Causes
Let's look at the causes of dental cancer
:
- Oral injuries of various origins. Poor-quality dentures rub the gums; the presence of piercings in the tongue or lip can cause inflammation
- Bad habits (smoking, drinking alcohol and drugs).
- Untreated caries.
- Inflammatory diseases of soft tissues.
- Herpes virus, HPV, Bowen's disease.
- Poor oral hygiene.
- Hot or spicy foods that constantly irritate the mucous membranes.
- Work in conditions harmful to health (hot workshop, dusty room).
- A history of cancer of the stomach, kidneys and lungs. In this case dental cancer
is a secondary pathology.
To take care of your health, rule out dental cancer, causes
its development must be monitored. Careful oral care, eradication of bad habits, and regular visits to the dentist will reduce the risk of developing pathology.
Oral care for children
Children should follow the recommendations in this material. They should also adhere to the recommendations below.
- Use fluoride toothpaste. If your child is 2 years old or younger, consult your dentist or doctor before using fluoride toothpaste.
- If your child's teeth have not yet grown, use a terry cloth, wet wipe, or sponge to clean the gums after meals and before bed.
- If a child has a stable immune system, he should be taken to the dentist every 6 months for routine monitoring.
- Contact Child Life Services to learn how to help your child cope with pain. You can contact them at 833-675-5437 (833-MSK-KIDS).
to come back to the beginning
Stages of pathology development
Dental cancer
Like any cancer, it occurs in the human body through four stages:
- The first stage is when the tumor is within 10 mm. The place of formation is the mucous membrane or tooth germ.
- The second stage is when the tumor reaches 3 cm. The symptoms of cancer become more obvious. Metastasis is found in one of the regional lymph nodes.
- Stage three – the tumor exceeds 3 cm in size. Metastases are detected in several regional lymph nodes.
- The fourth stage is when the process becomes aggressively malignant, affecting the oral cavity, nose, and also the base of the skull. Metastases may be found in the lungs and liver.
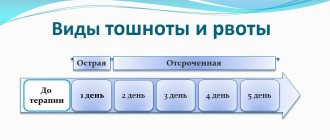
When is chemotherapy indicated?
The decision on drug treatment of oncology is made by the attending physician, based on the results of tests and hardware studies. As a rule, chemotherapy is used in the following cases:
- Type of cancer. The choice of surgical or conservative treatment depends on the type of malignant tumor, its size and stage of development. Chemotherapy is always given after surgery to destroy remaining cancer cells and possible metastases.
- Features of the patient's body. If a cancer patient is elderly and most likely will not survive the operation, or for other reasons (the tumor is localized in a place inaccessible to surgery, poor general condition, chronic diseases), he is prescribed chemotherapy as treatment. In this case, the emphasis is on inhibiting the growth of cancer cells and increasing the life expectancy of a person with cancer.
Most often, drug therapy for oncology is prescribed to prevent metastasis of previously removed tumors, as well as to treat blood cancer (leukemia, hemoblastosis) and other rare types of malignant neoplasms (choriocarcinoma, rhabdomyosarcoma). Chemotherapy is also used to prepare the tumor for surgery so that the surgeon can completely remove it without leaving a single cancer cell.
Symptoms of tooth cancer
Oncology in the initial stages has hidden symptoms and can develop over years and decades. Gradually the symptoms begin to manifest themselves:
- A formation of soft consistency to the touch appears on the jaw, convex in shape, increasing in size over time.
- The dentition may become deformed and the teeth become mobile.
- Pain sensations increase. It becomes difficult for a person to eat, chew, and swallow.
- Regional lymph nodes increase in size.
- A man loses weight.
- Low-grade body temperature, which periodically rises.
- Fistulas in tissues.
- When pressing on the tumor area, the doctor may feel a crunching sound.
- The enamel becomes fragile and is destroyed very easily.
In the prevention of dental cancer symptoms
may not appear, but it is important to visit your doctor regularly. Identified disease in the early stages provides a better prognosis for treatment. Late stages are dangerous for metastasis to other organs.
