Condylomas of the penis and foreskin are the result of infection with the human papillomavirus, which is expressed in the pathological proliferation of epithelial cells in the form of papillae on the mucous surface of the penis. Genital warts are contagious and can develop into genital cancer, so they cannot be left untreated.
Appointment with a urologist - 1000 rubles. Comprehensive pelvic ultrasound - 1000 rubles. Appointment based on ultrasound or test results - 500 rubles (optional)
CLICK TO MAKE AN APPOINTMENT or ultrasound tests
Causes of condylomas on the penis
The content of the article
You can become infected with the virus only through sexual contact (not only genital, but also oral and anal); it is extremely rare that the infection is transmitted through household means.
At first, the virus does not manifest itself and can remain dormant for years. The appearance of condylomas is facilitated by a decrease in immunity caused by other diseases: influenza, ARVI, gastritis, STIs, stress, climate change, etc. Also, condylomas grow with changes in hormonal levels associated with male menopause and other reasons. When multiple genital warts appear, the urologist diagnoses “condylomatosis.”
Why are genital warts dangerous for men?
The appearance of condylomas is caused by HPV strains No. 6, 11, 16, 18, 30, 42-45, 51, 52 and 53, accounting for about 2% of all types of papillomavirus. Moreover, it is these strains that are oncogenic and cause cancer in more than half of the cases. The most dangerous of them are types 6, 11 (to a lesser extent), 16 and 18.
In addition to oncology, condylomas cause other troubles:
- Psychological trauma
. Men are embarrassed by sexual diseases and are afraid of injuring tumors, so they restrain sexual activity. - Infection
. Condylomas come into contact with underwear, causing injury, and the same thing happens during washing. The infection easily penetrates the wounds, leading to inflammation. - Inflammation of the prostate
. Decreased sexual function leads to stagnation of secretions in the prostate and prostatitis.
Other complications are possible and are described below.
How does condyloma of the penis and foreskin develop?
The development of genital warts in men is more difficult to detect than in women. The virus has a long incubation period ranging from several weeks to 3 years, lasting an average of 2-3 months. First, it travels throughout the body through the bloodstream and inserts itself into the DNA of the cell, disrupting its division. Only at the end of the incubation period do the affected epithelial cells come to the surface in the form of pointed growths on the mucous surfaces of the genital organ.
A sick person is quite capable of infecting his sexual partner with dangerous HPV, even without having any symptoms! Moreover, the presence of HPV in the body does not mean the simultaneous appearance of condylomas. According to scientists, one or another strain of the virus is present in 62% of all inhabitants of planet Earth, but not everyone is diagnosed with condylomatosis.
The trigger mechanism for the development of the disease is external factors.
These include:
- injuries to the surface of the skin on the genitals (fissures of the anus, microtraumas of the frenulum);
- weakened immunity due to the presence of another disease (flu, hepatitis, pneumonia, etc.)
- stress and depression, which reduce the body's defenses;
- passion for saunas, cedar barrels and other types of overheating of the genitals;
- hypothermia;
- various infections (ureaplasmosis, pyelonephritis, trichomoniasis);
- frequent visits to solariums or prolonged exposure to the sun.
How does HPV, which causes condylomas on the genitals in men, manifest?
The first alarming thoughts arise when a man discovers skin growths on his genitals that look like cauliflower inflorescences or small papillae. In homosexuals, condylomas also appear around the anus. They are also localized on the scrotum, frenulum, and at first do not cause concern. But over time, the tumors gather in groups, itch and cause microtrauma.
Depending on how strong a person’s immunity is, the human papillomavirus has four stages of development. Stages of development of condylomatosis:
- Incubation period
. Lasts from several weeks to several years. The disease does not manifest itself in any way; it can only be detected by PCR analysis. - Initial stage
. On the head of the penis and foreskin, single papillary-shaped neoplasms are noticeable, matching the color of the skin. They do not cause pain or discomfort. If the immune system is restored and the patient undergoes treatment, the condylomas disappear on their own. Many men do not want to hope for a miracle and turn to a urologist to remove tumors. - Chronic form
. Condylomas merge into groups resembling cauliflower inflorescences. The affected areas are itchy and make urination or sexual intercourse difficult. Here it is definitely necessary to remove condylomas. - Launched form
. Condylomas have affected nearby areas of healthy tissue, which dies, rots and emits a foul odor. Any mechanical trauma to the tumor leads to the degeneration of the epithelium into cancer cells. There is no way to do this without surgery.
