The number of cancer diseases is steadily growing throughout the world every year, and the proportion of patients with malignant neoplasms can reach 1.4% of the country's population [1]. According to experts from the World Health Organization, in the next twenty years the number of cases of various types of cancer in the world will increase by 60% [2]. Today in Russia there are about 3.7 million people living with some kind of cancer, which is approximately 2.6 thousand cases per 100 thousand population [3].
Currently, an important indicator of the effectiveness of cancer treatment is improving the quality of life of patients. One of its components is timely dental care aimed at maintaining health and preventing oral diseases.
How cancer affects oral health
Oncology develops under the influence of both external and hereditary genetic factors. This pathology can affect any part of the body and does not depend on the age of the patient. It begins with changes in just one cell and leads to serious, often fatal consequences for human health and life.
With the development of cancer, the functions of the affected organs may be impaired. In addition, these pathologies lead to a general deterioration of the condition, decreased immunity, bad mood, depression, digestive dysfunction and anemia. Thus, malignant tumors have a complex effect on all systems and organs of the body, including the condition of the oral cavity.
Types of nausea and vomiting
The type of nausea and vomiting is determined by the time it occurs during the chemotherapy cycle:
acute - on the first day after the administration of cytostatics
delayed - within 2-5 days after the administration of cytostatics.
With subsequent administrations of the drug, “premature vomiting” (nausea and vomiting “waiting”) may occur - within several hours before the administration of cytostatics. It usually develops in patients who previously received highly emetogenic PCT regimens and suffered from its complications. It can be provoked by smells, tastes, the sight of objects and surroundings reminiscent of treatment. To prevent such nausea and vomiting, tranquilizers, psychotraining, and hypnosis are used.
Unfortunately, often patients may not report the development of complications. This behavior is due to widespread misconceptions about the chemotherapy process, such as:
- “Nausea and vomiting always accompany chemotherapy”
- “The presence of nausea and vomiting indicates the effectiveness of chemotherapy”
- “My chemotherapy will be canceled!”
- “There are no effective treatments for nausea and vomiting”
Some patients downplay the strength and significance of developing complications and do not want to further disturb the medical staff. This behavior greatly impedes constructive interaction between patient and doctor and creates additional health risks.
How cancer therapy affects oral health
Various, often intensive and aggressive methods of therapy are used to treat cancer. Each type of cancer typically requires a different treatment regimen, which may combine surgery with chemotherapy (drugs) and radiation therapy (targeted exposure to radiation). All of these treatments are aimed at suppressing the division, development and death of cancer cells. However, they are often accompanied by painful side effects, which are associated with the fact that radiation and chemotherapy have a detrimental effect on normal tissue cells and can also suppress the functioning of the immune system. Moreover, often the more effective the treatment method, the higher the degree of toxicity for the patient.
In addition, radiation and chemotherapy often have long-term consequences for health, including dental health. It is especially important to take this into account when treating children who have undergone these types of cancer therapy.
Among the side effects of radiation and chemotherapy that have a direct impact on oral health and its treatment are:
- deterioration of general condition, weakness, nausea;
- diseases of the mucous membranes, including the oral mucosa, most often manifested as inflammation - stomatitis;
- decreased immunity and anemia, which cause frequent local bleeding.
Which chemotherapy drugs are used for which tumors?
These are 2 groups of drugs for conservative treatment of cancer - cytostatics and cytotoxins. The first ones penetrate an atypical cell, disrupt its DNA, starting the process of self-destruction. Most often, the following cytostatics are used for treatment: Hydroxyurea, Fluorouracil, Cyclophosphamide, platinum preparations.
Cytotoxins destroy cells, both cancerous and healthy, causing severe side effects in the body of cancer patients. Among these drugs there are several groups:
- anthracyclines (Daunomycin, Doxorubicin, Zavedos, Farmorubicin);
- bleomycins – antitumor antibiotics (Bleocin, Blenoxan);
- mitosans (Mitomycin is a cytotoxic antibiotic);
- targeted therapy drugs - drugs with targeted action (for example, Avastin blocks the growth of blood vessels that feed a malignant tumor).
Cytostatics and cytotoxins have the most side effects. Therefore, treatment after chemotherapy is an integral part of the process of getting rid of cancer. It allows you to speed up the restoration of body cells, alleviate the patient’s condition and improve his quality of life.
Dental treatment during chemotherapy and radiation therapy
Timely dental care can significantly improve the quality of life of a patient with cancer. Regular preventive examinations and treatment help get rid of pain and inflammation, help maintain chewing function in full, and prevent the development of pathological processes in the oral cavity.
However, when carrying out treatment, the dentist must take into account the side effects of the radiation and chemotherapy the patient receives, as well as the impact of toxic reactions on both the general condition of the patient and the health of his oral cavity.