Anemia during chemotherapy
Oxygen is delivered to the tissues of the body by red blood cells - erythrocytes. Each of them lives only 3-4 months, so new ones must constantly form in the red bone marrow. Chemotherapy drugs attack red bone marrow cells, the content of red blood cells and hemoglobin in the blood decreases, and anemia develops.
Manifestations of anemia:
- weakness;
- dizziness;
- shortness of breath, feeling of lack of air;
- cardiopalmus.
Tell your doctor if you begin to experience these symptoms. Anemia requires immediate treatment. There are drugs that increase the activity of red bone marrow. In severe cases, red blood cell transfusion is indicated.
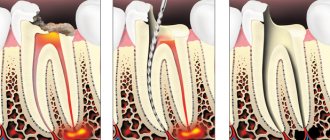
Treatment of tooth cancer
When the doctor confirms dental cancer, symptoms
which prompted you to come to the appointment, it is necessary to begin treatment as soon as possible. The most effective method is surgical removal of the tumor within healthy tissue. In the early stages of the process, the tumor is removed along with the teeth and part of the jaw.
In other cases, the jaw is resected completely or partially, and regional lymph nodes are removed. Based on the results of diagnosing the type of tumor and the stage of the process, chemotherapy or laser therapy is prescribed before surgery in order to reduce the tumor in size.
In the first and second stages, the prognosis is favorable: 80% of people survive the 5-year mark. In the third stage of the disease, more than half of people survive five years. In the fourth stage, only 15% reach the five-year survival mark. Regular preventive examinations and adherence to healthy lifestyle standards can reduce the risk of disease.
Dental treatment for oncology
Dental treatment for cancer is associated with difficulties. During chemotherapy and radiation therapy, the body suffers from various side effects. Dental treatment becomes additional stress for a person. The gold standard before starting cancer therapy is oral hygiene, as the body will be less able to resist bacteria during cancer treatment.
How to preserve eggs and sperm
First of all, you need to consult a fertility specialist. Then the patient receives a referral for a spermogram and a test that shows how sperm tolerate freezing.
After receiving the results, the man donates blood for HIV, hepatitis and syphilis and, if the results are negative, donates seminal fluid. Semen storage costs from 3,500 rubles per year, depending on the sperm bank. It is better to contact specialized reprobanks rather than IVF clinics. Reprobank has better conditions for storing frozen biomaterial and much better prices.
Donating eggs is much more difficult. A woman will have to undergo a course of hormonal stimulation to get not one egg, but ten. The eggs are then collected from the ovary by inserting a thin needle through the vagina under general anesthesia. In some cases, hormonal stimulation is contraindicated, so consultation and permission from an oncologist is necessary.
A special method, vitrification, allows you to save eggs. This is ultra-fast freezing, in which the solution in which the object is located does not crystallize, but turns into a glass-like state. This explains the name - from Latin “vitrum” is translated as glass.
Vitrification does not damage eggs and allows you to preserve 99% of them indefinitely. There are cases where eggs were used for fertilization thirteen years after freezing.
Treatment and removal of teeth in cancer patients
In cancer patients, during the treatment of the underlying disease, favorable conditions are created in the oral cavity for the proliferation of pathological microorganisms. Irradiation inhibits cell growth, including in the oral cavity.
The task of a dentist in the treatment of teeth and oncology
the patient is not to harm him. Despite the fact that the body is weakened by a serious illness and no less severe therapy, caries must be treated so that it does not turn into pulpitis. Due to weakened immunity in cancer patients, inflammation progresses rapidly if left untreated. When treating teeth, it is important that the doctor knows the number of leukocytes, blood coagulation status, uses low-traumatic techniques, and coordinates the procedure with the oncologist.
Consequences of chemotherapy for men
Chemotherapy drugs affect the male gonads, reduce the number of sperm and impair their motility. In addition, the drugs affect the hereditary material of the cell, causing changes in the DNA structure and mutations. Drugs such as cyclophosphamide and cisplatin are especially dangerous.
A course of chemotherapy causes temporary infertility in ninety percent of men. In sixty percent of them, reproductive function is not restored. And with each course, the quality of sperm will deteriorate even more, so men should think about cryopreservation of seminal fluid in advance. Then, after being cured of cancer, the patient will have the opportunity to have children.