Manipulation technique
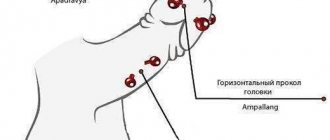
In medicine, two directions of correction of the frenulum of the genital organ are used:
- frenulotomy, dissection of the connecting tissues of a previously intact frenulum;
- frenuloplasty, restoration of the length of the frenulum when a scar forms after its rupture.
The manipulation technique involves dissecting the tissues of the frenulum in the transverse direction, followed by stitching them longitudinally, increasing its length. The operation is performed using local anesthetics and takes no more than a quarter of an hour; the patient remains under observation for about half an hour, after which he is sent home. The period of complete recovery takes from two weeks to a month.
Immediately after the operation, no extraneous sensations are observed; during the next 24 hours after the intervention, some discomfort and pain persist:
- this is due to the presence of a wound surface that comes into contact with urine when the bladder is emptied;
- as well as during spontaneous erection at night, when, with an increase in the size of the organ, tension occurs in the unhealed tissues.
After healing, a neat suture remains, which runs along the lower zone of the organ. Restoring the length of the frenulum allows you to fully and painlessly open the head, without causing pain and discomfort during erection and sexual intercourse.
Symptoms and diseases of the frenulum of the penis:
- Rupture of the frenulum of the penis
- Removal of the frenulum of the penis
- Growths on the frenulum of the penis
- Soreness of the frenulum of the penis
- Papillomas on the frenulum of the penis
- Rash on the frenulum of the penis
- Itching of the frenulum of the penis
- Frenum of the penis
- Inflammation of the frenulum of the penis
- Swelling of the frenulum of the penis
How is condylomatosis transmitted and how to protect yourself from it?
There are three common ways of transmitting HPV, which leads to the appearance of condylomas on the male genital organ.
- Unprotected sexual contact and protected sex with a sick partner
. Even using a condom does not protect 100% from the virus. During sexual intercourse, cells of the affected epithelium penetrate the mucous tissues of a healthy partner, and this is the most common method of infection among people 18-35 years old. - During childbirth from mother to child
. The baby is born already infected, and neoplasms on the child’s penis can be seen already in the first year of life. - Contact and household method
. This happens extremely rarely, mainly in conditions of lack of sanitation (when using one razor, a shared towel or comb) and only if there is microtrauma on the surface of the skin.
A person can be a carrier of HPV, but he or she will not develop condylomas until the carrier of the virus has a weakened immune system. In this case, the affected epithelium will begin to multiply atypically (with the formation of cells unusual for this tissue), forming condylomas on the surface.
Condylomas pose the greatest danger to women, in whom in 99.9% of cases the disease is the cause of cervical cancer, therefore, upon learning about your disease, you must definitely warn your partner. Girls who are promptly vaccinated with the Gardasil vaccine against HPV have a lower risk of infection. By the way, this vaccination is also given to young men.
Causes
Genital warts in men on the penis can appear due to the following reasons:
- Lack of protection during sexual intercourse.
- The presence of microcracks in the skin and mucous membranes in the genital area.
- Weakening of the immune system.
Men who are sexually active are the first to fall victim to HPV attacks. Warts on the penis are more likely to appear on the penis of members of the male population who are gay or who welcome promiscuous sexual relations without the use of protective equipment. You should not include only men who are into sexual excesses into the risk group. Respectable family men are also susceptible to infection. If HPV has entered a man’s body, this does not mean immediate infection. For the papillomavirus to begin its attack on a person, he “needs help.” An unfavorable factor in this case may be a weakened immune system. Vulnerability to the entry and spread of infection in the body increases if a man:
- became very cold or overheated;
- leads an unhealthy lifestyle (doesn’t get enough sleep, eats poorly, etc.);
- abuses smoking or alcohol;
- suffered from any serious illness;
- is in a constant state of stress.
Complications of condylomatosis: genital warts are very dangerous!