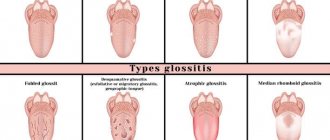
Most often, diseases of the oral mucosa occur during radiation and chemotherapy. These are stomatitis , candidiasis, tongue papillomas, “geographic tongue” (an inflammatory disease that manifests itself as a bright pattern on the tongue and causes discomfort in the mouth) and other types of glossitis (inflammation of the tongue). The increased risk of developing such diseases is due to the fact that antitumor therapy is aimed, among other things, at suppressing the body’s immune function.
Another group of diseases, the risk of which increases with antitumor therapy, is periodontal disease. They occur in 69.5% of cases, while gingivitis is observed 2 times more often than periodontitis [1].
In addition, patients receiving radiation and chemotherapy may complain of discomfort in the mouth. Among them:
- dry mouth;
- formation of ulcers and abrasions;
- taste changes;
- inflammation, swelling, bleeding gums and others.
Diagnosis of cancer of the oral mucosa
The diagnosis is established based on visual examination and confirmed by histological examination of tissue obtained from a biopsy of the affected area. If there is a suspicion that the tumor has spread into the bone tissue, a skull x-ray is indicated.
Ultrasound examination of the abdominal organs and chest radiography are prescribed to detect distant metastases. For the same purpose, it is possible to use PET-CT.
Features of the treatment of oral diseases during radiation and chemotherapy
It is important for the patient to undergo a preventive examination and consultation with a dentist in advance, before starting radiation or chemotherapy. This is due to the fact that mandatory examination of such patients should include an X-ray or tomographic examination of the condition of the bones of the jaws and teeth, which makes it possible to exclude the development of a pathological process in them.
If a patient requires oral surgery (such as tooth extraction) or dental prosthetics, treatment strategies should be discussed with the treating oncologist and dentist. As a rule, surgical interventions are recommended to be performed 2–3 weeks before the start of antitumor therapy. In addition, before starting the course of treatment, it is necessary to perform sanitation of the oral cavity (cure carious cavities), and it is also advisable to conduct a course of remineralization of the enamel.
Due to the increased risk of bleeding, poor wound healing, and the possibility of inflammation or infection when treating dental diseases in patients receiving radiation or chemotherapy, dentists must take a number of precautions.
- When examining the oral cavity, the doctor should pay attention to the condition of the gums and ask the patient about cases of inflammation or bleeding.
- All interventions must be carried out with monitoring of blood tests, in particular the level of leukocytes.
- All interventions, from local anesthetic injections to the canal depulpation procedure, must be performed in the most gentle and careful manner possible.
- Consultations between the dentist and the treating oncologist are advisable for a correct assessment of the patient’s condition.
- If necessary, a course of antibiotics is given before treatment, which reduces the risk of infection.
Kidney disorders
When undergoing chemotherapy, patients may experience side effects that affect kidney function. Chemotherapy may change the color and smell of your urine. Ask your healthcare provider what changes may occur.
If urination becomes difficult, your urine changes color (green, red, orange) or has a strong smell, be sure to tell your doctor about these symptoms.
What to do if you have kidney problems during chemotherapy?
- drink more liquid (at least 40 ml per 1 kilogram of weight) - water, fruit drinks, juices, compotes;
- Avoid drinks that contain caffeine, alcohol, and carbonated drinks.
Complications of dental development during radiation and chemotherapy
Treatment of malignant neoplasms in childhood significantly affects dental development. It is important to understand that the development of teeth is one of the longest processes in the human body, because teeth are fully formed only by the age of 21–22 [4]. Tooth buds contain embryonic tissues that have the properties of intensively dividing and developing. If a child or teenager receives radiation or chemotherapy aimed at suppressing active cell growth, this inevitably affects the development of teeth. In particular, the impact manifests itself as follows:
- the resistance of teeth to cariogenic factors decreases;
- the constancy of the composition (homeostasis) of the oral fluid changes, including its cleansing properties, the protective function and content of trace elements and minerals involved in the remineralization of enamel and others decreases;
- teething is delayed;
- the risk of developing dental anomalies increases, for example, underdevelopment of tooth roots, microdentia, impaired enamel formation, and the formation of cavities;
- the rudiments of teeth die, which leads to their absence, while the likelihood of tooth loss is especially significant when chemotherapy is administered before the age of 9 years [4].
Children who have undergone chemotherapy should be routinely examined by a dentist at an early age (optimally at the age of 6 years, when the buds of all teeth are normally well mineralized and visible on radiographs, and for older children - after completion of chemotherapy) for timely diagnosis of edentia and prevention secondary deformation of the dental arches
Korolenkova M. V., Ph.D., pediatric dentist, Central Research Institute of Dentistry and Maxillofacial Surgery[4]
The effect of chemotherapy on the condition of hair, nails, skin
Chemotherapy affects the condition of your skin, nails and hair, as their cells regenerate quickly and are especially sensitive to chemotherapy.
