Gum inflammation
Recommended Articles
- Causes of gum inflammation
- Types of inflammation
- Main manifestations and symptoms
- Diagnostic features
- Treatment methods
- Prevention methods
Gum inflammation is a general concept that includes both superficial and deep inflammatory processes. Everyone faces this problem to one degree or another, and in the absence of proper attention to the condition of the oral cavity, inflammation can lead to serious consequences, including the loss of healthy teeth. It is important to recognize in time not only the onset of inflammation, but also to assess the depth of its spread, receive qualified dental care and prevent complications.
Injections of antibiotics into the gums –
I would like to say a few words about such a treatment method as injections of antibiotics into the gums. This method of treatment has never been used abroad due to the enormous harm that such injections cause to the gums. In Russia, this method of treatment was previously very common due to its low cost and low qualifications of dentists (in conditions where the treatment of periodontal diseases is not carried out by periodontologists specially trained for this, but by any ordinary dentist).
Below we will explain why, if a clinic offers you a course of antibiotic injections into your gums, you should immediately run away from this clinic and look for another clinic/another doctor. The visible part of the treatment is basically that injections into the gums can actually lead to a decrease in the intensity of inflammation (bleeding, pain, swelling and redness of the gums are reduced). Although some patients may already experience gum abscessation at this stage, this is especially common in the presence of deep periodontal pockets.
How are antibiotic injections given in the gums?
Injecting an antibiotic directly into the gum results in the creation of a terrifyingly high concentration of antibiotic in the gum and bone tissue around the tooth. The antibiotic lincomycin is usually prescribed. In low concentrations it is bacteriostatic, but in high concentrations it begins to have a bactericidal effect, which leads to the immediate destruction of a very large number of pathogenic microorganisms (and not gradually, as it should be). The death of pathogenic bacteria is always accompanied by the release of a large number of toxins, various pathogens, as well as so-called “cytokines” (inflammatory mediators).
When too many of them are thrown out at the same time, this leads to the appearance of multiple foci of necrosis in the periodontium (the periodontium is the ligamentous apparatus of the tooth, with the help of the fibers of which the tooth is connected to the bone tissue). Such areas of necrosis heal with the formation of scar tissue, the formation of which initially gives the appearance of strengthening the tooth, but, unfortunately, the joy does not last long. Normal periodontium of teeth is adapted to bear a large mechanical (chewing) load, which cannot be said about scar tissue. And as soon as the area of attachment of the tooth to the bone decreases due to the normal periodontium, a mechanical overload of the ligamentous apparatus of the tooth occurs.
As a result, the bone tissue around the tooth begins to dissolve, which leads to an even greater increase in its mobility. Moreover, in this case, mobility will no longer be associated with inflammation, but with a decrease in bone level, as well as a decrease in the area of periodontal attachment of the tooth root to the bone. And this is irreversible mobility, which cannot be corrected by any treatment.
Gingivitis
This is the first and reversible stage of periodontitis. Gingivitis is inflammation of the gums. This disease is very dangerous during pregnancy - due to changes in the hormonal levels of the pregnant woman, the disease progresses faster than usual, can lead not only to the loss of teeth in the pregnant woman herself, but also cause dental problems in the future in the child, and even provoke premature birth.
If you notice the following signs, then most likely these are symptoms of developing gingivitis:
gum inflammation, bleeding,
bright red gum color,
pain and swelling in the gum area,
bad breath, quickly forming plaque and stones.
Important: combination of antibiotic and antiseptics
When treating gum inflammation (chronic generalized periodontitis), antibiotics alone are not enough.
In this case, treatment should be comprehensive - removal of dental plaque, antibacterial therapy, antiseptic mouth rinses + the use of a special anti-inflammatory gel for gums. Now we would like to tell you why it is important to combine antibiotics with mouth rinses with antiseptic solutions when treating periodontitis. In case of aggressive periodontitis, as well as moderate and severe periodontitis, in addition to pathogenic bacteria, fungal flora (fungi of the genus Candida) is also present in the periodontal pockets. The presence of fungal flora in periodontal pockets actually has a very important impact on the effectiveness of antibacterial therapy of gums for periodontitis. The fact is that fungi of the genus Candida form so-called “microbial associations” with pathogenic bacteria, which makes the bacteria insensitive to many antibiotics.
