Free webinars on anti-aging medicine Learn about the features of the Anti-Age Expert International School, as well as the opportunities for improving your medical practice every day.
The webinar program also includes fascinating reviews of innovations in anti-aging medicine and analyzes of the most complex clinical cases with recommendations that really work. Find out more
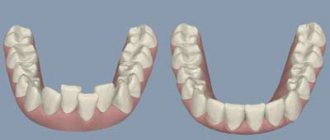
Caries
According to a study published in the medical journal The Lancet, 2.83 billion adults and children worldwide have tooth decay.
Cavities typically form when bacteria in plaque combine with sugar to form an acid that erodes enamel.
Treatment:
If you or your dentist catches tooth decay early enough, you may be able to reverse the process with fluoride medications. Otherwise, the classical treatment of caries is provided - filling.
However, if the decay gets so bad that a filling doesn't help, your dentist may crown the tooth or remove it. Again, early detection can prevent tooth decay and loss.
Gum diseases
Some form of gum disease, also called periodontal disease or periodontitis, affects nearly half of adults age 30 and older. Severity ranges from mildly swollen gums to bleeding gums and complete loss of teeth.
Most gum diseases develop in several stages:
- Plaque and tartar build up on the teeth, leading to gingivitis (inflammation of the gums).
- Gingivitis irritates the soft tissue along the gum line, which gradually leads to periodontitis.
- Periodontitis occurs when the gums separate from the teeth, forming pockets. This can lead to further gum infection, requiring treatment with antibiotics, surgery, or tooth extraction.
Treatment:
Like tooth decay, gum disease in the gingivitis stage is highly treatable if detected early. If it can't be corrected, your dentist will likely suggest scaling, a professional deep cleaning to remove all plaque from your mouth. As noted, antibiotics may also be prescribed. If periodontitis is advanced, surgery may be required.
“Periodontal disease is indeed a common problem. If such diseases are left untreated, sooner or later this will lead to the formation of deep and painful periodontal pockets, and ultimately to tooth loss. In addition, the microflora that lives in the mouth is very aggressive. Once it enters the bloodstream, it can spread and complicate the course of chronic diseases of the joints, heart, lungs, and brain, causing disruption in their functioning. The relationship between the presence of pathogenic microflora in the oral cavity and diseases such as Alzheimer's and Parkinson's disease has been proven. Getting dental plaque or the contents of periodontal pockets into the lungs when coughing can worsen the prognosis of any acute respiratory viral infection, as well as aggravate the course of COVID-19. Therefore, it is so important to monitor the condition of the periodontium, undergo preventive examinations every 6 months, and have a professional. oral hygiene, remove dental plaque, both hard and soft. When diagnosing gum disease, it is imperative to carry out timely treatment. For prevention, it is important to use simple care methods at home - brushing your teeth with high-quality toothpaste - 2 times a day, and also use dental floss, irrigators, and special rinses for additional hygiene.”
Kalashnikova Oksana Yurievna
dentist, implantologist-orthopedist, gnathologist, maxillofacial surgeon, specialist in aesthetic dentistry, candidate of medical sciences, doctor of the highest category, doctor of integrative interdisciplinary anti-aging medicine Work experience: 30 years
What bacteria inhabit the oral cavity?
The permanent microflora of the mouth consists of 30 strains of microorganisms that are responsible for the most important functions. These strains include: streptococci, veillonella and diphtheroids.
Almost 300 species of microorganisms constantly reside in the oral cavity. Among them there are pathogenic - harmful. Suitable habitats for parasites are braces and plates, carious cavities, crowns, gum pockets, and the back of the tongue. Some teeth have a soft but thick layer of yellow plaque, which over time turns into dark tartar - this is the focus of harmful microorganisms.
Bacteria and microbes form a unique environment that is maintained in the normal state of the body and is capable of self-regulation. In the normal state of the oral microflora, beneficial bacteria outperform pathogenic bacteria.
Systematic hygienic teeth cleaning at the dentist is an essential attribute of a healthy and beautiful smile.
