - they often ask to install a prosthesis for carious teeth, not to pay attention to swelling of the gums (and this is a sign of inflammation), to choose the most expensive crowns. Such rashness has no place - the doctor must explain the situation to the patient in detail and inform the patient about the possible consequences. And patients themselves should be guided by the recommendations of professionals - this will be the key to obtaining the desired effect.
Oral hygiene after dentures
To maintain a healthy and beautiful smile, it is not enough to simply insert a tooth. You also need to take care of careful care of the oral cavity and the dentures themselves. Hygiene is the basis of dental health. After installing a denture, hygiene requirements increase, since food particles can get stuck in the elements of the orthopedic structure, plaque accumulates on the walls of the denture, and thus creates a favorable environment for bacteria - the main culprits of all diseases of the teeth and gums.
Care of fixed dentures:
- 1
regular brushing of teeth (recommended not only in the morning and evening, but also after each meal);
- 2
rinsing with special antiseptic preparations;
- 3
professional dental cleaning every 3 months.
Care will become much easier if you purchase an irrigator - a device that effectively washes away food debris in the most inaccessible areas of the oral cavity and is completely safe for dentures.
Rules for caring for removable dentures:
- after each full meal or snack, the denture should be removed and washed under running warm water;
- In the morning and evening, dentures, just like teeth, need to be cleaned (for this, use a toothbrush with soft bristles and a special paste for dentures);
- in order to prevent the accumulation of plaque, it is recommended to soak the denture in a special solution for 10-20 minutes after each cleaning;
- From time to time it is necessary to take your dentures to the dentist for cleaning;
- Removable orthopedic structures should be stored in clean water or a special solution for storing prostheses.
New generation removable dentures, made of high-quality polymers, are so comfortable that they can be left on at night.
POSTOPERATIVE COMPLICATIONS
Post-operative complications of dental implantation
| Complication | Norm |
| Nerve damage can cause severe numbness in part of the face. It can be observed for two weeks to 6 months, but in the end, as a rule, disappears on its own, as blood circulation is restored. | Do not confuse nerve damage and compression that occurs in the bone as a result of swelling after the installation of implants located close to the nerve endings. This type of pressure passes quickly enough and is normal. Improvements will be noticeable almost immediately after installing the prosthesis on the implants and activating the chewing load. |
| Injury to the maxillary sinuses can occur during implantation in the upper jaw. Incorrectly calculated dimensions of the implant can cause damage to the lining of the nasal sinus (it is simply pushed inside it, damaging it partially or completely ending up in the nasal cavity). Such a complication will require surgical intervention to restore the integrity of the membrane. The main consequences of sinus damage are prolonged runny nose and sinusitis. The main symptom of this complication is the leakage of a small amount of fluid from the nasal cavity. | This should not be confused with a situation where, due to the complexity of the clinical case, zygomatic implants are specially installed through the maxillary sinuses , or the wall of the maxillary sinus is moved back a little, but its integrity is maintained. This is an acceptable practice that has been used in maxillofacial surgery for more than 30 years; it is rarely resorted to and the doctor informs the patient in advance about the possible difficulties of the postoperative period. For transzygomatic (through the sinus) implantation, special implants with a polished antimicrobial surface are selected, and the installation strategy is carefully planned in 3D and on models. |
| sutures are separated - it is necessary to re-apply them, | slight discharge from the sutures in the absence of severe inflammation is normal; it can occur when using membranes or simultaneous grafting of bone tissue around the implant |
| Heavy bleeding immediately after surgery, more than 2-3 hours | Minor bleeding up to 48 hours after surgery. This is absolutely normal, as swelling increases in the first three days. |
| loss of the implant, which is possible due to a mismatch between the size of the hole and the structure itself, as well as weakness of the jaw bone. A good surgeon will exclude this type of complication immediately after surgery. | The implant lost its fixation after 14-18 days, but there is no inflammation in the bone, then this is an acceptable outcome. Such situations occur if the patient simultaneously has a number of chronic diseases (diabetes mellitus, osteoporosis), that is, the process of tissue regeneration is slowed down. The problem is solved by reinstalling implants using regenerative membranes (enriched with growth factors), as well as prescribing individual vitamin therapy. |
If there are symptoms of complications, such as increasing bleeding from the wound, acute pain that cannot be relieved with painkillers, chills, runny nose, body temperature above 38 degrees (on the 2nd day and beyond), swelling of the face, you should immediately go to the doctor.
Late complications
After implants are placed, it can take a long time for complications to arise. The main reason for their appearance is the deterioration of the patient’s health, injury or insufficient hygienic care.
- Peri-implantitis is an inflammation of the tissues that support the implant. It usually occurs as a result of poor oral hygiene and abuse of bad habits. If prompt measures are not taken, there is a high probability of rejection of the installed structure,
- Implant rejection is a serious problem that can be caused by poor fixation of the titanium “screw,” weakness of the bone tissue, or the body’s rejection of the foreign body. It is important to remember that there is a possibility of rejection even years after implant placement. It can occur due to poor oral care or exacerbation of chronic diseases (diabetes mellitus, acute decrease in immunity, dysfunction of the heart and vascular system),
- due to the low qualifications of the doctor, a problem may arise when the prosthesis cannot be installed on implant 2. This can happen due to incorrect calculation of the place where the implant should be located, as well as its incorrect installation relative to the level of the alveolar ridge.
Complications can arise both with immediate installation of a fixed prosthesis, and when using a protocol with delayed loading. But in practice, with classical implantation, there are more problems, since the technique involves a larger number of additional procedures (bone augmentation), a rather traumatic installation of implants with subsequent suturing, as well as the need to exclude multiple contraindications.
“The dentists at the Smile-at-Once clinic pay great attention to preparing for implantation. Sometimes this stage takes more than one day, since it is important to exclude all possible contraindications. Our goal is to give patients new teeth that will last for decades, and for this it is important to carefully work out a treatment plan, prepare the oral cavity and the patient’s body as a whole.”
Vasiliev Alexander Alexandrovich, implant surgeon, more than 10 years of experience make an appointment