Frozen sperm can be used at any time; it is stored for at least twenty years, and children born from it are no different from those conceived naturally.
Another problem for a man with cancer is that his body is severely depleted by the effects of the tumor and chemotherapy drugs. Often there is a decrease in libido and erectile dysfunction, but most often this problem is purely psychological. The support of a caring “other half” will help overcome this problem, especially since after completing the course, erection and libido are restored.
However, it is worth remembering that during the course a man must use condoms, even if his sexual partner uses other methods of contraception. This is due to the fact that chemotherapy drugs are even contained in a man’s seminal fluid. In addition, during the course there is a very high probability of conceiving a child with deformities.
Chemotherapy and tooth extraction
Teeth that cannot be restored are subject to removal. Although patients receiving chemotherapy have a weakened immune system, the consequences of refusing to remove an inflammatory tooth are much more serious than the side effects of anticancer therapy. It is advisable to remove teeth before starting chemotherapy.
in dental treatment
is taken into account, the doctor takes into account the patient’s condition when choosing an intervention technique. Treatment by a dentist during chemotherapy is not advisable, but if there is an emergency and the patient is already taking chemotherapy, the intervention of a doctor will avoid big problems. Removal should be done as atraumatically as possible.
Dental problems and dental treatment for oncology
After chemotherapy, many are faced with the fact that they develop caries, gingivitis, stomatitis, periodontal disease, cysts begin to form, gums become more sensitive and bleed.
This condition creates additional difficulties for the dentist, but does not mean that you need to refuse dental treatment, cancer
not prevent. It is important to tell your dentist about your diagnosis and that you are currently undergoing treatment for cancer. This will allow him to choose the most gentle methods for solving dental problems.
You need to know that when treating teeth, oncology
does not progress and the disease itself is not a contraindication to dental intervention. Dental treatment will remove the source of infection, prevent its further spread, and defeat cancer.
Dental treatment of patients during chemotherapy and radiotherapy: review of clinical approaches
Rai Balwant, doctor, professor (USA)
It was previously reported that the cumulative effect of acute and chronic forms of oral lesions as a result of chemotherapy and radiotherapy provokes the development of complicated dental pathologies. This article reviews aspects of the dental treatment of cancer patients before, during and after appropriate anticancer therapy.
Cancer is one of the most difficult diseases to treat, as it is characterized by uncontrolled tissue growth and an imbalance between cell division and apoptosis. Most side effects of chemotherapy and radiotherapy can be caused by toxic effects on a specific organ or disruption of the division of normal cells in the structure of the affected organ.
The following are the side effects of chemotherapy agents used to treat cancer.
- Bone marrow suppression:
- leukopenia;
- thrombocytopenia;
- anemia;
- increased susceptibility to infections;
- increased incidence of secondary malignant lesions;
- Lesions of the gastrointestinal tract:
- nausea;
- vomit;
- diarrhea;
- mucositis;
- Skin lesions:
- erythema;
- maculopapular rash;
- exfoliative dermatitis;
- alopecia;
- hyperpigmentation;
- photosensitivity;
- Irreversible cardiomyopathy.
- Toxic lung damage.
- Hepatotoxic effect.
- Toxic kidney damage.
- Neurotoxic effects such as pain, peripheral neuropathy, seizures.
- Suppression of spermatogenesis, oogenesis and the menstrual cycle.
- Oral lesions:
- mucositis;
- infectious lesions (bacterial, viral, fungal);
- bleeding;
- xerostomia.
Prevention and therapeutic treatment before starting antitumor therapy
Before starting any manipulations aimed at treating cancer, a preliminary diagnosis of the condition of the oral cavity is recommended in order to:
- prevent further development of diseases that may worsen during cancer therapy;
- obtain data on the initial state of the oral cavity, which will later be used in monitoring and analyzing the effect of radio- and chemotherapy;
- identify metastases in a timely manner;
- minimize the level of discomfort in the patient’s oral cavity during antitumor therapy.