Hair loss (alopecia) due to chemotherapy occurs after several weeks of treatment. This is a harmless side effect, but it causes a lot of inconvenience.
Remember that this is a temporary side effect; your hair will return 3-6 months after completing chemotherapy.
What to do with alopecia?
- try changing your hairstyle: cut your hair short, shave your head, pick up a wig;
- treat your hair with care (use mild shampoo);
- Protect your head from ultraviolet radiation and strong temperature changes.
The condition of your skin and nails may also change during chemotherapy. Your skin may become particularly dry and flaky, your sensitivity to ultraviolet light may increase, and your nails may begin to yellow and peel.
What to do?
- protect your skin from ultraviolet radiation by using creams and hygienic lipstick with a high protection factor;
- Avoid visiting the solarium and taking hot water baths;
- take good care of hygienic skin and nail care;
- try to shave less to reduce the risk of damaging your skin;
- cut your nails short;
- When washing dishes and cleaning, use protective gloves;
Features of oral hygiene in cancer patients
Given the side effects of radiation and chemotherapy for cancer and the development of possible complications, oral hygiene is of particular importance for patients. It allows you to prevent the development of many diseases and prevent the deterioration of the mucous membrane of the oral cavity and teeth.
It is important for the patient to especially carefully follow all the rules of oral hygiene. First of all, hygiene procedures for cancer patients should include:
- brushing your teeth twice a day, using a toothbrush with soft bristles, which will help avoid injury to the gums, as well as fluoride-containing toothpaste ;
- careful and gentle cleaning of interdental spaces with dental floss (if gums are bleeding, painful areas should be avoided);
- rinsing your mouth with water will help relieve dryness and prevent irritation of the oral mucosa.
During antitumor therapy, it is not recommended to use rinses containing alcohol, as it can cause unpleasant and painful sensations in the oral cavity and increase dryness of the mucous membrane. In addition, the dentist may recommend the use of saliva substitutes to eliminate dryness, discomfort and prevent caries and inflammation. Another remedy to help cope with dry mouth is chewing gum, which stimulates saliva production. Patients undergoing radiation or chemotherapy are advised to use sugar-free chewing gum.
In addition, it is important for the patient to independently examine the oral cavity (gums, tongue and mucous membranes) daily, paying special attention to pain, bleeding, abrasions and wounds. Regular examinations by a dental specialist who can promptly detect a possible problem and select the necessary treatment are also becoming critically important. In addition, it is very important to visit your dentist before starting radiation or chemotherapy.
List of sources
- Features of dental status in patients with cancer, Uspenskaya O. A., Fadeeva I. I. // Problems of dentistry. 2022. No. 1. - URL: https://cyberleninka.ru/article/n/osobennosti-stomatologicheskogo-statusa-u-patsientov-s-onkologicheskimi-zabolevaniyami (date of access: 09/06/2020).
- WHO outlines measures to save 7 million lives from cancer // WHO, News Release February 4, 2020, Geneva. — URL: https://www.who.int/ru/news-room/detail/04-02-2020-who-outlines-steps-to-save-7-million-lives-from-cancer (access date: 09/06/2020).
- Statistics of oncological diseases in the Russian Federation // Kommersant newspaper No. 28 dated 02/15/2020, p. 2. - URL: https://www.kommersant.ru/doc/4258255 (date of access: 09/06/2020).
- Korolenkova M.V. Dental malformations in children after chemoradiotherapy // Vestn. RONC named after. N. N. Blokhin RAMS. 2015. No. 1. - URL: https://cyberleninka.ru/article/n/poroki-razvitiya-zubov-u-detey-posle-himioluchevogo-lecheniya (date of access: 09/06/2020).
What to do if your temperature rises after chemotherapy?
If a cancer patient is undergoing chemotherapy as an outpatient, then an increase in body temperature is the reason for a mandatory visit to the doctor outside of the scheduled appointment. Even in the absence of accompanying symptoms, the body’s signals cannot be ignored.
Contacting the Yusupov Hospital can be done independently, in the form of an online consultation, a telephone conversation with a doctor, an appointment for the near future, or a doctor visiting your home.
Before contacting a doctor, you should do the following:
- taking an antipyretic (after doctor’s recommendations);
- measuring temperature every 1–2 hours and recording changes in a special diary;
- compliance with bed rest;
- applying a cold compress to the forehead if headaches or chills occur.
You cannot take medications on your own. It should be remembered that chemotherapy involves the introduction of toxic drugs into the body that can cause a dangerous reaction in combination with certain other drugs.