According to statistics, the inferior alveolar nerve (IAN) suffers quite often during implantation.
The nerve passing in close proximity to the inferior alveolar process is part of the trigeminal facial nerve, which is responsible for the sensitivity of the facial muscles. Disruption of this nerve during implantation 15-20 years ago was considered a common phenomenon. However, in modern dentistry, the equipment used makes it possible to reduce the risk of damage to the NAS.
Statistics say that only 3% of patients experience a postoperative complication in the form of disruption of the lower branch of the facial nerve. But dental practitioners are sure: more than 30% of people become victims of neuropathy, while about 15% of patients remain with this diagnosis forever.
Probability of occurrence
The mandibular nerve fascicle is a fragment of the trigeminal nerve. It provides sensitivity to intraoral and facial tissues, and is responsible for contraction of the facial muscles and dentofacial apparatus. The bundle consists of motor and sensory fibers and nuclei.
The inferior alveolar nerve (IAN) is located in the lower jaw and is one of the three endings of the trigeminal nerve. The NAN borders the root system of the mandibular arch. In this regard, there is a high risk of damage during dental treatment.
The statistics of nerve damage are especially high during the period when dental operations were performed without the use of modern technologies.
According to the latest data, the incidence of nerve damage during dental implantation does not exceed 3%. Of this number, only 1.7% end up with permanent neuropathy.
According to some dentists, these data are underestimated, and the percentage of damage to NAS reaches 30%. In any case, this issue should be given sufficient attention.
Factors influencing neurological response to nerve injury
— Preoperative screening for neuropathic pain is necessary. Preexisting neuropathic dental pain (PDAP type 1), which exists before surgery, can be caused by many different systemic conditions, medications, and other lesions. It is critical that surgeons recognize presurgical neuropathic conditions because neuropathic pain does not respond to surgery and can often lead to worsening pain. In addition, poorly controlled preoperative pain and nerve damage can cause chronic postoperative pain.
— The main indicators for predicting chronic post-surgical pain are psychological factors, including the level of anxiety, neuroticism (a fundamental personality trait in psychology, characterized by anxiety, fear, rapid mood swings, frustration and a feeling of loneliness. It is believed that neurotic people cope worse with stress and are prone to exaggerate the negative side of a particular situation.), catastrophization and introversion. Thus, the doctor has the opportunity not to perform the surgery of choice (implantation) in such patients, but to decide in favor of an alternative treatment plan.
- The concentration of the anesthetic used is up to 2% lidocaine - the accepted standard, because higher concentrations have a greater neurotoxic effect, which may cause permanent neuropathy. Avoid using multiple (repeated) anesthetic blocks in the same area for the same reason.
— Preoperative medical examination should exclude the following diseases : Raynaud's disease, Erythromelalgia (Mitchell's disease), Irritable bowel syndrome (IBS), Migraines, Fibromyalgia.
—Location of surgery is another factor associated with neurological response. Trauma in the distal jaw is more significant (eg, angle and ramus) than in the mental foramen, because the closer the proximal nerve injury is, the greater the risk of damaging trigeminal ganglion cells and initiating retrograde effects of differentiation into the central nervous system. .
Thus, a thorough interview and examination of the patient, detailed pre-implantation planning based on CBCT data, appropriate visualization of the implantation plan and the use of surgical guides, selection of optimal implant sizes with extended safety zones, use of drill limiters and, of course, an experienced team of doctors who will carry out the implantation followed by early postoperative care, all of which will contribute to safer practice and optimized patient outcomes.
First symptoms
Clinical signs of damage to the mandibular nerve are expressed in discomfort in the area of innervation: the area of the mental foramen, the lower lip, the membrane of the gums and cheeks to the borders of the second molar.
Pathology is expressed:
- Paresthesia – change in sensitivity (no painful sensations during injection, etc.).
- Dysesthesia is a change in sensitivity that brings discomfort (pain, “pins and needles”).
- Anesthesia – complete loss of sensitivity.
When extracting wisdom teeth, the lingual nerve is most often damaged (up to 2.1%). During implantation, damage to this nerve is less common and manifests itself with the following symptoms:
- increased salivation;
- speech defects;
- involuntary tongue biting;
- problems with swallowing;
- loss or change in taste;
- burning sensation of the tongue;
- numbness of the mucous membrane of the tongue and gums.
Up to 90% of lingual nerve injuries heal on their own within 7-10 weeks of onset.
Classification of manifestations
According to Seddon's classification, injuries to the trigeminal nerve are of several types:
- Neuropraxia. The damage is reversible. The sheath of the nerve fibers is not affected. There is no degeneration. Sensitivity returns a few weeks after treatment.
- Axonotmesis. Requires long-term therapy for up to six months. Fiber damage occurs and degeneration develops. The damage is reversible.
- Neurotmesis. Nerve structures, fibers and connective membranes are affected. Scars form. The pathological process is irreversible. Surgery is required.
According to the WHO classification, there are five categories of NAS lesions:
- compression or traumatic injury;
- edema;
- gap;
- final break;
- post-traumatic fibrosis.
Assessing the complexity of a clinical situation
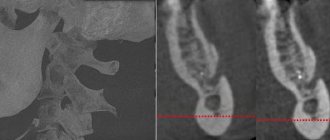
To diagnose neurological pathologies, two research methods are used:
- Mechanoceptive. The tissue response to mechanical action and stimulation is recorded.
- Two-point irritation.
- Brush test.
- Nociceptive. Determine the perception of pain.
- Using a pin.
- Temperature test.
You can determine a taste deficiency by using a cotton pad with sugar or salt.
Research is carried out simultaneously on the affected and healthy sides of the maxillofacial apparatus.
Symptoms are documented. Areas of neurosensory deficit are measured with an accuracy of 1 mm.
