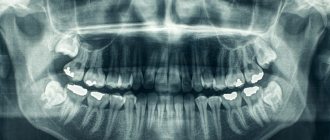
A panoramic photograph of the teeth (orthopantomogram or OTP) is an x-ray of the upper and lower jaw. Allows you to examine most dental problems in detail, conduct high-quality diagnostics and prescribe treatment.
A panoramic dental photograph shows not only the teeth, but also the jaw joints, paranasal sinuses and facial bones. All this makes it indispensable for orthodontic, surgical and reconstructive treatment. You can obtain OPTG using an orthopantomograph.
What is pulpitis?
Dental pulpitis is an inflammatory process that affects the soft tissues located in the dental cavity and causes attacks of acute pain that worsen at night.
Inflammation of the pulp, or in other words, the nerve, most often occurs due to pathogenic microorganisms entering the soft tissues of the tooth. The way microbes enter the pulp is through damaged tooth enamel. The cause of damage can be complications from caries caused by the lack of timely treatment, mechanical damage (chips, fractures, trauma), as well as poor-quality materials used for filling. It is easy to determine tooth pulpitis, because when it appears, it becomes difficult for a person to chew food, a sharp, shooting pain appears when cold or hot liquid comes into contact with the diseased tooth, and frequent wave-like attacks of pain occur at night. Sometimes the patient himself cannot even identify which specific tooth is bothering him, since the pain often spreads to the entire jaw or part of it. Externally, pulpitis can manifest itself as swelling of the gums, bleeding, and even darkening of the color of the enamel.
Dental pulpitis is not only a disease of adults. Many children, especially those of younger preschool age, suffer from this disease. The fact is that baby teeth differ in structure and strength from molars. Their enamel is thinner, the dentin layer is relatively small, but the volume of soft tissue is extensive. Due to this structure, caries destroys baby teeth much faster than molars.
Since pulpitis most often forms on the lower molars, parents do not notice the threat to the health of children's teeth until the baby begins to constantly cry, refuse to eat, or complain of pain. Unfortunately, by this time the signs of pulpitis are already so obvious, and the consequences are irreversible, that the only way out is to remove the diseased tooth.
Doctors distinguish two types of inflammation: acute and chronic pulpitis. Acute begins with a sudden, sharp pain and can affect either a small lesion or the entire mass of the dental pulp. Chronic forms slowly, is not so painful, the unpleasant sensations either fade or return again. Chronic disease is divided into three types: hypertrophic, fibrous and gangrenous pulpitis of the tooth.
What does a panoramic dental photograph show?
The data in the orthopantomogram image is sufficient for the attending physician to see:
- all possible carious lesions of teeth (including those hidden under fillings or on the contact plane of units);
- various malocclusions (congenital and acquired), including occlusion;
- pronounced pathologies of the dentition as a whole and individual units;
- the condition of previously placed fillings (for medical reasons and during an aesthetic dental procedure);
- foci of acute inflammatory processes (including chronic ones);
- dynamics of changes in the dental system during the use of orthodontic structures (braces, aligners, etc.);
- mechanical damage to bone and soft tissues in the oral cavity (for example, due to injuries);
- impact on the gums of removable and conditionally removable orthopedic structures (any dental prostheses);
- various types of neoplasms (shows cysts, granulomas and malignant tumors);
- the number and location of root canals (this information allows you to carry out the procedure for removing nerves and filling canals as accurately as possible);
- condition of the gum bone tissue (especially important before prosthetics and implantation);
- diseases of the temporomandibular joint (for diagnosing arthritis, arthrosis, dysfunction and other pathologies);
- condition (including atrophy) of the alveolar process;
- stage of eruption and position of permanent and milk teeth (buds);
- pathology of the paranasal sinuses;
- position and degree of survival of implants;
- all possible hidden dental diseases.
Also, a panoramic photograph of the teeth is needed to determine the quality of the operations performed. For example, to assess the quality of root canal treatment (to understand whether there are any parts of the instrument, nerves left, and whether there is enough filling material). Such diagnostics are necessary and may be required both during the collection of a clinical picture and at the end of treatment (as a control study).