There are scientific works (source) that show the comparative effectiveness of different types of antiseptics and their different concentrations in the treatment of chronic generalized periodontitis, in which Candida fungi are present in periodontal pockets. Clinical studies show that there are only 2 antiseptics that are simultaneously effective against common pathogenic bacteria and Candida fungi for periodontitis. This is primarily 0.2% chlorhexidine, and also to a lesser extent 0.1% hexetidine (the drug “Hexoral solution”).
Important: most often, Candida fungi in periodontitis occur in the following categories of patients. For example, if your gum inflammation is of a long-term chronic nature (i.e., we are talking about moderate or severe periodontitis), with aggressive periodontitis. And also, if you smoke, or eat a lot of carbohydrates, or if you have concomitant chronic tonsillitis, or gastrointestinal diseases, or in the past - at least 1 case of candidiasis (thrush) of any localization.
→ The best mouth rinses for periodontitis, → Rating of the best gels for gums.
Antibiotics for implantation –
A separate issue of the use of antibiotics is their use in implantology - in preparation for surgery, its accompaniment and use in the early postoperative period - for the prevention of infectious complications, as well as for the treatment of already existing infectious complications (peri-implantitis). Read more about the choice of antibiotics in these cases in the article:
→ Choice of antibiotics in implantology
Antibiotics after tooth extraction
One of the surgical operations in dentistry is the removal of wisdom teeth. Antibiotics in the preoperative period are prescribed for prophylactic purposes to patients with glomerulonephritis, endocarditis, diabetes mellitus, and those with weakened immune systems. Prevention is possible with planned removal, which is carried out in case of atypical position and mobility of the unit, in case of chronic cysts and periodontitis, in case of mechanical damage without the possibility of recovery after sanitation of the oral cavity.
An antibiotic is also prescribed after tooth extraction if the operation is performed as an emergency. More often, Ciprofloxacin. What antibiotics to take after tooth extraction is prescribed by the dentist, taking into account the specifics of the microflora. The main indications for such removal are acute purulent inflammatory diseases localized to bone tissue, abscesses, lymphadenitis, and phlegmon. Antibiotics are used for tooth extraction if it is not subject to conservative treatment, including filling, due to extensive destruction and loss of functionality.
Antibiotics for wisdom tooth removal are prescribed if the integrity of bone or soft tissue was damaged during the procedure, which in the future can provoke infection, inflammation, and the formation of gumboil. Antibiotics after wisdom tooth removal are prescribed for the following complications:
- Alveolitis. It develops 3-4 days after surgery and is characterized by a dry gray lump with a whitish coating. The pathology is characterized by an unpleasant odor, pain, swelling of the cheek, and an increase in temperature to 38-39 °C.
- Apical periodontitis. Periodontal inflammation of an infectious, traumatic or medicinal nature is treated comprehensively. It is necessary to ensure the outflow of exudate, prescribe broad-spectrum antibiotics, antiseptic treatment, and filling the canals.
- Osteomyelitis. A purulent-necrotic process caused by pyogenic bacteria and mycobacteria. With this pathology, hospitalization is necessary. How and what antibiotics to take for this pathology after tooth extraction will be prescribed by the leading doctor.
Regenerating drugs
The main problem in the treatment of periodontal disease is the restoration of tissues damaged or destroyed during the development of the disease. For this purpose, a variety of drugs are used, including stem cells and other biogenic stimulators of regenerative processes. They are most often administered by injection directly into the affected areas of the gums. Modern methods of treating periodontal disease include the use of the following drugs:
- Fibroblasts
Fibroblasts are connective tissue cells that play an extremely important role in the healing process of wounds and injuries, and also participate in the synthesis of collagen and elastin fibers, which make the soft tissues of the body more elastic. The introduction of fibroblasts helps restore the elasticity and firmness of sagging gum tissue, and also increases the protective properties of the mucous membranes of the oral cavity. The strength of fabrics and their resistance to destructive influences of various natures also increases significantly.
- Stem cells
The anti-aging properties of stem cells are widely known in modern medicine and, especially, cosmetology. Stem cell preparations can stimulate regenerative processes and promote accelerated restoration of cellular structures. Under their influence, the healing process of damage is accelerated, which is extremely important in the treatment of periodontal disease and related diseases.