Every time we accept another patient for caries treatment, we are convinced that the price of professional hygiene is disproportionate to the consequences and costs that will have to be borne if it is not done.
It has been proven that even correct, scrupulous and constant home care is ineffective. 90% of adults brush their teeth ineffectively.
Teeth cleaning at Unit using modern technologies: Air Flow and ultrasound gives the maximum effect in maintaining a healthy balance of microflora and local immunity.
Sign up for professional cleaning
Infectious diseases
An infection of the oral cavity leads to the development of a disease in which the mucous membranes become inflamed. The pathological process can involve the teeth and gums. Symptoms of infections in the mouth are often hidden, but sooner or later they appear.
Online training in Anti-Age medicine Learn the intricacies of anti-aging medicine from anywhere in the world.
For the convenience of doctors, we have created the Anti-Age Expert online training platform: Lectures from our educational programs are consistently posted here, and are accessible 24/7. Doctors can study the materials as many times as necessary, ask questions and discuss interesting clinical cases with colleagues in special chats. Find out more
Causes of infectious diseases of the oral mucosa:
- Uncontrolled medication use.
Treatment of any disease should be under the supervision of a doctor. Improper use of antibiotics, antibacterial and other agents leads to consequences, including diseases of the oral cavity.
- HIV and AIDS.
Infectious diseases of the mucous membranes of the oral cavity often occur against their background.
- The occurrence of infections in the oral cavity
may be associated with a weakened immune system.
- Poor nutrition.
If the mucous membrane is exposed to aggressive food, it injures it. Thus, the mucous membrane becomes more vulnerable and susceptible to infection.
In addition, smoking and alcohol provoke oral diseases. Those whose bodies are dehydrated or experience hormonal imbalances also face similar problems.
- Stomatitis.
There are many bacteria living in the mouth, and due to a decrease in immunity, they are activated. Thus, an infectious disease develops. One of the most common is stomatitis. It usually develops in people who brush their teeth incorrectly or not thoroughly enough. The disease can also occur due to tonsillitis or diseases of the gastrointestinal tract. There are several types of stomatitis:
- Catarrhal.
It is manifested by swelling of the oral mucosa. As catarrhal stomatitis progresses, plaque appears on the tongue.
- Ulcerative.
In this case, the lymph nodes become enlarged. This stomatitis is manifested by dizziness and weakness. May occur in people with stomach ulcers or enteritis.
- Aphthous stomatitis.
Leads to damage to the oral mucosa, on the surface of which erosions form. Aphthous stomatitis is associated with an imbalance in the gastrointestinal tract. Signs of aphthous stomatitis: swelling of the oral mucosa, malaise, erosion in the mouth.
- Diseases caused by viruses.
The best known oral infection is herpes, clinically known as herpes simplex virus type 1 (HSV-1). It is often found in children between 6 months and 5 years of age.
Once HSV-1 enters a child's body, he will carry the virus throughout his life. It is estimated that 50-80% of adults live with herpes simplex, either dormant or active.
The herpes virus manifests itself as rashes around the mouth. As the disease progresses, ulcers form in the mouth: they are localized on the inside of the lips and cheeks. Herpes can also infect tissues near the teeth.
After the first attack of oral herpes, the body produces antibodies to fight the virus and its effects. This way, your subsequent outbreaks of HSV-1 may not be as severe or the virus may remain dormant.
Otherwise, taking antiviral drugs may help.
- Candidiasis.
This is a manifestation of a fungal infection. Candida fungus microorganisms live in the mouth and are activated under the influence of unfavorable factors. Candidiasis occurs in people with weakened immune systems. To avoid illness, it is necessary to strengthen the immune system and avoid hypothermia. There are several types of candidiasis:
- Pseudomembranous.
It occurs in an acute form. As the pathology progresses, the mucous membrane of the cheeks begins to dry out, and the same thing happens with the lips and tongue. A coating of curd consistency forms on the tongue. Pseudomembranous candidiasis causes discomfort when chewing and itching. The disease can occur in people with a weakened immune system, as well as against the background of blood pathologies. Other causes of pseudomembranous candidiasis are diabetes mellitus and hypovitaminosis.