You might be interested in:
Dental diagnostics
Orthopantomogram of teeth
Pediatric orthopantomogram
Causes
Pulpitis is an inflammatory disease, most often caused by infections. Here are the most common ones:
- streptococci;
- staphylococci;
- lactobacilli.
Getting into microcracks in tooth enamel or into carious cavities, they gradually destroy the surface of the tooth, rushing towards the nerve. In this regard, in addition to treating a damaged tooth, it is often necessary to treat the entire body as a whole, in order to avoid further spread of infection. However, keep in mind that only a specialist can prescribe treatment.
However, the patient may develop pulpitis, the causes of which will not be of a bacterial nature. Let's consider all possible sources of the problem:
| Infectious | Non-infectious |
| • Inflammation when bacteria enter through an area damaged by caries; • Infection through the periodontal pocket formed due to tartar deposits, i.e. pulpitis complicated by periodontitis; | • Mechanical damage to tooth enamel, as a result of which the pulp is also damaged (chips, trauma, tooth fracture - traumatic pulpitis); • Burns or overdrying of the pulp due to unprofessional treatment (the so-called pulpitis under a filling and pulpitis under a crown, appear when the tooth overheats in the absence of sufficient water cooling during drilling of carious areas of enamel or excessive drying of the tooth cavity with a jet of air); • Damage to soft tissue due to strong drugs or filling material. |
What does a radiologist pay attention to when interpreting an orthopantomogram?
For the specialist who interprets and gives a conclusion, a panoramic photograph of the teeth shows a complete picture of the condition of the dental system. Six key points are explored in detail:
- Fabrics _ Both hard (bone) and soft tissues are subject to examination. This allows you to identify all possible inflammations and consequences of mechanical damage.
- Roots of teeth . A panoramic photograph shows not only the condition, location and defects of already formed roots, but also the root follicles. This makes it possible to assess the state of the primordia, predict the direction of their eruption, etc. That is why x-rays of children's primary teeth are no less important than an orthopantomogram for adults.
- Jaws . Timely examination of the individual characteristics of the jaws allows us to identify possible pathologies and defects. In cases where there are problems with the bite, the degree of abnormal development of the dental system is determined so that the correct orthodontic treatment can be prescribed.
- Crowns and fillings . They have a certain shelf life and may lose their functionality over time. In addition, caries can develop under fillings, and inflammation can develop under crowns. A visual examination alone is not enough to determine the location and foci of the disease, so a panoramic photograph of the teeth is required.
- Temporomandibular joint . An orthopantomogram provides complete information about the condition of the joints, clearly showing existing asymmetry, irregular shape and other defects. Panoramic photography is one of the effective ways to diagnose arthritis in the earliest stages.
- Maxillary sinuses (sinuses) . At the same time, the nasal passages and septum are examined. These orthopantomograms make it possible to determine the exact size and features of the outline of the nasal sinuses and identify even the most minimal curvature of the nasal septum. This is especially important in cases where discomfort and pain in the teeth are the result of ENT diseases rather than dental ones. An orthopantomogram of the teeth shows the cavities on the monitor as a darkened area, and the bony/cartilaginous septa as light areas. Modern equipment allows for a fairly high contrast, which makes it possible to notice even the smallest defects and deviations from the norm.
If you still have a question about how to take a panoramic photograph of teeth for adults, ask it at a dentist’s appointment in any of the Smile Factor network of clinics. Our dental orthopantomogram is not only a safe diagnostic procedure, but also the most informative technique that is used before and after treatment in almost all areas of dentistry. What the result of an X-ray examination shows can be seen in 3D on a disk (or sent by email) and in 2D on a printout.
Symptoms
To determine the symptoms and identify the disease, you need to know about the existence of two types: acute and chronic pulpitis. Each of them has different severity of symptoms and speed of development. In acute pulpitis, the symptoms will be as follows:
- pain occurs suddenly and unexpectedly;
- between attacks of pain, while eating or drinking, painful reactions to changes in temperature and increased acidity appear. When the irritants are eliminated, the unpleasant sensations continue for several minutes;
- It is quite difficult for the patient to determine the source of pain, since a large area around the pulpy tooth is often irritated and inflamed;
- at night, as well as simply in a lying position, attacks of acute pain become more frequent, sometimes to such an extent that the patient cannot fall asleep without painkillers and sleeping pills;
- in the absence of timely treatment, the inflammation turns purulent, while the pain intensifies and becomes permanent;
- sometimes accompanied by an acute form of pulpitis and a temperature rising to subfebrile levels.