All patients with neoplastic lesions receiving chemotherapy should undergo a thorough dental evaluation, which includes a clinical examination and radiographic examination. Before starting chemotherapy, the patient should be instructed and properly motivated to practice oral hygiene.
In the case of chemotherapy for the head and neck area, the following recommendations must be taken into account:
- periodontally or structurally compromised teeth must be removed;
- teeth associated with maxillofacial abscesses also need to be removed or treated through endodontic intervention;
- all surgical procedures must be completed at least 10-12 days before the onset of neutropenia;
- it is advisable to fully carry out the necessary dental treatment aimed at restoring teeth affected by caries or pathological abrasion, replacing defective restorations, removing poorly fixed orthopedic structures and orthodontic arches;
- existing dentures should be thoroughly cleaned and treated daily with nystatin to prevent the development of fungal infections;
- In children, it is necessary to remove mobile primary teeth, as well as those teeth that probably cannot be saved after chemotherapy and radiotherapy, taking into account the time required for healing of the sockets before starting antitumor therapy.
Recommendations for tooth extraction in patients planning to undergo radiotherapy or chemotherapy
- The extraction procedure should be minimally invasive and performed 2, or better yet, 3 weeks before the start of radiotherapy.
- In the upper jaw, tooth extraction should be carried out at least 5 days before the start of chemotherapy. On the lower jaw - no less than 7 days.
To avoid injury to the oral mucosa, the sharp edges of the socket should be smoothed immediately after extraction.
It is necessary to ensure primary closure of the wound.
You should avoid introducing hemostatic drugs into the socket, since in the future they can become a source of infection.
If the platelet count is less than 50,000 units/mm3, a blood transfusion is required.
Extraction should be delayed if the platelet count in the blood is less than 2000 units/mm3 or the neutrophil count is less than 1000 units/mm3. As an alternative approach, tooth extraction can be performed with the mandatory prescription of antibiotics.
Patients who want to save their own teeth should be informed about the possible development of hyposalivation, an increased risk of developing infectious lesions such as caries or osteonecrosis, associated specifically with the effect of chemotherapy and radiotherapy.
Oral care during chemotherapy
From the very beginning of chemotherapy, special attention should be paid to proper oral hygiene in order to minimize the risk of developing possible complications. To date, there are no generally accepted protocols for the prevention and treatment of chemotherapy-induced mucositis.
Rinsing the mouth with physiological or bicarbonate solutions helps relieve symptoms of mucositis, remove plaque, and dilute acids and toxins in the oral environment. Some commercially available rinses, such as hydrogen peroxide, may adversely affect the oral cavity in the presence of mucositis and should be discontinued in patients.
Given the increased likelihood of oral infection during chemotherapy and increased bleeding of soft tissues, patients are advised to brush their teeth 2-3 times a day.
Patients who undergo total body irradiation or chemotherapy are also likely to develop thrombocytopenia. Bleeding of the oral mucosa usually develops when the platelet count is less than 5000 units/mm3. Local agents, such as a gelatin sponge with thrombin or microfibrillar collagen, or antifibrinolytic agents in a soft mouth guard can be used to control bleeding. If such interventions do not produce the desired effect, platelet transfusions should be considered.
The dental surgeon must be aware of the number of leukocytes and platelets in the blood of a patient undergoing chemotherapy or radiotherapy before starting treatment. If the platelet count is above 50,000 units/mm3, the patient can undergo most routine dental procedures, however, if the platelet count is below this figure, it is imperative to consult an oncologist. If invasive dental procedures are necessary, blood or platelet concentrate transfusions should be considered. If the platelet count is less than 2000 units/mm3, it is recommended to prescribe antibiotic prophylaxis and consult with your doctor.
In addition, patients should be advised to:
- Drink plenty of water and other liquids other than coffee and tea.
- During and after radiotherapy, teeth may become hypersensitive, which may be due to a decrease in salivary secretion and a decrease in its pH. Topical application of fluoride gel can relieve symptoms of hypersensitivity.
- Radiotherapy to the head and neck area can cause damage to muscle vessels and cause trismus of the masticatory muscles and joint capsule. To minimize the effect of radiation on the muscles of the maxillofacial area, special protective mouth guards must be used during external irradiation. The patient should also perform muscle stretching exercises at least 3 to 4 times a day.
