What is bifurcation
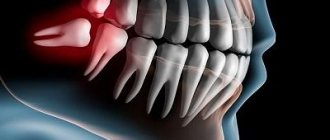
The bifurcation of a tooth is the area on the tooth itself where the branching of its roots begins (you can see what it looks like in the photo below). The term "bifurcation" means "branching into two", i.e. for two roots. But some teeth have not two, but three roots - in this situation the term “trifurcation” would be more correct, but doctors often still use the word “bifurcation” as a more common concept. Moreover, bifurcation does not occur on any tooth, but on multi-rooted ones - molars have two or more roots (“sixes”, “sevens” and “eights”).
Is it necessary to treat bifurcation?
In fact, when a dentist talks about tooth bifurcation, he means not only the area of root branching itself, but also the pathological processes occurring here. But there should be a clarification here. For example, perforation in the bifurcation area - i.e. the formation of a hole that violates the integrity of the tooth. This pathology not only causes complications (pulpitis, inflammation of the bone socket, etc.), but often calls into question the very existence of the tooth. Therefore, treatment of perforation or other pathologies in the area of root branching should begin as early as possible.
On a note! If there is perforation in the bifurcation area, the tooth is quite difficult to treat and will not last more than 3-5 years, after which it will have to be removed. Such a tooth is not suitable for a prosthesis, since it can no longer withstand increased chewing loads.
General information
In dentistry, bifurcation refers not only to the area of root branching, but also to the pathological processes occurring in this area. Thus, perforation in the bifurcation zone is fraught not only with pulpitis, inflammation of the bone socket, etc., but also with extraction of the unit.
Treatment of perforation and other pathologies in the furcation zone should be carried out in the early stages of problems. This is due to the complexity of measures that extend the service life of the unit to 3–5 years. Installing a prosthesis on a tooth that is perforated in the bifurcation zone is not advisable, since it is not able to withstand excessive chewing loads.
Why problems arise
Involvement of the furcation area in the pathological process occurs in two cases:
- infection penetrates from the outside (through the gum or bone): normally, the furcation area is in close contact with the periodontium and the bone walls of the tooth socket. But if the bone begins to sag (which happens with periodontitis, periodontal disease), then the furcation area becomes accessible to microbes from the external environment. Also, inflammation of the bone (for example, when an infection enters it through the bloodstream) leads to the “melting” of dental tissue. Over time, the root cement is destroyed, a hole appears in the tooth, and microbes penetrate into the pulp,
- from inside the tooth: for example, with pulpitis or perforation of the bottom of the pulp chamber (during drilling or passage of root canals), which is located just above the furcation area. In this case, microbes from the oral cavity penetrate into the bone socket, causing its inflammation.
Retrograde root canal filling
Indications for retrograde filling:
1. Poorly sealed root canal with phosphate cement, resorcinol-formalin paste or other materials that make re-treatment impossible.
2. Poorly sealed root canal and the presence of a metal object in it: a) stump insert; b) anchor pin; c) fragments of an endodontic instrument.
3. Obliteration of the root canal.
4. Extremely long and curved root canal when conventional endodontic treatment is impossible or unsuccessful.
5. Canals with apical deltas or funnel-shaped expansion.
6. The presence of metal-ceramic or other crowns or fixed structures in combination with the above conditions.
| A root apex resection operation was performed. A control photograph was taken after 3 months. The inflammatory process has been stopped. The tooth is saved! Leaky sealed canals of 12, 11, 21 and 22 teeth. Radicular cyst, core inlay of tooth 12, metal-ceramic crowns. | 2 years after retrograde filling with Trioxident cement. The cavity is filled with newly formed bone tissue. Teeth saved! In most cases, doctors would recommend such teeth to be removed and then made with a removable denture. |
What symptoms should you pay attention to?
In many people, pathology in the area of branching of dental roots is asymptomatic. But some patients note the following signs:
- pain when biting and pressing,
- darkening of the enamel,
- bad breath,
- unsteadiness of an artificial crown or bridge,
- discharge of blood or ichor from under the gums.
Read on the topic: why a tooth hurts “without a nerve” - and how to remove the pain, advice from a dentist.
How is diagnostics carried out?
Diagnosis of the pathological process in the area of bifurcation of tooth roots includes several studies. An X-ray examination is required - computed tomography, which shows the smallest changes, is more informative here. The dentist also probes the gum pocket (normally, the gums should not move away from the tooth by more than 3 mm).
It is important to know! If necessary, the artificial crown is removed or the old filling is removed and the dental cavity is examined for the presence of perforations. It is optimal if the doctor uses a microscope during such an examination - after all, with multiple magnification, you can see the smallest defects.
If pathology in the bifurcation area occurs during treatment, the dentist should pay attention to the appearance of blood in the cavity. In this case, we can speak with 99% certainty about perforation, which needs urgent restoration.
Cystectomy with root apex resection and retrograde filling
cysts (epithelial, non-epithelial) are cavities formed in tissues and filled with one or another liquid content.
Cysts are the most common benign tumor-like formations of the jaws, which usually have to be distinguished from each other, as well as from the cystic form of adamantinoma, fibrous dysplasia or eosinophilic granuloma of the jaw, etc.