Chronic tooth pulpitis differs in symptoms from acute pulpitis. Pain is also present, but it is much weaker than in the acute form, aching rather than cutting, and sometimes completely absent. During periods of exacerbation, the chronic form acquires acute symptoms for a short period of time.
In any case, if you have any type of inflammation, you need to contact your dentist as soon as possible. And although chronic pulpitis symptoms are less pronounced than acute ones, its presence can ultimately lead to necrosis of soft tissues and even blood poisoning. Pulpitis of the front teeth is especially unpleasant, since in advanced cases the only treatment option will be to remove the damaged tooth. Subsequently, a person will either have to walk around with a hole in his jaw or spend a lot of money on an implant.
How to recognize pulpitis? Symptoms and signs of the disease
- The first signs of pulpitis are expressed in a painful reaction of the teeth to temperature changes or other irritants.
- Complaints of a sharp toothache, worsening at night, are a sign of already progressing pulpitis.
- Attacks of pain occur on their own, but can appear or intensify when biting, from inhaled air, or from changes in food temperature.
- Very often it is difficult to determine which tooth is affected, since half of the head hurts. With pulpitis of a tooth located in the upper jaw, pain can radiate to the temple, or to the ear - with inflammation of the pulp in the lower jaw.
- When moving from serous inflammation of the pulp to purulent inflammation, the severity of toothache increases. As the purulent process spreads, the toothache takes on a shooting, pulsating, tearing character, and pain-free intervals shorten.
- In the acute form of pulpitis, there may be an increase in body temperature, pain and enlargement of the nearest lymph nodes.
External signs will also help identify pulpitis:
- grayed enamel,
- tooth mobility,
- bleeding,
- redness of the gums,
- the presence of swelling in the area of the diseased tooth,
- formation of a fistula tract.
Untreated acute pulpitis, as a rule, turns into a chronic form, which is characterized by an asymptomatic course or manifests itself in aching pain.
- As a rule, it is characterized by a putrid odor from the mouth.
- Sometimes there is a toothache, aggravated by hot food, and subsided by cold food.
- When visiting a doctor in the chronic form, proliferation of pulp tissue is often diagnosed.
Symptoms of pulpitis may be similar to signs of other diseases (trigeminal neuralgia, periodontitis, etc.), therefore self-diagnosis and self-medication are unacceptable.
What does pulpitis look like in the picture?
Most often, when a patient visits a dentist with acute pain in a tooth, treatment begins with an examination and determination of the type of disease. To begin with, the doctor comprehensively examines the diseased tooth, taps it with instruments, and directs a stream of cold air to identify painful sensations. If there is no visible external damage to the tooth, the patient is sent for an x-ray, based on the results of which a final diagnosis is made and appropriate treatment is prescribed.
The fact is that the pulp is a soft tissue, and X-rays are retained only in hard tissue, resulting in an image. Thus, the image can only reflect a change in bone tissue: a carious cavity, enamel deformation, granuloma or radicular cyst. Therefore, what does pulpitis look like in the picture? Yes, just like a healthy tooth. The only exception is the gangreous type of inflammation, when the death of soft tissue is accompanied by the release of toxic substances beyond the upper part of the tooth root, which provokes slow resorption of bone tissue. Bone density decreases and this is reflected on x-rays.
Based on the above, it is impossible to see pulpitis in the picture. That is, it is possible to distinguish what worries the patient, pulpitis or caries, only by opening the tooth enamel and removing the damaged tissue. However, this does not mean that x-rays will be absolutely useless, because they will help to identify the absence of related problems.
Why do you need a dental x-ray?
Radiation diagnostics is needed in most cases during dental treatment. Without accurate photographs of the oral cavity, the doctor cannot determine the entire affected area and the spread of the disease. Many problems cannot be assessed visually alone, such as nerve damage. X-rays reflect bone tissue well, so this is a very effective technique for examining teeth. Soft tissues also cast a shadow on the photo; using them, the dentist can detect an abscess, cyst or tumor.
Content:
- Why do you need a dental x-ray?