- Patients should avoid using prostheses for the first 6 months after completion of radiation therapy.
- The installation of dental implants can be carried out one and a half years after radiation therapy, taking into account the condition of the oral tissues, the level of their vascularization and the possible prognosis of healing.
Prevention is the best treatment for soft tissue bleeding in the oral cavity. When the platelet count is low (eg, <20,000 units/mm3), even routine tooth brushing can cause bleeding. Oral hygiene in such cases should be carried out with a disposable sterile sponge under slight pressure or a cotton swab, followed by rinsing with a solution of chlorhexidine 0.6% or povidone-iodine.
Antiemetics may be used to reduce or prevent symptoms of nausea and vomiting. The use of high-calorie and high-protein supplements often helps maintain adequate quality nutrition for the patient during cancer therapy.
Caring for Patients After Chemotherapy
The period after chemotherapy is most suitable for most dental procedures. Oral care should include daily brushing of teeth with soft brushes. Oral rinsing with saline or bicarbonate solutions, lubricants and topical anesthesia, and chlorhexidine rinses should be continued to prevent the development of infectious lesions and relieve residual symptoms of xerostomia. Fluoride administration and dietary counseling are also useful in a program to prevent xerostomia-induced caries.
Patients should be monitored after anticancer therapy for several reasons:
- a patient with cancer pathology is at risk of developing additional lesions;
- the likelihood of developing hidden metastases;
- the likelihood of recurrence of primary lesions;
- the risk of complications associated with therapy.
Treatment of mucositis can be carried out by the patient following the following recommendations:
- Moderate mouth rinses (salt + soda solution).
- Local anesthetics (lidocaine 5%) and antihistamine solutions (benzydamine chloride).
- Antimicrobial rinses, such as chlorhexidine rinses.
- The use of anti-inflammatory drugs: Kamilosan liquid (aqueous-alcoholic chamomile extract) or topical steroids (dexamethasone).
- Adequate hydration of the oral cavity.
- Use of oral lubricants.
- Air humidification.
If a patient has developed some form of immunosuppression after chemotherapy, and the white blood cell count is less than 2000 units/mm3, the immune system is not able to overcome most infections on its own. In addition, patients after chemotherapy or radiotherapy often experience a decrease in salivation and the development of opportunistic infections. For candidiasis of the mucous membrane, antifungal drugs (such as nystatin) should be used.
Osteoradionecrosis after radiation therapy
Osteoradionecrosis is a pathological condition characterized by exposure of bone tissue, areas of which are unable to regenerate after a significant dose of radiation. Protocols to reduce the risk of developing osteoradionecrosis include adequate choice of endodontic treatment instead of tooth extraction, use of non-lidocaine local anesthetics without or with very low concentrations of epinephrine, prophylactic antibiotics, as well as their use after surgery for two weeks, use of hyperbaric oxygenation before starting invasive procedures.
In the early stages of necrosis, conservative treatment is indicated. The exposed bone can be irrigated with saline or an antibiotic solution, and patients should be instructed to irrigate the affected area. When a bone sequester forms, it should be removed immediately to ensure the epithelization process.
Translation: Miroslav Goncharuk-Khomin, Yulia Devyatko
Urinary dysfunction during chemotherapy
Chemotherapy may change the color and smell of your urine. Ask your doctor what changes may occur. If some symptoms appear, you must inform your doctor about them:
- Chills, fever over 38°C.
- The urine turned red, orange, dark yellow, green, cloudy, and there was blood in it.
- Urination has become difficult, during which there is a burning sensation and pain.
- The urine began to smell sharp.
Some recommendations will help you:
- Drink enough liquid - at least 8 glasses daily. This can be water, juices (it is better to dilute them with water), fruit drinks, milkshakes, compotes, soups.
- Drink more water, even if you urinate a lot and often, this will help normalize your body's functioning.
- Avoid any drinks that contain alcohol or caffeine.
What should you ask your doctor?
- How much fluid should I drink daily?
- What drinks are best to drink?
- What drinks are undesirable?