Therapy concept
Medical tactics for pain and discomfort:
- Monitoring the patient and tracking the dynamics of the condition over a certain period of time.
- Drug therapy. The use of painkillers, hydrogen pump blockers, glucocorticosteroids and other drugs.
- Removing or unscrewing the rod several turns. It is carried out within 24 hours after implantation. The critical period of treatment is three months. It is during this period that improvement should occur.
- Carrying out a microsurgical operation.
There are no strict treatment protocols. The doctor selects the best option based on practical experience and knowledge.
It is generally accepted that the clinical result of the operation is achieved only if it is performed within a year after implantation.
Surgery
Indications for the operation:
- Confirmed nerve damage.
- Persistent sensory impairment for three months.
- Pain due to a pinched nerve.
The result of surgery depends on certain factors:
- Time elapsed from injury to surgery.
- Type and severity of manifestations.
- Features of blood supply in the pathological zone.
- Proper selection and preparation of the rod.
- The general health of the patient.
- Age.
- Presence of tension zones.
- Experience and practical skills of the surgeon.
Speed of diagnosis is key. Especially with minor damage. Late diagnosis threatens the formation of carpal tunnel syndrome.
Post-traumatic sensory nerve damage. Terminology.
The Association for the Study of Pain has standardized a nomenclature system that defines the most commonly used neurosensory descriptive terms Classification of Chronic Pain, Second Edition: International Association for the Study of Pain Task Force on Taxonomy, ed.: H Merskey and N. Bogduk. IASP Press IASP Council in Kyoto, November 29-30-2007.
- Paresthesia is a non-painful altered sensation. May be described by patients as a pins and needles, slight burning or tingling sensation. NEW sensations - stretching, pulling sensations.
- Dysesthesia is perverted sensations. Abnormal, sometimes unpleasant sensations experienced by a person with partial damage to sensory nerve fibers when touching the skin. - Unpleasant abnormal sensation, spontaneous or provoked. Note : Dysesthesia is not pain when it hurts or paresthesia. Special cases of dysesthesia are hyperalgesia and allodynia. Dysesthesia should always be unpleasant , and paresthesia should not be unpleasant, although it is recognized that the boundary can create some difficulties when it comes to whether these sensations are pleasant or unpleasant. It should always be stated whether the sensations are spontaneous or provoked.
- Neuropathic pain (IASP) is pain caused by damage or disease of the somatosensory nervous system.
- Neuropathy (IASP) is a dysfunction or pathological change in a nerve: in one nerve - mononeuropathy; in several nerves - mononeuropathic multiplex; if diffuse and bilateral - polyneuropathy. Note : Neuritis is a special case of neuropathy and is currently a term reserved for inflammatory processes affecting the nerves. - sensitive (touch, heat, pain) - motor (movement).
- Allodynia is pain from non-noxious stimuli (pain with light touch/cold/heat). The appearance of pain in response to a stimulus that does not cause pain in healthy people. Thermal allodynia, especially cold allodynia, is a feature of the extraoral dermatome in patients with IANIs. Some patients report decreased taste and heat sensitivity. Perversion of sensitivity is characterized by an increased threshold of sensitivity and increased duration of perception, lack of precise localization of sensations of an unpleasant nature, and a tendency to irradiate. The pain continues when the stimulus is removed.
- Hyperalgesia - increased sensitivity to painful stimuli
- Anesthesia - numbness
- Hyperesthesia and Hypostesthesia are terms that are often used to describe changes in sensitivity that increase or decrease, respectively.
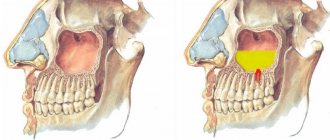
Rice. 5 Anatomy of the II (maxillary) and III (mandibular) branches of the trigeminal nerve. It is important to note that the branches of the superior alveolar nerve retrogradely “merge” into the infraorbital nerve, which explains the symptoms of swelling and pain in the infraorbital region when the superior dental plexus is damaged.
Post-traumatic sensory neuropathy is pain that develops after medical intervention (surgery, treatment, anesthesia), with a minimum duration of 2 months, while other causes of pain are excluded (infection, persistent malignancy, misdiagnosis, etc.), preoperative pain from others must also be excluded reasons.
It is important to add that the neuropathic area does not have to be clearly indicated by the patient, however, about 80% of patients can localize and indicate the neuropathic area.
HERE you can read more about the incidence of “phantom toothache” (atypical odontalgia) after endodontic treatment, which is classified as persistent dentoalveolar pain (PDAP type 2) and occurs in up to 3% of cases.
Causes of gum pain
Patients begin to panic, feeling severe pain in the gums after tooth extraction. This happens after 2-3 hours, when the anesthesia wears off. However, physiologically everything is fine.
The free space left after extraction is called a socket. It initiates healing processes, accompanied by active hematopoiesis and osteoregeneration.
Longer and more painful healing may be due to the following circumstances:
- the further away the problematic tooth was located, the more unpleasant the patient’s sensations;
- tooth extraction was carried out in parts, for example, due to severe destruction of the crown or irregularly shaped roots;
- During the removal process, additional washing of the hole was required due to the discovery of a granuloma (suppuration of the apical part of the root).
Any complex extraction is fraught with errors, which can lead to complications and long-term pain in the gums.
Removal of tooth nerve with arsenic
Removing pulp using arsenic is considered an outdated treatment method, which is almost never used today. The procedure was quite simple: the tooth was prepared using a drill, then the root canals were expanded, medicine was applied to remove the nerve in the tooth, after which a temporary filling was installed for 2 - 3 days. The negative side of such treatment is that arsenic is a strong poison that has a detrimental effect on both the tooth and the tissues surrounding it. With the advent of new safe techniques, the need for arsenic has disappeared.