- Atrophic candidiasis.
In this case, the mucous membrane of the mouth becomes red and dry. The chronic form of the disease develops in those who use dentures for a long time.
- Hyperplastic candidiasis
may be acute or chronic. In chronic cases, plaque forms on the mucous membranes, including the tongue. When you try to remove it, the mucous membrane becomes more inflamed. Brushing your teeth may cause bleeding.
- A disease that occurs due to HIV.
Secondary immunodeficiency is characterized by the active proliferation of pathogenic flora in the oral cavity. Early diagnosis will allow faster initiation of treatment and improve the prognosis of immunodeficiency.
It is important to note that diseases of the oral cavity that occur against the background of HIV often become chronic.
In the process of evolution of living beings, including humans and microorganisms, their mutual adaptation occurred. As a result, a group of microorganisms was formed that constantly live on the external surfaces and internal organs of humans.
Each person, being surrounded by natural sources of microflora, communicating with other people and entering into various relationships with them, as a result of direct and indirect contacts “exchanges” microflora with them.
Microorganisms enter the human body with water, food, from various objects, and from the air. The composition of this “random” group depends not only on environmental factors, but also on the specifics of work, everyday life, individual physiology and metabolism of each person (oily or dry skin, sweating, etc.).
Appreciating with surprise the diversity and abundance of microbes in the environment, and primarily on his body, A. Leeuwenhoek noted that there are more of them in his own mouth than there are people in the entire United Kingdom.
In recent years, information has emerged that the microflora of the human body, with all its abundance and diversity, also has strictly individual characteristics for each individual. This individual specificity of microflora is so high that it can be compared with the specificity of fingerprints. This, in principle, makes it possible to identify a person’s personality based on the “prints” of a person’s microflora.
The microflora of the oral cavity is extremely diverse. Suitable temperature, alkaline reaction of saliva, leftover food are favorable conditions for the development of a wide variety of microorganisms. Almost all people in the oral cavity are inhabited by micrococci, streptococci, staphylococci, spore and non-spore bacilli, vibrios, spirochetes, spirilla, acidophilus, yeast, actinomycetes, etc.
Plaque and deposits in carious teeth and tonsil folds are especially rich in microbes.
In sick people and bacteria carriers, hemolytic streptococci, diphtheria bacillus, meningococci, tuberculosis bacillus, etc. can be found in the oral cavity.
The human respiratory organs do not have a permanent microflora. Its composition depends entirely on the content of microbes in the inhaled air. The microflora of the gastrointestinal tract, especially the large intestine, is very abundant. To illustrate, it can be stated that an adult person excretes many hundreds of billions of microorganisms from the intestines every day. The intestines are constantly inhabited by coli bacteria, some cocci, tetanus bacillus, bacillus perfringens, etc.
A lot of different microorganisms are on the hands, where they get from all other parts of the body and from the environment. The detection of typical inhabitants of the gastrointestinal tract, in particular E. coli, on the hands indicates an unsatisfactory sanitary and hygienic regime of work and life, and a low level of personal hygiene.
Cleanliness of hands, body, and maintenance of normal health are necessary for trade and catering workers who have constant contact with food products.
Oral cancer
Oral cancer most often affects the tongue, tonsils, gums and oropharynx. Since its various types often do not cause obvious signs and symptoms in the early stages, regular dental examinations are the most important method of detecting them.
Your dentist may also test you for oral cancer during your exam, especially if you have any of these symptoms:
- Persistent pain in the mouth or lip;
- Red or white spot in the mouth;
- Loose teeth;
- Painful swallowing, constant pain in the mouth or ears.
Treatment:
Depending on the type and stage of oral cancer, treatment may include a combination of surgery, radiation therapy and chemotherapy.
Dental clinic No. 2
The role of anaerobic bacteria in the occurrence of bad breath. 80% of problems associated with bad breath occur due to an excessively rapid growth of the number of bacteria in the mouth.