- Platelet-derived growth factor
Platelet growth factor is a special protein synthesized by the body and involved in the processes of tissue growth and repair. In addition, the growth factor promotes accelerated synthesis of collagen, glycosaminoglycans and other components of connective tissue.
The use of biogenic drugs is an extremely promising direction in modern medicine, but these methods are not widely used today due to technological complexity and high cost. To stimulate recovery processes, you can use more accessible means, in particular propolis. This substance is included in a wide variety of hygiene, therapeutic and prophylactic products; in particular, it is the main active component of the antimicrobial gel for gums ASEPTA. In addition to stimulating tissue restoration, propolis also has a pronounced antimicrobial and anti-inflammatory effect, reduces the sensitivity of damaged gums, and eliminates bleeding.
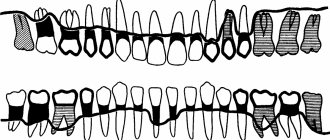
Types of inflammatory and dystrophic gum diseases
Inflammatory manifestations include:
- Gingivitis
- Periodontitis
Dystrophic manifestations include:
Gingivitis: signs, causes and treatment
Gingivitis is the first stage of inflammation, in which the integrity of the periodontal junction has not yet been compromised. This disease can be identified by the following signs:
- Swelling of the gums.
- Blood while brushing teeth.
- Pain when eating cold, hot or solid foods.
Improper brushing of teeth, errors during fillings and dentures, improper bite – all this can cause gingivitis. By the way, this is one of the most popular problems that pediatric dentists encounter.
Treatment of gingivitis involves a set of procedures carried out in a dental clinic and at home. If there is dental plaque, it is necessary to carry out ultrasonic cleaning. In addition, you should pay more attention to hygiene: brush your teeth properly and use antibacterial agents.
Periodontitis
Periodontitis is a pathology that occurs as a result of advanced gingivitis. In this case, the swelling of the gums becomes even stronger, they begin to bleed frequently. If left untreated, infection and pus may form. As a result, the bone tissue begins to atrophy, and this leads to increased sensitivity of the teeth, their mobility, and sometimes even loss.
Treatment of periodontitis is prescribed taking into account the course of the disease. At first, procedures such as removing plaque from the enamel and regular brushing of teeth with antiseptic agents may be sufficient. In more serious situations, when the infection has penetrated deep into the bone tissue, surgery may be necessary:
- Partial gum excision.
- Cleaning periodontal pockets.
- Implantation of bone tissue substitutes.
Periodontal disease
Periodontal disease is a systemic disease. As a rule, it is typical for elderly patients. Inflammatory-dystrophic manifestations in this case are concentrated in the periodontal tissue.
Periodontal disease develops at a leisurely pace, gradually erasing tooth enamel. The presence of this disease can be determined by exposed tooth roots and cervical chips of tooth enamel. In most cases, no pain occurs, but if you ignore the problem, you can “lose” your teeth.
To eliminate periodontal disease, it is necessary not only to observe and treat the dentist, but also to related specialists.
Treatment of inflammation at home
The course of treatment of teeth and gums is always selected taking into account the individual characteristics of the disease:
- A type of inflammatory process.
- Neglect of pathology.
- Patient's age.
For example, in adult patients, inflammatory processes most often occur due to chronic diseases. To eliminate the problem, as a rule, pharmaceutical products are required - antiseptics, gels, ointments, antibiotics, toothpastes. If a child’s gums become inflamed, this is almost always associated with teething and herbal medicine, that is, rinsing with herbal decoctions and using other methods of traditional medicine, is sufficient for treatment.
Whatever the situation, adequate treatment is only possible after consultation and diagnosis by a qualified doctor. Remember that the wrong choice of procedures can not only fail to produce results, but also cause painful complications.
Antiseptics
Rinsing with antiseptic agents is the most important step in the fight against inflammatory processes. Let's name well-proven drugs that can be purchased at the pharmacy:
- Malavit - reduces inflammation and prevents its development, but does not eliminate pain effectively enough.
- Kamistad – recommended in the presence of severe pain. It also copes well with swelling.
- Chlorhexidine is a suitable treatment for gingivitis in children. Daily rinsing after meals is recommended.
- Listerine is a good drug for eliminating swelling. Suitable for all types of gum inflammation.
