Local anesthesia is used to numb sensations in a specific part of the body. This prevents pain during surgical procedures.
An anesthetic is applied to the part of the body that is undergoing surgery.
Can be used for sedation, which calms the patient and reduces stress levels. Together, they allow the surgeon to perform the procedure without pain or distress.
Local anesthesia does not last long, so it is mainly used for small outpatient procedures where the patient can leave the clinic the same day.
Benefit
Local anesthesia provides pain relief for dental surgery and other outpatient procedures.
Local anesthesia is used when:
- the operation is minor and does not require general or regional anesthesia
- the procedure can be performed quickly and the patient does not have to stay overnight
- the operation does not require muscle relaxation or loss of consciousness of the patient
Examples include dental surgery, removal of warts, moles or cataracts, and biopsy.
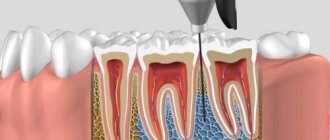
Stages of administration of infiltration application anesthesia
Infiltration anesthesia is used in the treatment of caries, pulpitis and other dental diseases, as well as tooth extraction (including complex ones) for prosthetics and removal of tumors of the oral mucosa. Regardless of the type of anesthesia, the algorithm for its implementation is as follows:
- Treating the injection area with an antiseptic;
- Exposing the transitional fold of the patient's oral cavity;
- Place the end of the needle on it at an angle of 45° relative to the alveolus;
- Inserting a needle into the bone to a depth of 5 to 15 mm;
- Carefully slowly introduce the solution.
The procedure is not performed if the patient has inflammation in the oral cavity or a malignant neoplasm.
Types of Local Anesthesia
The type and dose of anesthesia will depend on many factors. These include patients' age, weight, allergies, body part being operated on, and any current health conditions.
Various drugs are used to block pain. They can be applied by injection or by applying a spray or ointment.
The drug works by targeting specific nerve pathways to prevent the nerves in the area of application from sending signals to the brain.
Typically, the drug takes effect within a few minutes and wears off within a few hours. A stronger and higher dose will last longer.
Cocaine was the first anesthetic, but is now rarely used. Lidocaine is currently the most widely used local anesthetic, but different drugs are used for different purposes.
For longer procedures, bupivacaine is more suitable, but it may be more painful when first used. Therefore, the anesthesiologist may use lidocaine first and then administer bupivacaine if numbness is required for a longer period.
Synthetic anesthetics are similar in structure to cocaine, but these drugs do not have the same potential for abuse.
Principles of anesthesia in ophthalmology
Anesthesia in ophthalmology is used not only for pain relief; along with this, it solves several other problems and performs certain functions. Among them:
- Complete immobilization of the eyeball.
- Ensuring stable normal intraocular pressure.
- Blocking the flow of moisture to the eye through the tear ducts.
When choosing a method of pain relief in ophthalmology, the age of the patients must be taken into account. As a rule, these are elderly and elderly people who, in addition to eye diseases, also have some systemic diseases that require certain conditions.
Preparing for local anesthesia
If the patient is undergoing surgery with local anesthesia, the doctor should explain in advance how to prepare.
Patients should tell their doctor if they are using any medications, especially if they are blood thinning agents such as aspirin or warfarin.
Your doctor may instruct you not to eat anything for several hours before surgery. It is also important not to drink alcohol for 24 hours before taking the anesthetic.
In the doctor's office, the doctor applies a local anesthetic to the appropriate area of the body. It will start to feel numb.
The doctor will not act if the patient does not feel numb.
The anesthetic will prevent any pain, but the patient may still feel pressure during surgery.
Depending on what the procedure is and how anxious the patient feels, a sedative may be prescribed at the same time. This will help the patient feel calm and less anxious.
The doctor will monitor the amount of oxygen in your blood using a small device placed on your finger. In rare cases, a plastic nasal tube will be used to provide supplemental oxygen.
Regional anesthesia is a type of anesthesia that involves local interruption of pain impulses from the site of intervention by blocking the pathways. Regional anesthesia can act either as the main element of anesthesia, or as part of the so-called. combined anesthesia, that is, used as its component. The degree of participation of regional anesthesia in this case is different: it can act as the main analgesic component of the treatment, enhance the effect of systemic analgesia, or be used for postoperative pain relief.