- What drinks should you not take?
- In what cases should you urgently consult a doctor?
Swelling during chemotherapy
The occurrence of edema can be provoked by chemotherapy drugs, hormonal changes in the body, and general health (in particular, the cardiovascular system). Call your doctor immediately if you experience the following symptoms:
- Difficulty breathing.
- Feeling that the heart is not working properly.
- Rapidly, sharply occurring swelling that quickly increases.
- Unexplained weight gain - This may also be due to swelling.
- Very rare urination, a small amount of urine - this indicates that fluid is retained in the body.
Some recommendations will help improve your condition:
- Wear loose shoes.
- Try not to stand for long periods of time.
- When lying or sitting, try to raise your legs so that they are no lower than the level of your heart.
- Weigh yourself at the same time every day, keep a diary and record your results every day.
- Avoid adding salt and soy sauce to your food.
- Avoid foods that contain a lot of salt: ham, chips, sauerkraut, pickles.
- When you buy foods, be sure to read labels and check how much salt they contain.
What should you ask your doctor?
- How much salt can I consume per day?
- Should I wear compression garments?
- What kind of weight gain should you pay attention to?
- What foods should you not eat?
- How can you reduce swelling and improve the condition?
Read more about swelling due to cancer in a separate article.
Goals and evaluation of the effectiveness of drug treatment
There are three types of drug therapy: preoperative (neoadjuvant), prophylactic (adjuvant) and palliative (maintenance).
— How is treatment carried out in each case?
— Let's start with preoperative drug therapy. For example, a patient is admitted to the department with a diagnosis of stomach cancer. CT results show that there are no distant metastatic foci, however, due to the spread of the primary tumor, surgery at the first stage is impossible. In this case, treatment looks like this: four courses of therapy, then surgery, and after that another four courses of adjuvant therapy. Why else? Formally, the tumor was removed, but there is a risk of the tumor returning, and adjuvant therapy helps to delay it.
The doctor chooses palliative therapy when surgical methods are powerless (for example, with distant metastases to the lungs, liver, lymph nodes, etc.). Treatment is then primarily aimed at maintaining the patient's quality of life and controlling the disease, and the duration of treatment depends on its effect. In chemotherapy, doctors use RECIST 1.1, a system of criteria for assessing tumor response to therapy, and in immunotherapy, irRECIST.
“I’ll explain how this works, using the example of a patient with a colon tumor and multiple metastases in the liver and lungs. To assess the severity of the situation, we conduct an examination, identify the most measurable lesions and administer two to three cycles of chemotherapy. Most chemotherapy courses involve drug administration. There are 14-21 days between the first injection and the second, and this time period is called a cycle.
Next we look and compare. If the tumor has decreased by more than 30%, this is a partial response, and therapy should be continued for up to six courses. If she leaves, this is a complete regression, and we also add four courses to consolidate the result. If the tumor has increased or decreased by 20%, this means stabilization, we do two more courses and look again: if the situation has not changed, the patient goes on a chemotherapy holiday until the disease progresses, and then the regimen is repeated.
But if the tumor has grown by more than 20% during treatment, we are dealing with progression; most likely, this tells us about the aggressiveness of the tumor. In this case, I explain to the patient what is happening to him and why we are changing treatment.
— How to persuade a patient to undergo treatment?
— Everyone needs an individual approach. I always say: “Chemotherapy may worsen your condition, but you should not be afraid of this - we will try to select the optimal symptomatic therapy that will reduce adverse events.” If after this, during treatment, evidence of poor tolerability appears, we will think about reducing the dose of the cytostatic. There are times when I literally talk a patient into going to therapy and explain to him what we are fighting for. And I explain this regardless of the seriousness of the case - if with an aggressive tumor a person is determined to fight to the last, it is my duty to give him this opportunity.
Interviewed by Daria Semeina
What to do if there is bleeding during chemotherapy treatment?
By attacking bone marrow cells, chemotherapy can reduce the number of platelets in the blood, the cells that are responsible for blood clotting. If chemotherapy drugs affect blood clotting, bruises on the body, frequent nosebleeds, and a small rash on the body may occur.