- Stomatophyte is an antiseptic made from natural raw materials: chamomile flowers, oak bark and sage leaves.
- Furacilin is an excellent antimicrobial agent. Penetrates inside the microbial cell, preventing its division.
- Miramistin is an anti-inflammatory drug with a pronounced antimicrobial effect.
Gels and ointments
Therapeutic gels and ointments are applied to the inflamed gums after rinsing with antiseptic agents. They provide effective protection to the mucous membrane, preventing infection from entering wounds and helping to cope with pain.
List of the most effective gels and ointments:
- Metrogyl Denta is a powerful antiseptic gel. It has pronounced anti-inflammatory and analgesic properties.
- Cholisal is one of the best options for combating inflammation that occurs due to internal reasons. Relieves pain well.
- Kamistad - suitable for both preventing gingivitis and combating complications (severe swelling, pain).
- Gengigel is an excellent healing agent. Improves blood supply, promoting rapid healing of wounds in the oral cavity.
- Stomatophyte A – recommended for severe and prolonged pain.
- Asepta - contains propolis, which provides accelerated tissue regeneration and reduces inflammation.
- Solcoseryl is a healing agent with a pronounced anesthetic effect.
Vitamins and minerals
To restore damaged tissues, the body needs a wide variety of nutrients, which are not always contained in the required quantities in the daily diet. That is why the drug treatment regimen for periodontal disease often includes taking vitamin complexes. The best effect can be achieved by taking special complexes, for example, the vitamin-mineral complex for teeth ASEPTA.
The ASEPTA complex includes a whole range of substances necessary to strengthen gums and teeth. Vitamin C strengthens the walls of capillaries and blood vessels, helping to improve blood circulation in the gums, disruption of which is one of the main causes of periodontal disease. Vitamins B3 and B6 help reduce gum sensitivity, strengthen bone tissue and promote healthy mucous membranes. Vitamin A is involved in all metabolic processes occurring inside the body and increases protection against inflammatory and infectious diseases that often accompany periodontal disease.
In addition to vitamins, the complex also contains green tea extract - a natural component that has an antimicrobial effect, eliminates unpleasant odors, and slows down the aging process of tissues. An equally important component of the complex is coenzyme Q10, a substance that is a rich source of energy for the growth and restoration of cellular structures. Taking coenzyme promotes accelerated regeneration of damaged gums.
The complex also includes substances intended to strengthen the hard parts of the tooth, which are subject to increased stress during periodontal disease - coral calcium, which is well absorbed by the body, and vitamin D3, necessary for the proper absorption of calcium and phosphorus.
Description
Compound
active ingredients: metronidazole benzoate, chlorhexidine digluconate
1 g of gel contains metronidazole benzoate in terms of metronidazole 10 mg, chlorhexidine digluconate solution 20% in terms of chlorhexidine digluconate 0.5 mg
excipients: carbomer, propylene glycol, sodium saccharin, trilon B (trilon B), triethanolamine, peppermint oil, purified water.
Dosage form
Basic physical and chemical properties:
gel is white or almost white in color with a specific odor. It should be uniform in appearance.
Pharmacological group
Products for use in dentistry . Antimicrobial and antiseptic agents for topical use in dentistry.
Pharmacological properties
Antimicrobial combination drug for the complex treatment and prevention of certain infectious and inflammatory diseases of the oral cavity.
The effectiveness of the drug is due to the presence of two antibacterial components - metronidazole and chlorhexidine.
Metronidazole is a nitroimidazole derivative that has antiprotozoal and antibacterial effects. Active against anaerobic bacteria that cause periodontal diseases: Porphyromonas gingivalis, Prevotella intermedia, Prevotella denticola, Fusobacterium fusiformis, Wolinella recta, Eikenella corrodens, Borrelia vincenti, Bacteroides melaninogenicus, Selenomonas spp.
Chlorhexidine is a bactericidal antiseptic. Active against a wide range of vegetative forms of gram-negative and gram-positive microorganisms, as well as yeast, dermatophytes and lipophilic viruses.
The minimum inhibitory concentration (MIC50) of metronidazole for anaerobic bacteria is below 1 μg/ml. When applied topically (applied to the gums), the concentration of metronidazole in the gum area is significantly higher than when the drug is administered orally, and the level of systemic absorption of metronidazole when applied topically is significantly lower than when administered orally. The main route of excretion of metronidazole and its metabolites is the kidneys. Reduced renal function does not alter the pharmacokinetics of a single dose of metronidazole.