Regional anesthesia is very attractive in a physiological sense, as it allows one to locally suppress pain impulses, preventing systemic effects of pain on the body and allowing one to either completely abandon the systemic effects of anesthetics or significantly reduce the degree of such effects. The use of regional anesthesia contributes to more effective treatment of postoperative pain syndrome, prevents the formation of chronic pain after surgery, has a beneficial effect on trophism and tissue regeneration, which ultimately accelerates the patient’s recovery and rehabilitation. Early activation of patients after regional anesthesia helps prevent thromboembolic complications in the postoperative period.
The following types of regional anesthesia are distinguished:
- Infiltration (terminal) anesthesia - blockade of pain impulses directly in the intervention area, most often performed by a surgeon;
- Conduction - blockade of nerve plexuses and individual nerves, which is carried out at a distance from the operation area;
- Neuraxial (central) blockades - spinal, epidural and caudal anesthesia, as well as their combinations.
Infiltration anesthesia is the simplest type of local anesthesia. It is performed directly by the operator by infiltrating the site of the intended intervention with an anesthetic solution. Infiltration may be limited to the skin and subcutaneous tissue, or may affect deeper layers. Its variety is terminal (topical) anesthesia, when an anesthetic is applied to the mucous membranes (ophthalmology, otorhinolaryngology, endoscopy, etc.).
Conduction anesthesia is a blockade of nerve plexuses, as well as individual nerves. It has become widespread during operations on the upper limb (blockade of the brachial plexus and individual nerves). The brachial plexus block has a high success rate, since when it is performed correctly, it is enough for the anesthetic to enter the fascial sheath of the plexus, the block is of sufficient quality and sufficient in duration. In contrast, nerve blocks of the lower extremity have not been as successful, as they have a lower success rate and are easily replaced by spinal or epidural anesthesia. Recently, nerve blocks of the anterior abdominal wall - TAP block and the like - have become widespread. Verification of plexuses or individual nerves during conduction blockades can be carried out in various ways: by paresthesia, using a neurostimulator or through ultrasound navigation. Verification by paresthesia is gradually becoming a thing of the past, since this method is accompanied by unpleasant sensations for the patient and a high risk of nerve damage. The classic technique remains verification using a neurostimulator, which gives a high block success rate, allows manipulation under sedation and is safer for the patient. Ultrasound navigation during regional blockades has been actively developing recently. It allows you to directly see nerve structures and reduce the amount of local anesthetic administered. Currently, most specialists recommend a combination of ultrasound navigation and the use of a neurostimulator to verify nerve structures.
Central (neuraxial) blocks are very common due to their effectiveness, the possibility of prolonged implementation and the relatively simple technique of implementation. Spinal anesthesia is widely used for interventions below the navel level, caesarean section, and for pain relief during childbirth. Epidural anesthesia is the gold standard for prolonged pain relief in labor and is widely used in postoperative analgesia, to stimulate intestinal motor function, and as part of multicomponent anesthetic treatments on the chest and abdominal organs. Caudal anesthesia is used in gynecological and urological practice. A significant advantage of epidural and caudal anesthesia is the possibility of prolonged anesthesia, when the installed catheter allows the patient to be administered local anesthetic for a long time.
Risks and complications
Local anesthesia is generally considered very safe. For minor surgeries it is safer than general anesthesia.
There may be tingling and pain, and there may be bruising as you take the drug and wear it off, but this is usually minor.
A person who has had local anesthesia must be careful not to get hurt when they cannot feel pain, such as when biting their cheek after dental treatment.
Temporary side effects that affect some people include:
- blurred vision, dizziness and vomiting
- headache
- muscle twitching
- persistent numbness, weakness, or tingling
Some people may have an allergic reaction. The patient may experience hives, itching, and difficulty breathing.
Cyanosis may occur, in which the skin turns bluish due to poor circulation or insufficient oxygenation of the blood.
In very severe cases, a person may experience CNS depression, in which the central nervous system slows down too much, resulting in a decrease in breathing and heart rate. This can lead to cardiac arrest if blood stops pumping to the heart.
An overdose of local anesthetic can lead to seizures. This can be life-threatening.