What to do if there is a risk of bleeding?
- handle cutting objects carefully;
- avoid too vigorous activity, in which there is a risk of bruises and cuts;
- use an electric razor instead of a razor;
- use a soft toothbrush and avoid dental floss;
- Avoid constipation.
When to see a doctor?
Tell your doctor if you are concerned about the following symptoms:
- There was no stool for more than 2 days.
- I'm worried about pain in my stomach.
- The belly has increased in size.
- Appetite has decreased, nausea and vomiting occur periodically.
How to deal with constipation?
These simple tips help many people:
- Drink enough liquid - at least 8 glasses a day. Plain water, compote, juices from fruits and vegetables, tea, coffee will do. Water will help soften the stool and make it easier to pass.
- Eat more foods rich in fiber : seeds, nuts, vegetables, fruits, whole grain bread.
- Move more. Physical activity helps strengthen intestinal motility. Walk or bike for 15-30 minutes every day. Ask your doctor what exercises may be appropriate for you.
What to ask your doctor?
- What medications will help relieve constipation?
- What's better to eat and drink?
- How much fluid should you drink daily?
- What physical exercises can you do?
- When do you need to see a doctor urgently?
Infection during chemotherapy
Tell us immediately if you:
- Temperature 38⁰ C or higher. Ask your doctor how to take your temperature.
- You have chills.
- Cough or sore throat.
- Ear pain.
- Headache and pain in the maxillary and frontal sinuses.
- Pain or stiffness in the neck muscles.
- Skin rash.
- Ulcers, white coating on the tongue or inner cheeks.
- Redness or swelling anywhere. This is especially important if you have a catheter.
- Blood in the urine or cloudy urine.
- Pain or burning when urinating.
If you feel unwell or have symptoms that weren't there before, don't wait. Call your doctor immediately.
Follow these tips to reduce your chance of infection:
Always wash your hands:
- Before preparing and eating food,
- After the toilet,
- After being in public places. Wash your hands with warm water and soap.
- Ask your loved ones to wash their hands thoroughly as well.
- Consult your doctor about using hand sanitizer.
Follow the rules of hygiene:
- Brush your teeth after eating and before going to bed. Use a very soft toothbrush.
- If you have a catheter, try to keep the area dry and clean. Ask your nurse how to care for this area.
Try to avoid injury:
- Use an electric razor, not a regular razor.
- Wash yourself thoroughly and carefully after using the toilet. Tell your doctor if your rectal area hurts or bleeds.
- Do not touch or squeeze pimples.
Avoid contact with germs:
- Stay away from people who are contagious, especially those with a cold or flu. Avoid large crowds of people.
- Wash raw fruits and vegetables thoroughly.
- Wash your hands thoroughly after handling raw meat. Fry the meat thoroughly.
- Try to avoid people who have recently been vaccinated against measles, chickenpox, or polio.
- Have someone clean up after your pets.
Questions to ask your doctor:
1. In what cases should I call a doctor? 2. What else can I do to avoid infection? 3. How often should the temperature be measured? 4. In what cases should you call an ambulance?
Nervous system during chemotherapy
Chemotherapy can cause some nervous system side effects. If you notice them, you should immediately tell your doctor:
- Pain while walking.
- Rapid fatigue of the arms and legs, tingling, burning, numbness.
- Loss of balance, falling.
- Dizziness.
- Muscle spasms, cramps, pain.
- Deterioration in hand function: it has become more difficult to lift and hold objects.
- Hearing loss.
- Stomach ache.
- Constipation.
Helpful tips for people with neurological disorders:
- Remove or move carpets in your home to avoid tripping hazards.
- Screw on special grab bars in the bathroom.
- Place a non-slip mat in the bathroom.
- Wear comfortable shoes without high soles.
- Use a cane.
- Buy comfortable shoes for indoors.
- Wear rubber gloves when working in the kitchen or cleaning.
- Regularly examine your feet with a mirror, ask your loved ones for help.
- An ice pack will help reduce pain and discomfort.
- When doing chores around the house, take your time and don't overexert yourself.
- If you find it difficult to do some things, do not hesitate to ask your loved ones for help.