If excess chlorhexidine is ingested, when applied topically as part of a dental gel, about 1% of the dose that enters the stomach is absorbed from the digestive tract. Chlorhexidine does not accumulate in the body and is minimally metabolized.
Diarrhea after taking antibiotics –
Taking antibiotics can often lead to the development of diarrhea, and there is even such a term as antibiotic-associated diarrhea. Most often, diarrhea is caused by penicillin derivatives and cephalosporins (β-lactam antibiotics) - especially their tablet forms, although the development of diarrhea is possible after their intramuscular or intravenous administration. The main pathogen that leads to the development of diarrhea is Clostridium perfrogens. The rapid growth of this pathogen occurs due to the fact that antibiotics suppress not only pathogenic flora, but also bifidobacteria, lactobacilli, enterococci and Escherichia coli, which under normal conditions inhibit the growth of Clostridium perfrigens.
But the mechanism of development of diarrhea can be complex, i.e. may take into account not only the suppression of beneficial microflora. For example, clavulanic acid as part of a number of antibiotics can increase intestinal motility, thereby causing hyperkinetic diarrhea. Antibiotics of the cephalosporin group (especially cefixime or cefoperazone) are poorly absorbed from the intestinal lumen, which can lead to so-called hyperosmolar diarrhea.
Diarrhea most often occurs –
- in 10-25% of cases – when prescribing drugs “amoxicillin + clavulanic acid”,
- 15-20% – when prescribing cefixime (this is a cephalosporin),
- 5-10% – when prescribing ampicillin or clindamycin,
- 2-5% – when prescribing other cephalosporins (except cefixime), as well as macrolides (erythromycin, clarithromycin),
- and only 1-2% when prescribing fluoroquinolones.
Conclusions: i.e. If you have already had cases of diarrhea after taking Amoxiclav or Augmentin (containing amoxicillin and clavulanic acid), then it is better to opt for other groups of antibiotics. First of all, these are modern fluoroquinolones, and it is especially worth paying attention to those fluoroquinolone preparations that are combined with tinidazole (for example, Tsiprolet-A or Tsifran-ST).
Another type of severe antibiotic-associated diarrhea is called “pseudomembranous colitis”. Its development is already associated with another microorganism - Clostridium difficile. The development of pseudomembranous colitis is primarily associated with the use of clindamycin, ampicillin and cephalosporins. Moreover, unfortunately, experience shows that the risk of its development when taking Russian antibiotics is much higher.
How to reduce the risk of diarrhea after taking antibiotics -
Firstly, taking probiotics in parallel can help you with this. These are drugs that contain bacteria that are beneficial to our intestines. There are a large number of probiotics, for example, some of the best are the drug Linex, as well as Bifiform. Keep in mind that it is better to choose multicomponent preparations that contain several types of beneficial bacteria.
Probiotic Bifiform (30 capsules) –
Another option to reduce the risk of diarrhea is to choose an antibiotic combined with tinidazole or metronidazole (if the risk of diarrhea is high, and if indicated). We hope that our article: Antibiotics for toothache and gum disease was useful to you!
Sources:
1. Dental education of the author of the article, 2. Based on personal experience as an oral and maxillofacial surgeon, dental surgeon, 3. National Library of Medicine (USA), 4. “Systemic antibacterial drugs in periodontology” (Mazur I.P.), 5. “Sensitivity of microbial associations of periodontal pocket exudate and odontogenic focus to antibacterial drugs” (Makeeva I.M.).
Metrogyl Denta - composition and release form of the drug
The drug is available in the form of a white or almost white gel. Active ingredients : metronidazole benzoate, chlorhexidine gluconate.
1 gram of gel contains: metronidazole benzoate - 16 mg (in terms of metronidazole 10 mg); chlorhexidine gluconate solution (20%) (2.5 mg, based on chlorhexidine gluconate 0.5 mg).
Excipients : saccharin, sodium hydroxide, disodium edetate, levomenthol, propylene glycol, carbomeric homopolymer (type C), purified water.