Application infiltration anesthesia: features and types
Infiltration anesthesia is a subtype of application anesthesia, which involves the introduction of an anesthetic drug into the soft gum tissues and, in fact, soaking them with it in order to innervate the area. Another name for it sounds like “freezing” - due to the numbness of the tongue, lips and cheeks that it provokes... In the process, the nerve impulse going from the pulp to the brain is stopped. In this case, the effect is achieved immediately after administration of the drug, and disappears as its components are broken down.
The procedure is quite safe due to the use of drugs with a minimum concentration of active substances. The solution is administered:
- Under the mucous membrane of the mouth;
- Directly under the skin;
- In the tissue around the bone (periosteum).
According to the method of administration, infiltration anesthesia is of two types:
- Direct - the solution is injected directly into the area to be manipulated;
- Indirect - the solution is injected into the area adjacent to the affected area so that it penetrates deep into the tissue.
Other applications
Local anesthesia may also be used to diagnose some chronic conditions and to relieve pain after surgery.
Research has shown that local anesthesia may be more useful than opioids such as morphine for treating pain after total knee replacement surgery.
In 2010, results from a rodent study in Turkey showed that local anesthetics may reduce some symptoms of inflammatory bowel disease (IBD).
Anyone administering any type of anesthetic should be appropriately trained and qualified.
Advantages and disadvantages of application infiltration anesthesia
As already mentioned, this type of pain relief is safe for the patient’s body due to the low concentration of active substances. Its other advantages are:
- Providing immediate effect;
- Rapid removal of substances from the body;
- Simplicity of the procedure technique;
- Minimal tissue trauma;
- Prolonged effect;
- Anesthetizing a group of nerves.
As for the disadvantages, they are as follows:
- Insufficiently good effect or its almost complete absence in diseases of the oral cavity of a purulent and inflammatory nature;
- The patient feels an unpleasant bitter taste of the solution after its administration;
- Insufficiently good effect on areas of dense bone formations;
- No effect for tissues that are deep.
How does an appointment with an anesthesiologist-resuscitator take place and why is it needed?
- The anesthesiologist examines the patient before the operation, and not only pays attention to the main disease for which the operation is to be performed, but also clarifies in detail the presence of concomitant diseases
- If the patient is operated on as planned, then, if necessary, treatment of concomitant diseases and sanitation of the oral cavity are carried out
- The doctor finds out the allergy history (whether all drugs and substances are tolerated by the patient)
- Clarifies whether the patient has undergone operations and anesthesia in the past
- Pays attention to the shape of the face, chest, neck structure, and the severity of subcutaneous fat tissue
- Such a detailed consultation is necessary in order to choose the right method of pain relief for each individual patient.
Examples of work “Before” and “After”
Complex one-stage implantation of the lower jaw
Case: there was a loose bridge of 4 front teeth on the lower jaw; after diagnosis, removal of the remaining teeth and complex basal implantation were prescribed.
Restoration of all teeth using basal implantation method (March 2012)
Case: partial adentia, exposed roots of natural teeth, periodontitis, increased tooth mobility, severe atrophy of bone tissue in some places beyond the possible norms for classical dental implantation.
Simultaneous implantation and removable prosthetics (June 2012)
Case: complete absence of teeth in the upper jaw; at the time of treatment, an old removable denture was used and was to be replaced.
Classical implantation and dental prosthetics (October 2012)
Case: need for implantation of a primary canine.
Deep sedation with Propofol - drug-induced sleep
Dental anesthesia for children
Dental treatment for young children under anesthesia raises the maximum number of questions among adults. The main ones relate to the safety of the procedure and side effects. Parents are also interested in what kind of anesthesia they give their children during dental treatment - whether there are high risks of negative consequences.
Is anesthesia harmful for dental treatment for children?
Sevoran is a non-narcotic, non-toxic, completely safe drug that is used in dentistry for treatment under general anesthesia. It is given to the child through a mask, instantly putting him to sleep.
Among the advantages of the drug, confirming its safety for young patients:
- excreted from the body unchanged;
- does not affect internal organs;
- does not depress the heart;
- maintains physiological blood pressure readings.