If you are young, healthy, and not susceptible to chronic sinusitis, tonsillitis or laryngitis, and suffer from bad breath, then most likely you have problems in the oral cavity.
When bad breath occurs due to oral disease, the substances you smell are sulfur compounds produced by anaerobic bacteria. Anaerobic bacteria live in the absence of oxygen, and they most easily colonize areas where there are cavities where oxygen is limited. The class of substances that anaerobes produce are called volatile sulfur compounds. Volatile sulfur compounds (VSCs) include substances such as hydrogen sulfide (the smell of rotten eggs), methyl mercaptan (the smell of rotten cabbage and a chemical added to natural gas to give it a distinctive smell), and ethane sulfide (the smell of decaying vegetables). There are more than 400 types of bacteria that live in the mouth. And only a few dozen of them, under favorable conditions, can cause an unpleasant odor. Such bacteria digest proteins such as dead tissue, blood and mucous membrane cells. Proteins are made from building blocks called amino acids, and the digestion of these amino acids provides bacteria with energy. Some of the amino acids contain sulfur, and these sulfur constituents are converted to VSC as a waste product.
A healthy mouth can harbor many different types of bacteria. In any part of the oral cavity, a kind of balance is established between competing species. If this balance is maintained, there will be no bad breath. A healthy balance of bacteria is called normal microflora, or “normal flora pattern.” There is a very wide range of floral specimens that are considered healthy. It's a little different for everyone. But when conditions in any area of the mouth change due to disease or other factors such as dehydration or the presence of fermentable substances such as blood, dead tissue or food debris, the balance of bacterial species changes, leading to an overgrowth of anaerobic bacteria over time. at the expense of the rest of the normal microorganisms. Thus, oral malodor occurs due to the production of VSC.
Prevention
Maintaining oral health is not difficult if you follow simple recommendations:
- Eat a balanced diet.
The diet should contain a sufficient amount of protein foods, as well as foods containing amino acids, trace elements and vitamins. Carbohydrate foods, on the contrary, are best consumed in small quantities.
- Careful oral hygiene.
It is important, for example, to use dental floss and brush your teeth with toothpaste or gel twice a day.
- Use of vitamins and nutritional supplements (as prescribed by a doctor).
This will make up for deficiencies in the body that affect oral health.
- Regular visits to the dentist.
You should visit your dentist for a checkup at least once a year. Even if there are no complaints.
Microbiota of the oral cavity and its connection with the occurrence of local and generalized infection
There is an opinion that the oral cavity is one of the dirtiest places in the entire human body. One can argue with this statement, but, according to scientists, saliva and oral fluid contain on average 109 microorganisms per 1 milliliter, and dental plaque contains 1011 per gram. According to the latest data, 688 species of different bacteria live in the mouth of a person who does not suffer from pathologies of the oral cavity [1].
Despite such a diversity of microbiota, with good hygiene and the absence of somatic diseases and mental disorders (such as diabetes, AIDS, constant stress and many others), we live in peace and harmony with the colonizers of the mucous membranes of our oral cavity. The presence of certain microorganisms in the oral cavity can serve as a diagnostic sign (for example, fungal diseases of the mucous membrane can be a sign of disorders of the T-cell immunity).
But, in addition to the mucous membranes, microorganisms also colonize the surface of the hard tissues of the tooth. As everyone knows, this leads to caries, and if you postpone a visit to the dentist and let the process take its course, it leads to complications such as pulpitis, periodontitis, and in the future to the formation of granulomas and cysts. Knowledge about the presence of certain representatives of the microcosm in the oral cavity, as well as about their physiological characteristics, allows us to find new ways to combat the pathologies that they can cause. The study of the oral microbiome has not lost its relevance today. Periodically, reports appear about the discovery of new representatives or the deciphering of the genomes of previously found bacteria. All this is necessary for a deeper understanding of the pathogenesis of diseases of the oral cavity, studying interbacterial interactions and improving the processes of treatment and recovery of patients, as well as the prevention of local and generalized complications.