- How it's made
- In what cases is an x-ray needed?
- Where can I do it?
- Examination of children
- X-ray for pregnant and lactating women
- Frequently asked questions from patients
During a visual examination, the dentist can only guess the cause of pain, bleeding or other problems. For an accurate diagnosis, he needs an image of the internal structure of the oral cavity: gums, teeth, roots, canals. The procedure is always carried out before a diagnosis and treatment regimen are made. X-ray examination is necessary not only at the first stage; it is used to determine the effectiveness of therapy.
Be sure to take a series of photographs during cleaning and filling of the canals. They are used to determine the depth of each canal and the tactics for filling it. If the dental treatment is carried out incorrectly, for example, the canal is not completely sealed, this will lead to re-inflammation and various complications are possible, in the form of new dental problems. You cannot do without such technology after prosthetics, complex removal, or treatment of periodontal disease. That is, radiography of the jaw is needed to make a correct diagnosis and to monitor the progress of therapy.
Diagnostics
From the previous section of the article it is clear how to identify pulpitis by symptoms. Now let's look at what diagnostics of pulpitis is and how it is useful. The fact is that in dental practice, many diseases have fairly similar symptoms. This is mainly, of course, pain and inflammation. And differential diagnosis helps the doctor recognize a specific problem.
The main difference between pulpal pain and carious pain will be its behavior when eliminating the irritant. With caries, it will immediately subside as soon as the thermal or other irritant is removed from the mouth, and with pulpitis it will last another ten to fifteen minutes. It is also possible to confuse acute pulpal pain with trigeminal neuralgia, however, with this disease, nocturnal attacks of pain do not appear at all, or are reduced to tolerable.
Another similar inflammation is chronic periodontitis, a characteristic feature of which is painful percussion or tapping on the tooth with an instrument, which is almost pointless to do with pulpitis, since most often the tapping will be painless. In addition, on x-rays, chronic periodontitis will be determined due to the expansion of periodontal cracks.
How is a dental MRI done?
The patient is asked to lie down on a mobile tomograph table, and the head is fixed using bolsters. During scanning, you should maintain the original position of the body, which will avoid the appearance of defects in layer-by-layer images.
MRI procedure on a closed-type tomograph
Headphones provide protection from the noise of the operating device; the patient has an alarm button in his hand, which, when pressed, will pause the study. Medical personnel are located in the next room, and communication with the patient is maintained through a microphone placed in the tomograph tube.
The table with the subject moves into a wide tunnel where a magnetic field generator is installed. The scanning is carried out in three mutually perpendicular planes; based on the obtained images, the specialist can reconstruct a 3D model of the oral cavity and the temporomandibular joint.
When contrast enhancement is used, a series of native photographs are first taken. The study is then paused, the patient is given a gadolinium solution using a catheter connected to an automatic injector, and scanning continues.
An MRI session takes 15 to 20 minutes. When using contrast, the procedure lasts about half an hour.
Complications and consequences
Like any other serious disease, pulpitis complications in the absence of timely treatment can be very unpleasant. The most common of these is periodontitis. It occurs due to the fact that the infection from the inflamed pulp of the tooth gradually spreads to the soft tissue surrounding the tooth, and then the destruction of the jawbone begins. Subsequently, periodontitis can transform into an even more complex and difficult to treat purulent periostitis or osteomyelitis. In addition, chronic foci of inflammation can lead to the spread of infection throughout the body through the bloodstream, and, consequently, provoke diseases of the internal organs, which will lead to a sharp decrease in the level of immunity.
With illiterate or unscrupulous treatment, serious complications are also possible. If the doctor’s actions are not verified and honed to the point of professionalism, when filling the canals of a diseased tooth, the material may get beyond its top or, even worse, voids will remain in the filled tooth.
After treatment of pulpitis of a molar tooth, the pain should gradually fade after the anesthesia wears off. If it does not subside, but on the contrary intensifies, especially in a supine position, we can conclude that the tooth is undertreated. Either there is an unremoved piece of nerve left in it, or the filling was done incorrectly, or a small piece of a dental instrument is stuck in the tooth, which happens in medical practice.
Well, the last, perhaps the most harmless consequence of tooth depulpation for human health is that its tissues wear out over time, the color becomes darker (for example, gray or pink). Over the years, the tooth may begin to decay, so for aesthetic reasons, your doctor may suggest you get a crown on it.