In the example below, tooth-preserving surgery to remove a large cyst solved the problem even without removing the braces. In this case, resection of the root apices was not required.
| Before treatment. An extensive radicular cyst in the area of the roots of the lower incisors resulted from aggressive orthodontic treatment. | Treatment was carried out without resection of the roots of the teeth through conservative surgery and implantation of osteoplastic material. On an x-ray after 6 months, the inflammatory process was stopped. |
| In this case, there is a large cyst in the area of the roots of the teeth, which causes constant pain in the patient, especially when biting. Most clinics would suggest removing these teeth and then installing implants and new crowns in their place. | The operation of resection of the apexes of the roots of the teeth followed by retrograde filling made it possible to save the teeth on which core inlays and crowns were installed. Everything is saved, the problem is solved. |
| Unfilled canal of tooth 36. The focus of bone destruction is in the area of root bifurcation. Traditionally, such a tooth is recommended to be removed. | Clinical picture after 12 months. After resection of the apex of the problematic root followed by retrograde filling, the focus of bone tissue destruction was restored. The tooth is preserved. |
Modern methods of treatment
When pathology is detected in the area of root bifurcation, a logical question arises: is it worth saving the tooth? Only a dentist can give an accurate answer after a thorough diagnosis, because... There are many determining factors here. It is important to correctly predict the “functionality” of the tooth if treatment is chosen - so that severe inflammation of the gums and bones does not begin (which, by the way, can affect the roots of neighboring teeth).
Therapeutic treatment
Conservative treatment of the bifurcation area is possible if the hole size does not exceed 1 mm, and is most often carried out using the following technologies:
- closing the perforation with special filling materials: these can be glass ionomer cements that absorb moisture - since it is not possible to properly dry the work area. Suitable brands for root canal filling are ProRoot MTA, MTA-Angelus,
- closing the perforation using calcium preparations: they restore the structure of damaged tissues (which mainly consist of calcium),
- reinforcement with metal threads and filling of the hole in the bifurcation area.
In all of the above cases, after restoration of the hole in the bifurcation area, the tooth cavity is closed with a temporary filling, and after 5-7 days the patient comes for a control x-ray to assess the quality of the perforation closure. There may be several such visits. After achieving a positive result (the perforation is completely closed, there is no inflammation near the roots), a permanent filling is installed.
On a note! If the pathology began from the outside, then treating the tooth alone is not enough - you also need to cure all the tissues that surround it (this is called “periodontal”). Treatment of periodontitis is carried out comprehensively - i.e. conservatively and surgically. First, tartar and granulation tissue are removed using curettage, and then regeneration drugs are introduced.
Surgery
If the perforation cannot be closed, or the hole is 1-1.5 mm or more in size, then surgical intervention is indicated1:
- cystectomy: cutting off the root of a tooth is called
- hemisection: in this case, the root is removed along with the adjacent part of the crown,
- complete removal followed by prosthetics.
“During the treatment of pulpitis in the clinic, they “punched” a hole to the bone with a drill. Of course, I didn’t feel it, but the doctor’s face even changed a little. I thought that I would have to remove it, but the filling seemed to fit normally. Although the dentist immediately said that it would not last long, and in 3 years it would have to be removed. But I don’t feel any particular problems yet.”
Andrey, 34 years old, Kirov, review from forum.stom.ru
When the cause of the pathology is inflammation of the bone tissue or periosteum, removal is often required (even along with a section of the bone). The bone volume is replenished with a special graft, and after some time a prosthesis is installed.
Symptoms
In most patients, pathologies in the bifurcation zone are asymptomatic. However, some note discomfort, manifested in the following signs:
– painful sensations during palpation, chewing;
– darkening of the tooth surface;
– unpleasant odor from the mouth;
– loosening of crowns, bridges;
– appearance of ichor from under the gums.
Diagnostics
To identify pathological processes in the bifurcation zone, radiography, computed tomography, and probing of the gum pocket are performed.
To examine the cavity for the presence of perforation, if necessary, remove the artificial crown and old cement.
If pathology occurs during treatment, the dentist pays attention to the appearance of blood in the cavity. It indicates perforation, requiring immediate treatment.
Treatment
When choosing a treatment method, the dentist prevents the development of inflammation of the soft and hard tissues, which can affect neighboring units.
1.Therapeutic method. Conservative treatment in the bifurcation zone is possible if the perforation size is no more than 1 mm. Pathology is treated in the following ways:
– close the perforation using a filling material (glass ionomer cement that absorbs moisture);
– eliminate perforation with calcium-containing preparations that restore tissue structure;
– reinforced with metal threads, cemented holes.
With the above methods, the dental cavity is then filled with temporary material. After 5–7 days, the patient undergoes a control radiography to assess the quality of perforation removal. There may be several such visits.
When a positive result is achieved, permanent cement is installed.
In case of external causes of pathology, the tissues surrounding the problem unit are treated - tartar and granulation tissue are removed using curettage, and regenerating drugs are introduced.
- Operative method. If therapeutic treatment is ineffective or there is a large perforation hole (over 1–1.5 mm), surgical methods are used:
– cystectomy (tooth root is cut off);
– hemisection (the root is removed along with the adjacent tissues of the crown);
– extraction (the tooth is completely removed).
If the cause of the pathology is identified in the periosteum or bone tissue, the lesion is eliminated along with the bone area. The lost volume is replaced with a graft, subsequently installing a prosthesis.