If you ignore tumors on the genitals or glans, the following problems will arise:
- Spread of condylomas to the urethra
. They block the urethra, leading to inflammation and viral urethritis. - Viral infection of the rectum
leads to the formation of paraproctitis, which interferes with bowel movements, causes severe pain, bleeding, and is difficult to treat. - The exophytic nature of condylomas
is that they grow inside the organ. - Condyloma has the ability to degenerate into a cancerous tumor
. With reduced immunity, the virus that infects the epithelial cell (the upper layer of the skin) begins to produce new cells that differ in structure from the maternal one (atypical). This is how condyloma degenerates into cancer. - Condylomas have an unaesthetic appearance
, causing disgust in the partner. A man may experience psychological and even physical discomfort during sexual intercourse, which significantly reduces the quality of sexual life. - Men suffering from diabetes mellitus have wide lesions of the foreskin, and their inguinal lymph nodes become inflamed.
- Phimosis
develops - the inability of the foreskin to expose the head of the penis. - In advanced cases, pus accumulates around condylomas, and the patient experiences unbearable pain.
- Condylomas located at the opening of the urethra impede the passage of urine and cause general intoxication of the body, which leads to decreased vitality, drowsiness, poor health, and depression.
In 100% of cases, the patient’s regular partner also becomes infected with HPV.
Preparing for treatment
Before starting treatment for papilloma, the doctor conducts a thorough examination of the man’s groin under magnification, makes a diagnosis, and studies tests.
The effectiveness of treatment depends on the correct diagnosis:
- Oral interview with a venereologist, taking an anamnesis.
- If the head of the penis, urethra or urethra is affected, consultation with a urologist is indicated.
- You need to be tested for HPV using the PCR method (scraping from the genitals), for AIDS, HIV and syphilis.
- Examination of the anus by a proctologist.
- Getting tested for STDs.
After all the tests are ready, the doctor will select the appropriate method for treating and removing papillomas for the man. Tumors can be removed only if the man does not have infectious or viral diseases in the acute stage.
How are condylomas of the penis and foreskin diagnosed?
There are various diagnostics aimed at identifying the presence of HPV in the human body, as well as the oncogenicity (ability to produce cancer cells) of condyloma. The most common methods for identifying genital warts:
- Visual examination of the genitals and anus by a urologist or dermatologist
. To visualize atypical cells, the doctor covers the condylomas with acetowhite rayon, and the oncogenic cells are stained against the background of unstained healthy epithelium. - Biopsy
. This is a sampling of tumor tissue to determine its cellular composition. The most dangerous are strains 16 and 18, which degenerate into cancer cells; - Polymerase chain reaction test
, which uses biotechnology to detect DNA and RNA of a virus foreign to the body. This method can confirm the presence of human papillomavirus, but does not determine whether the cells are cancerous or degenerating. - Tests for HIV and tests for sexually transmitted infections. Condylomas appear when immunity decreases, and, in parallel with HPV, other infections can develop in the body;
- Test - urethroscopy.
If neoplasms are suspected, an internal examination is performed on the urethra.
Methods of diagnosis and therapy
Diagnosis of neoplasms begins with the collection of complaints (when and under what circumstances did condylomas appear) and a visual examination by a doctor (urologist, dermatovenereologist) of the injury sites (what do condylomas on the penis look like). If a human papillomavirus is suspected, the following examinations are prescribed:
- General tests (blood, urine) to assess the patient’s general health and determine infectious and chronic diseases.
- Tests for syphilis and HIV infection.
- PCR diagnostics (scraping or smear from the urethra, urethra) - determines the presence of the virus in the body and its prevalence, allows you to identify sexually transmitted infections.
- Biopsy and histological examination of a fragment of the neoplasm to determine the malignancy of the process.
- Genotyping is a laboratory determination of the type of virus or a combination of several.
- Urethroscopy - to examine changes in the urethra.
- Anoscopy is an examination of the anus (perianal area) under magnification (if there are lesions around the anus).
- Digene test - determines the concentration (quantity) of the virus and oncogenic risk. The mucous membrane of the urethra, the lining of the urethra and the head of the penis are scraped.
- Immunogram - diagnoses disorders of the immune system and the possibility of correcting them.