How is this pathology treated?
The key to successful therapy is a thorough diagnosis of periodontitis, which is based on radiographic studies. Treatment of this disease takes place in several stages. In case of exacerbations of periodontitis, it is necessary to first relieve the pain reaction and eliminate inflammation. For this use:
- physiotherapeutic approaches;
- antibacterial therapy to destroy pathogenic microflora.
After this, the root canals of the tooth should be filled. First, to isolate the working area from saliva, SM-Dentistry specialists resort to using a rubber dam system. It ensures the sterility of all manipulations and also does not allow dental preparations to enter the patient’s oral cavity.
Then you need to remove all areas of dental tissue that are affected by caries. If the degree of destruction of the dental crown is too great, the possibility of its complete removal and subsequent replacement with an implant is considered. Next, the doctor cleans the tooth canal and at the same time tries to give it as even a shape as possible. This will make it easier to install the filling, and will also significantly reduce the risk of developing complications of periodontitis.
The next stage is temporary filling of the dental canal. The doctor places a drug with an antibacterial effect in it and seals it with a seal. The drug remains in the tooth canal for two weeks. During this time, it will penetrate the hard shell of the teeth and destroy pathogenic bacteria in the periodontium. After the infection has been eliminated and the inflammatory process has been suppressed, the temporary filling is replaced with a permanent one, or if the tooth is destroyed by more than 50%, it is recommended to restore the tooth with a crown. For its production, the SM-Dentistry clinic uses modern and high-strength composite materials, and the shape of the filling will correspond to the natural and familiar shape of the tooth for the patient. Quality control of treatment at all stages is carried out using computed radiography.
Prevention
Still, one of the main causes of pulp inflammation was and remains caries, so if you do not want to discover pulpitis sooner or later, prevention should consist of regular visits to the dentist and timely treatment of problem teeth. In any case, preventive examinations every six months will cost you much less than treatment of an acute form of the disease.
Among other things, products containing calcium and fluoride, as well as vitamins, will be very useful for strengthening enamel. Timely adequate treatment and not allowing infections such as tonsillitis to become chronic will also benefit the teeth. To treat problem teeth, contact only trusted doctors, whose results will not have to be redone.
If, despite treating your teeth conscientiously, you encounter pain and inflammation, immediately make an appointment with your doctor, and before visiting the clinic, you can try to relieve the pain with folk remedies. For example, rinsing a diseased tooth with a solution of miramistin or chlorhexidine, as well as warm decoctions of chamomile, eucalyptus and sage, can relieve severe pain for a short time. However, if there is pus in the inflamed area, it is recommended to rinse your mouth only with liquid at room temperature to avoid further spread of the infection. And remember, self-medication or lack of treatment does not lead to good things.
Conservative treatment
For granulomas, conservative treatment is more often used. It consists of mechanical treatment of the root canals. After this, they are filled with temporary healing material - pastes based on calcium hydroxide. After 2-3 weeks, a control image can be taken, and if the inflammation is eliminated, the canals are filled with a permanent material - gutta-percha. A new permanent filling is placed on the crown of the tooth.
There are two treatment tactics depending on the initial condition of the tooth.
1. Treatment of granuloma of a tooth in which the root canals are not filled. In this case, treatment involves the following steps:
- removal of carious tissues, old filling on the crown, if any;
- mechanical treatment of canals - with the help of special tools they expand, the walls are smoothed;
- antiseptic treatment of canals.
Further actions depend on the size of the granuloma. If it is small, up to 3 mm, simultaneous filling is allowed. If the formation is more than 3 mm, then the root canals are filled with temporary paste. It helps the granuloma shrink or disappear completely.
You will have to wear temporary material for no more than 3 weeks. At the end of the period, the doctor will order a repeat x-ray, and if he sees positive dynamics, he will fill the root canals with permanent material. The restoration of the tooth crown is also carried out.
2. Treatment of a tooth in which the root canals have already been filled. In this case, the doctor will first remove the old material. If a tooth has a crown, it must be removed. The root canals must be resealed, and the treatment tactics correspond to those described above: sometimes the installation of a temporary therapeutic filling is required.