Sevoran simply turns off consciousness and does not cause side effects. Additional positive points:
- pain relief - doctors do not administer additional drugs to the child;
- pleasant smell - children themselves breathe through the mask with pleasure;
- quick recovery from anesthesia - awakening takes only 10-15 minutes.
The high quality of the composition ensures that the use of anesthesia for dental treatment for children eliminates any unpleasant consequences.
Anesthesia at the dentist for children: features
Having figured out whether it is possible to treat a child’s teeth under general anesthesia, parents begin to prepare the child for the procedure.
To do this, the young patient is prescribed a series of examinations:
- Consultation with a dentist.
The doctor must assess the amount of work - determine caries, pulpitis, and the intensity of tooth destruction. Together with the parents, a decision will be made on how many teeth to treat, what to remove, and whether prosthetics are necessary. - Testing, primary diagnostics.
The basic set of studies is general and biochemical blood tests, electrocardiogram (ECG).
- Obtaining permission from a pediatrician.
If there are chronic diagnoses, the child is also sent for a consultation with a specialized specialist in order to eliminate any risks during dental treatment.
When all issues are agreed upon, the doctor sets a date for treatment and gives final recommendations.
Soldatenkova Alina
When removing baby teeth, it is very important to preserve space for future permanent ones. To do this, they either undergo prosthetics or go to an appointment with an orthodontist to install an orthodontic seat holder.
Expert opinion
Emir Romanovich Omerelli
Maxillofacial surgeon, implantologist
Experience: more than 13 years
As can be seen from the above, pregnancy is a factor that excludes almost all types of anesthesia during treatment. Some experts believe that it is possible to use painkillers for dental treatment during pregnancy, but only if they do not contain adrenaline. And yet, before starting treatment with anesthesia, you need to decide whether it is really necessary in each specific case, and, if you cannot do without it, use local anesthetics. It is also worth assessing the level of necessity and appropriateness of the procedures, for example, teeth whitening is not necessary, and it is better to postpone it. There is no special anesthetic drug for pregnant women.
Currently, dentistry has a wide selection of drugs and anesthesia technologies. This allows treatment to be carried out with maximum comfort for the patient and the doctor. However, we should not forget about the risks of negative consequences, and make a decision about using anesthesia after carefully weighing all the pros and cons. Local anesthesia is by far the most preferred choice.
Other jobs
Deep sedation with Propofol - drug-induced sleep
During dental treatment, anesthesia for children or deep sedation may be used. These concepts are often confused, since in both cases the child is immersed in medicated sleep. But the difference is significant:
- General anesthesia in dentistry is given to children through a mask. Artificial sleep is as deep as possible, with complete loss of sensitivity.
- Sedation with Propofol involves intravenous administration of the drug and requires additional pain relief.
Propofol guarantees:
- natural physiological state of sleep;
- falling asleep in 1-2 minutes;
- exceptionally high safety for the child;
- simple awakening and rested state;
- extremely low risk of allergic reactions and side effects.
The quality and depth of sleep is controlled by an anesthesiologist. At this time, dentists treat and save teeth, remove completely destroyed units, and install prosthetic structures.
How to treat teeth without pain?
Today, all therapeutic and surgical procedures performed by a dentist with the risk of causing pain to the patient are carried out exclusively after the use of painkillers. Dentists use different types of anesthesia, which means reducing the sensitivity of the injection site to any external influences. The administered medication prevents the “pain impulse” from entering the brain, so the person “feels nothing.” Anesthesia in dentistry is necessary so that the patient avoids unpleasant sensations when a specialist performs treatment. When the patient is not in pain, he can remain at rest for a long time. These are optimal conditions under which the dentist can perform manipulations more efficiently and effectively.
Are there complications with anesthesia?
Complications during anesthesia may be related to the technique of administering anesthesia or the effect of anesthetic agents on vital organs.
- One of the complications is vomiting
- Breathing complications may be associated with airway obstruction
- Complications from the circulatory system - hypotension - a decrease in blood pressure both during the period of induction of anesthesia and during anesthesia - can occur due to the effect of narcotic substances on the activity of the heart or on the vascular-motor center; - heart rhythm disturbances (ventricular tachycardia, extrasystole, ventricular fibrillation); — cardiac arrest is the most dangerous complication during anesthesia