Diagnosis of genital warts involves tests and hardware examination methods on the recommendation of a doctor. Depending on the results of the research, the extent of damage to the penis and surrounding tissues by condylomas, the doctor chooses a therapeutic tactic. Medication, destructive and combined methods of therapy are used. It is effective to use complex treatment, including removal of condylomas and restoration of the correct functioning of the body's defenses.
Drug treatment
To get rid of viral activity, correct and increase the body's immune defense, drug treatment is used. The negative consequences of such therapy are possible relapses and the manifestation of various side effects. The most effective is combination treatment: the use of drugs, destructive methods that destroy tumors, and the simultaneous use of antiviral and immunomodulatory drugs. The main goal of drug therapy is to increase and correct the body’s immune defense, suppression of viral activity before or after removal of tumors using methods chosen by the doctor.
How is it removed?
Local drug therapy (ointment, acid) is used to remove growths. The drug, dosage and treatment methods are selected by the doctor depending on the nature of the tumors and the patient’s condition. If the effectiveness is insufficient, more radical methods of removing condylomas are used. It is advisable to carry out manipulations in a medical institution. Small growths can be removed at home only after medical consultation. Self-medication and the use of traditional medicine are prohibited. Severe complications may appear in the form of proliferation of the viral process and deterioration in general well-being.
Removal preparations
| A drug | Operating principle | Side effects | Duration of therapy |
| "Kondilin" | Cauterizing effect, necrosis of affected tissues | Itching, peeling, burning, redness, soreness | 2 rubles/day 3 days, 4 days break. Course - 5 weeks |
| "Solcoderm" | Drying, falling off growths | Burning, pigmentation, soreness, scarring | 1 treatment. Repeat after 4 weeks |
| Oxolinic ointment | Drying, causing growths to fall off | Mild burning, itching | 2–3 times a day 1–2 months |
| Trichloroacetic, nitric acid | Destruction and death of affected areas | The appearance of wounds, scars, burns | Once every 7 days 6 weeks |
Surgery for genital warts is prescribed in extreme cases, if other treatment methods do not give the desired result.
Destructive techniques
If condylomas cannot be treated, they must be removed radically. Based on research data and drug therapy, the specialist selects the appropriate way to remove growths. The result of treatment is getting rid of tumors and the external consequences of their growth. Condylomas are removed in the following ways:
| Method | Indications | Description | pros | Minuses |
| Surgical | Removing small areas on external surfaces | It is performed under local anesthesia. The growths are cut off with a scalpel | Availability | Possibility of bleeding, scars, inflammation |
| Electrocoagulation | Removing single growths | Local anesthesia. Electric shock, cauterization | Availability, efficiency | Trauma, scarring, bleeding, long recovery |
| Cryodestruction | Removing spot areas, small areas | Treatment of genital warts with liquid nitrogen, exposure to low temperatures under local anesthesia | Simplicity, no scars, no scars | Possibility of hyperpigmentation |
| Laser exposure | Removal of single and large tumors | Laser beam drying | Accuracy, painlessness, fast healing | Potential for scarring, high cost |
| Radiosurgery | Removal of any types of condylomas | Exposure to radio waves | Accuracy, painlessness, speed of recovery | Price |
Removal of condylomas from the foreskin and glans penis
HPV today is an incurable disease, because there is no medicine that would destroy the virus itself, but relapses are successfully removed. The sooner treatment is started, the greater the chances of getting rid of condylomas.
Treatment methods are divided into surgical and conservative. The latter include:
- Immunotherapy to enhance immunity
. It should be noted that immunostimulants should be taken carefully and only after consultation with a doctor, because they contribute to the development of oncology. Those. If you already have cancer, it will only get worse! Immunomodulators used in the treatment of HPV are of two types: based on interferon-alpha-2 (Altevir, Intron-A, Realdiron) and stimulators of interferon protein production by microphages and lymphocytes (Cycloferon, Arbidol, Amiksin). - The use of ointments that stop the proliferation of condylomas
(Oxolin, Viferon, Aldara cream, Panavir gel, Epigen cream). They are applied to the affected areas of the skin, stopping the further spread of atypical cells, healing tissues and increasing the intracellular production of interferons. - Immunostimulants and ointments
are used as a general course for several months in the initial stages of the disease. Their use is effective only for single small-sized condylomas.