Consequences of periodontal disease
Periodontal disease requires urgent treatment, as it can lead to serious consequences:
- gingivitis;
- periodontitis;
- intoxication of the body with pus;
- loss of teeth;
- cancerous tumors;
- impossibility of prosthetics;
- pulpitis;
- serious problems in the gastrointestinal tract.
Specialists of the 32 Dent clinic network specialize in the treatment of all types and forms of periodontal disease. Every day, doctors help patients once and for all get rid of a problem that brings internal discomfort and unaesthetic changes.
Dosage regimen
The gel is intended for topical use in dentistry only.
For adults and children over 6 years of age with gum inflammation (gingivitis), Metrogyl Denta ® is applied to the gum area in a thin layer with a finger or with a cotton swab 2 times a day. After applying the gel, you should refrain from drinking and eating for 30 minutes. It is not recommended to wash off the gel. The duration of treatment is on average 7-10 days.
In case of periodontitis, after removing dental deposits, periodontal pockets are treated with Metrogyl Denta ® gel and the gel is applied to the gum area. Exposure time - 30 minutes. The number of procedures depends on the severity of the disease. In the future, the patient can apply the gel independently:
- Metrogyl Denta ® is applied to the gum area 2 times a day for 7-10 days.
For aphthous stomatitis, Metrogyl Denta ® is applied to the affected area of the oral mucosa 2 times a day for 7-10 days.
To prevent exacerbations of chronic gingivitis and periodontitis, Metrogyl Denta ® gel is applied to the gum area 2 times a day for 7-10 days. Preventive courses of treatment are carried out 2-3 times a year.
To prevent post-extraction alveolitis after tooth extraction, the hole is treated with Metrogyl Denta ® gel, then the gel is applied 2-3 times a day for 7-10 days.
Antibiotics for gumboil and inflammation of tooth roots -
Let's look at what antibiotics can be used for adults for gum gum disease. The choice here is quite large, for example, ranging from inexpensive antibiotics - such as lincomycin or amoxicillin, to more expensive drugs (for example, β-lactam antibiotics, 2nd generation fluoroquinolones and macrolides). Below we will look at the most popular antibiotics and tell you whether they work well for this type of dental inflammation.
1) Amoxiclav (or Augmentin) - these drugs contain a combination of “the antibiotic amoxicillin and clavulanic acid.” Many modern pathogenic bacteria produce β-lactamase enzymes that destroy amoxicillin. Clavulanic acid protects amoxicillin from the action of beta-lactamases, which greatly increases the effectiveness of the antibiotic. But using the most common amoxicillin (without combination with clavulanic acid) in dentistry today is already pointless.
The dosage regimen for adults is 500 mg 2-3 times a day (2 or 3 times depending on the severity of inflammation), the duration of administration is usually 5 days, but if necessary, the doctor can extend the drug for another 2-3 days. A package of the antibiotic Amoxiclav (15 tablets of 500 mg) costs from 330 rubles, and a package of the antibiotic Augmentin (14 tablets of 500 mg) costs from 180 rubles. And we do not recommend purchasing their Russian analogues containing a combination of “amoxicillin and clavulanic acid,” especially since they will not be cheaper.
Important: if you decide to purchase inexpensive amoxicillin (without clavulanic acid), then it should be used at least in combination with the antibiotic metronidazole (Trichopol). The latter is taken for purulent infections according to the same regimen - 500 mg 3 times a day (5-7 days in total). Only in this case can we expect at least some acceptable effectiveness from the treatment.
2) Ciprofloxacin (Tsiprolet) - this inexpensive, popular antibiotic belongs to the 2nd generation fluoroquinolones. The recommended regimen for use in adults is 500 mg 2 times a day (for 5 days), and the cost of a package of the Indian-made drug will be about 120 rubles. It works well for apical periodontitis, i.e. inflammation at the apex of the tooth root. In addition, the risk of developing diarrhea with this drug is lower - compared to β-lactam antibiotics (Amoxiclav, Augmentin).