What should you ask your doctor?
- What medications can help treat neurological disorders?
- Should I see a chiropractor?
- What neurological problems might I have and when is it most likely to happen?
- How long will these side effects last?
- In what cases should you consult a doctor?
Changes in appetite during chemotherapy
Typically, chemotherapy causes two types of changes in appetite:
- Decreased appetite, up to complete absence.
- Changing the taste of foods.
It is important for cancer patients to continue to eat and drink enough fluids. Some tips will help with this:
- Train yourself to always eat at approximately the same time . Even if you are not hungry, take some food.
- Often 5-6 small meals throughout the day are better than 3 large ones.
- Try new dishes. If you don't feel like eating, eat socially with family and friends while watching TV.
- Seasonings can improve the taste of food . Ask your doctor which ones may be appropriate for you.
- Sometimes patients feel a metallic taste in the mouth. In this case, you can replace the spoon and fork with plastic ones.
- Food should be high in calories and rich in protein.
- Move more. Physical activity will help increase your appetite.
- Eat liquid foods (broths, cocktails) that are easy to swallow.
- Don't drink while eating.
- Keep a food diary , write down everything you eat, and note the time. This will help you and your doctor monitor how well you are eating.
High-calorie foods recommended during chemotherapy:
- Soups : bean, lentil, cream soups.
- Drinks : whole milk, fruit smoothies, milkshakes, drinking yoghurts.
- Snacks : beans (black and red), chicken, fish, eggs, grains, nuts, wheat germ.
- Desserts : muffins, ice cream, custard, yoghurt, puddings.
- Other products : margarine, sunflower and butter, soft cheese, sour cream, cottage cheese, milk powder, liquid meal replacements.
If you are losing weight, be sure to tell your doctor about it!
What to ask your doctor?
- What foods can you eat?
- Should I take vitamin complexes and protein shakes?
- How much fluid should you drink every day?
- What physical exercises can you do to increase your appetite?
- How to properly keep a food diary, what to write down there?
- In what cases do you need to urgently contact a doctor?
What to do in case of memory and attention problems?
Taking chemotherapy drugs causes disruption of the nervous system and memory problems. If you experience dizziness, loss of balance, spasms and pain, or deterioration of the musculoskeletal system, tell your doctor about these conditions.
During chemotherapy, memory may be impaired and thinking may be inhibited. Sometimes, a condition called “chemo-brain” occurs, a disorder of cognitive processes associated with taking drugs that suppress cancer cells. If you experience problems with attention, memory, or confusion, talk to your doctor about overcoming these unpleasant symptoms.
What to do?
- get more rest;
- make a to-do plan and act on the list;
- ask your loved ones for help;
- create reminders in the form of notes or using an application on your phone;
- divide big things into small and specific tasks.
The effect of chemotherapy on male fertility
Some chemotherapy drugs cause a decrease in testosterone levels in the body in men. This leads to some symptoms:
- Erectile dysfunction: difficulty getting and maintaining an erection.
- Decreased sexual desire.
- Increased fatigue.
- Irritability, tendency to depression.
- Sometimes - hot flashes, sweating.
Some medications help combat these disorders.
When a man is undergoing chemotherapy, he must use a condom during sexual intercourse, even if his partner uses other forms of contraception. Chemotherapy drugs can penetrate sperm and enter the woman’s body with it.
The effect of chemotherapy on female fertility
Chemotherapy can lead to decreased levels of female sex hormones and premature menopause. Symptoms such as:
- Dryness, itching in the vagina, pain and discomfort during sexual intercourse.
- Hot flashes.
- Decreased sexual desire.
- Weakness, emotional instability, tendency to depression.
- Irregular periods or absence of them.
- Sweating at night.
Hormonal therapy, relaxation techniques, and artificial vaginal lubricants help to cope with these manifestations. If hot flashes are a concern, carry a fan with you. Wear light clothing under warm clothes so that they can be removed during high tide.
During chemotherapy, you need to use contraception because chemotherapy drugs damage the cells of the embryo and fetus. If you are planning to have a child in the future, you need to inform your oncologist in advance and consult with a reproductive health specialist.