As already mentioned, the human oral cavity normally contains a large number of different types of bacteria that do not live separately, but enter into various interactions, for example, forming biofilms. The entire microbiome of the oral cavity can be conditionally divided into two groups: permanent (species specific to a given biotope) and non-permanent microorganisms (immigrants from other host biotypes, for example, nasopharynx, intestines). A third type of microorganism may also be present—introduced microbiota from the environment.
Among the representatives of the normal microbiota, one can distinguish various types of actinomycetes (Actinomyces cardiffensis, A. dentalis, A. oris, A. odontolyticus, etc.), representatives of the genus Bacteroidetes (taxa 509, 505, 507, 511, etc.), Bifidobacterium (B. dentium, B. longum, B. breve, etc.), Campylobacter (C. gracilis, C. gingivalis, C. sputorum, etc.), Fusobacterium (F. periodonticum, F. gonidiaformans, F. hwasookii, etc.), Staphylococcus (S. warneri, S. epidermidis, etc.), Streptococcus (St. mutans, St. intermedius, St. lactarius, etc.) [1]. Despite its diversity, the species composition of the oral microbiota is quite constant, but the number of microbes of different species may fluctuate due to their species and changing environmental conditions. The quantitative composition of the microbiota can be influenced [2]:
- condition of the oral mucosa,
- physical conditions (temperature, pH, etc.),
- secretion of saliva and its composition,
- condition of hard dental tissues,
- food composition,
- hygienic condition of the oral cavity,
- absence of pathologies of the salivary glands, chewing and swallowing functions,
- natural resistance of the body.
Bacteria are retained on the surface of hard and soft tissues due to their morphological characteristics and certain intercellular interactions, which will be described below. Different types of bacteria have tropism for different tissues. For a further story about the formation of oral biofilms and the development of pathological processes, it is necessary to consider the main features of the predominant microorganisms.
This genus of bacteria is represented by immobile gram-positive cocci, located in “grape bunches” in the smear; are facultative anaerobes, chemoorganotrophs [5]. The most common representative of this genus in the oral cavity is Staphylococcus epidermidis, mainly located on the gums and in dental plaque. Breaks down food debris in the mouth and participates in the formation of dental plaque. Another common representative, Staphylococcus aureus, is the cause of the development of purulent bacterial infections, including generalized ones.
They are found in the oral cavity much more often than any other bacteria. Gram-positive spherical or ovoid cocci, chemoorganotrophs, facultative anaerobes [5]. Representatives of the genus that live in the oral cavity were identified as a separate group of oral streptococci. Like staphylococci, they break down food debris (mainly carbohydrates) to form hydrogen peroxide, as well as lactic acid, which plays a big role in the formation of dental plaque. Streptococcus mutans and S. sangius live mainly on the hard tissues of teeth and are found only after damage to the enamel, S. salivarius - mainly on the surface of the tongue.
Gram-negative anaerobic non-spore-forming cocci, chemoorganotrophs [5]. During their life activity, they decompose lactate, pyruvate and acetate into carbon dioxide and hydrogen, which increases the pH of the environment and has a positive effect on the formation of dental plaque (mainly Veillonella parvula) and the growth of other microorganisms. In addition, they are able to oxidize food debris to various organic acids, which promotes demineralization processes and the formation of microcavities.
Brief conclusions
- The most common oral diseases are tooth decay, gum disease, infectious diseases and oral cancer.
- Caries and gum disease are highly treatable in the early stages.
- The causes of infectious diseases of the oral cavity vary - from viruses to poor diet and uncontrolled use of medications.
- For prevention, it is important to review “life hygiene” and regularly visit the dentist.
Anti-Aging Medicine Seminars Gain knowledge based on evidence-based medicine first-hand from the world's leading experts. As part of the Anti-Age Expert Modular School, in-person two-day seminars are held every month, where the intricacies of anti-age medicine are revealed to doctors of more than 25 specialties
Find out more