Antibiotic Tsiprolet (10 tablets, 500 mg each) –
However, if we are talking about long-term apical periodontitis (especially if there have been cases of a fistula with purulent discharge in the projection of the tooth root), if there is acute pain indicating the formation of a purulent abscess at the apex of the tooth root, it would be optimal to prescribe an antibiotic containing the combination “ciprofloxacin” + tinidazole." These are drugs - “Ciprolet-A” or “Tsifran-ST”, in which, in addition to 500 mg of ciprofloxacin, each tablet also contains 600 mg of tinidazole. Their cost is from 210 and 320 rubles, respectively, but 1 package of each drug will be enough for you for a full 5 days of antibiotic therapy.
Tinidazole is an antibacterial drug with antiprotozoal activity, i.e. it is effective against anaerobic microorganisms (which are especially numerous during the formation of pus at the site of inflammation). In addition, tinidazole is very effective against Clostridium difficile and Clostridium perfringens, which are responsible for the development of diarrhea while taking antibiotics, and thus, when taking combination antibiotics with tinidazole, diarrhea is practically excluded.
3) Azithromycin (Azitral) - it is usually prescribed for allergies to β-lactam antibiotics (for example, amoxicillin). There are different regimens of use, but according to studies for purulent odontogenic infections, the optimal treatment regimen is to take a single dose of 1000 mg for 1 day, after which the drug is taken for another 2 or 3 days at a dose of 500 mg once a day. But the price of this antibiotic will be high if we do not take into account Russian manufacturers.
For example, a good Indian drug with azithromycin “Azitral” will cost you 220 rubles per package of 3 capsules of 500 mg (it turns out that you will need to purchase 2 packages for the course). The short course of use is due to the fact that this antibiotic has a cumulative effect, and therefore, even after taking it, therapeutic concentrations of the antibiotic remain in the body for several days.
Is it worth using Azithromycin for complications of caries (apical periodontitis, swelling or fistula on the gum, or gumboil on the face) - it’s definitely not worth it. This is due to the fact that in patients with inflammation at the apex of the tooth, drugs with azithromycin show good effectiveness only in 50% of cases, and in the remaining half of patients, the sensitivity of the microflora in the inflammation site to azithromycin is regarded as “low”. Below we will also demonstrate scientific works that confirm this.
4) Lincomycin or Clindamycin are quite old antibiotics belonging to the lincosamide group. Moreover, clindamycin is a more effective analogue of lincomycin (in terms of effectiveness against certain types of pathogenic bacteria that cause purulent inflammation, it is 2-10 times more effective than lincomycin). The peculiarity of these antibiotics is a certain affinity for bone tissue, which is an advantage for purulent inflammation in the teeth, as well as their low price. The disadvantages include a narrow spectrum of antimicrobial action, as well as the fact that they often cause diarrhea.
The regimen for taking Lincomycin is 2 capsules 3 times a day, for a total of 5 days (a package of the drug costs only 60 rubles). Clindamycin dosage regimen: 1 capsule 150 mg 4 times a day for 4 days. The latter is the drug of choice for allergies to β-lactam antibiotics, which include penicillins, amoxicillin, cephalosporins, etc. Affordable price – pack of 16 tablets. 150 mg each (made in Serbia) costs approximately 160 rubles. To prevent diarrhea while taking antibiotics, they should also be combined with tablets. Metronidazole.
Is it worth using Lincomycin - modern studies show that lincomycin shows good effectiveness only in 36.8% of cases (in at least 63.2% of cases - pathogenic bacteria in the inflammation site have only weak sensitivity to lincomycin). Moreover, if we are talking about a long-existing focus of inflammation in the area of the tooth root (in the presence of a fistula or purulent abscess), lincomycin is effective only in 19% of cases, at the same time in 47.6% of cases it demonstrates only weak effectiveness, and in the remaining 33 .4% of cases – patients have complete resistance of the microflora in the inflammation site to lincomycin.
It is also worth considering that lincomycin has very low bioavailability (when taken on an empty stomach, only about 30% of the drug is absorbed through the intestines). Simultaneous food intake reduces bioavailability by 4-5 times, i.e. bioavailability will be only about 5%. Taking on an empty stomach and poor bioavailability make the drug excessively harmful to the normal microflora of the stomach. In addition, taking Lincomycin can often cause antibiotic-dependent diarrhea.
SUMMARY (which antibiotic is better for inflammation at the root of the tooth) –
To compare the effectiveness of antibiotics in this article, the author of the article used personal experience in prescribing them, as well as the scientific work “Sensitivity of microbial associations of exudate of a periodontal pocket and odontogenic lesion to antibacterial drugs” (Makeeva I.M., Daurova F.Yu.), which was performed in 2016 at the Medical University. Sechenov, Moscow.
From this work we learn the following. In patients with apical periodontitis (inflammation at the apex of the tooth root), antibacterial drugs with the combination of amoxicillin + clavulanic acid were highly effective in 79-80% of cases, for ciprofloxacin (without tinidazole) - in 76% of cases, for azithromycin - from 66 % to 52% of cases, and for lincomycin - only from 36% to 19% of cases. Thus, if you have swelling of the gums or gumboil on your face, or there is acute pain when biting on a tooth, you should definitely not use lincomycin or azithromycin.
The 1st choice drugs are 2nd generation fluoroquinolones, namely the antibiotic ciprofloxacin (you can use the usual “Tsiprolet”, but the best drugs are those where ciprofloxacin is combined with tinidazole - these are “Ciprolet-A” or “Cifran-ST” ). Moreover, the last 2 drugs are the first choice drugs also for those patients who have a history of diarrhea during antibacterial therapy. In second place are β-lactam antibiotics such as Amoxiclav or Augmentin, which can be used as monotherapy or in combination with metronidazole (to enhance the effect in purulent inflammation).
If we are talking about the need for antibacterial therapy in a hospital setting (purulent abscesses, phlegmons, odontogenic osteomyelitis, etc.), then the drugs of first choice will be antibiotics of the cephalosporin group (i.m.), for example, the antibiotic Ceftriaxone.
Important: Remember that you should not take antibiotics on your own without a doctor's prescription. The choice of antibiotic is made by the doctor, taking into account the specific situation in the oral cavity, the severity of purulent inflammation, and also taking into account your chronic diseases. Antibiotics for gum gum disease are prescribed immediately after opening the tooth by a dentist, as well as after making a small incision in the gum (if necessary). But antibiotics cannot be a replacement for these medical procedures, because... Antibiotics are not able to “sterilize” infection in root canals and around the apex of the tooth.
Treatment with antibiotics for swelling of the gums near a tooth or acute pain when biting on a tooth is not the main treatment. If it is possible to save a tooth, the root canals must first be opened (to create an outflow of purulent discharge from the source of inflammation at the apex of the tooth root). And only after this are antibiotics prescribed. If you use an antibiotic just to suppress inflammation, you create a situation in which the infection at the site of inflammation becomes resistant to the antibiotic, and subsequent exacerbations of inflammation will be much more serious.
Antibiotics for toothache -
Tooth pain is a consequence of either inflammation of the nerve in the tooth (this disease is called pulpitis) or inflammation at the apex of the tooth root (apical periodontitis). Antibiotics for toothache do not quickly reduce it, because... they do not have an analgesic effect. True, they can reduce pain indirectly - by reducing inflammation, but this effect will develop for so long that it does not have any clinical significance.
An effective remedy for relieving toothache are non-steroidal anti-inflammatory drugs (NSAIDs), which include Nurofen, as well as other much stronger analgesics. You should start taking antibiotics before visiting the dentist only in one case, for example, if in the evening or at night you have acute pain when biting on a tooth or swelling of the gums/face, but you are planning an urgent visit to the dentist the next day.
Metroxidine denta
- Description
- Quality control
Dosage form
Composition per 1 g
Active ingredients:
- Metronidazole benzoate – 16.0 mg
- Equivalent to metronidazole – 10.0 mg
- Chlorhexidine digluconate solution 20% – 2.5 mg
- Equivalent to chlorhexidine bigluconate – 0.5 mg
Excipients:
propylene glycol – 50.0 mg, carbomer-980 – 15.0 mg, disodium edetate – 0.5 mg, saccharin – 1.0 mg, levomenthol – 5.0 mg, sodium hydroxide – 4.0 g, purified water – up to 1 year
Cost of periodontal disease treatment
The price of periodontal disease treatment depends on the following factors:
- volume of lesion;
- type of periodontal disease;
- forms of the disease;
- general condition of the oral cavity;
- chosen type of treatment.
On average, periodontal treatment in a good clinic costs from 1000 rubles per tooth. The total price of therapy is calculated individually. To find out the cost of effective treatment in a particular case, sign up for a consultation with a 32 Dent dentist.