How to remove condylomas of the penis and foreskin
Surgical methods for eliminating condylomas include:
- Electrocoagulation.
An effective, inexpensive, but painful method. It involves applying an electric current to the condyloma, causing it to fall off, leaving a small scar. The method is already outdated. - Cauterization with a solution of acetic and nitric acid
. As a result, the condyloma tissue dies, and it dries out and falls off. Used on separately located large condylomas. The method is not recommended, as surrounding healthy tissue may be damaged, and healing on the penis will take a long time. - Cryodestruction
. This is the effect of ultra-low temperatures of liquid nitrogen on an atypical area, as a result of which condyloma cells change structure and self-destruct. This is a painless method that does not leave scars. But it is effective for small, separately located condylomas. - Laser removal
. The method is painful and requires local anesthesia. Depending on the size of the condyloma, the doctor selects the depth of exposure of the laser beam. It burns out the base of the condyloma, it is deprived of nutrition and falls off, leaving no scar. - Surgical removal
with a metal, argon, plasma scalpel. Used to remove large condylomas located in groups. Requires stitches and long healing. - Radio wave method
. The most modern, effective and painless method. With the help of radio waves of various frequencies, the condyloma is completely excised and disappears. The nearby healthy tissues remain intact, and the patient is left with no scars. The relatively high cost of the method (from 500 rubles per tumor) is dictated by the high cost of complex professional equipment.
Operation methods
There are several ways to perform plastic surgery of the frenulum of the penis, which depend on the anatomical features of the structure of the structural tissue of the foreskin.
Among the main methods, there are two types of surgery:
- Frenulotomy.
Lengthening the frenulum occurs by cutting in the transverse direction followed by longitudinal stitching, which allows you to naturally increase the length of the fabric up to 2 centimeters. With this method, the sensitivity of the genital organ is not affected. - Frenulectomy
. Complete removal of the frenulum, which is required for mechanical injuries of the foreskin and scarring of the tissue. The incision is made transversely around the circumference of the genital organ, followed by longitudinal stitching. The result is a scar that aligns with the natural suture at the bottom of the penis.
Quite often, both methods are implemented without the use of classical surgical instruments. Intervention in the tissue structure is carried out through laser exposure. The technology of the procedure fully complies with generally accepted rules, with the exception of the use of radiofrequency exposure instead of a scalpel; instead of stitching, the edges of the resulting wound are soldered.
The main advantage of using modern equipment is the minimal risk of bleeding during the process and natural disinfection of the wound through exposure to high temperatures.
Answers to frequently asked questions on the topic of the frenulum of the penis:
- Which doctor treats frenulum of the foreskin?
- Where to go with a problem on the frenulum of the foreskin?
- What tests should be taken if there are problems with the frenulum of the penis?
- Diagnosis of diseases of the frenulum of the penis
- Treatment of diseases of the frenulum of the penis
- Is it possible to remove the frenulum of the penis?
- Swollen frenulum of the penis
- Rash on the frenulum of the penis
- Herpes on the frenulum of the penis
- How does the foreskin affect sensitivity?
- How to stretch the foreskin?
- What is the foreskin for?
- Diagnosis of diseases of the foreskin?
- Why doesn't the foreskin open completely?
- What to do if the foreskin is swollen?
- Have plaque appeared under the foreskin?
- Do you perform foreskin plastic surgery at your clinic?
Is it possible to protect yourself from the human papillomavirus?
To date, there is no medicine that would destroy the virus itself. But you can get a vaccination that protects the body from oncogenic strains of HPV. It is advisable to get the vaccine at the age of 9-17 years, and it is effective only for uninfected boys. It is of no use to those who are HPV carriers.
People under the age of 45 can be vaccinated; later it is no longer effective. If you vaccinate an uninfected young person under the age of 26, this will protect him not only from genital warts, but also from oncological processes of the male genital organs.
Currently, the most effective vaccine for men against penile cancer is Gardasil. It protects against oncogenic strains 6, 11, 16, 18, and the Gardasil-9 vaccine will additionally protect against non-oncogenic strains 31, 33, 45, 52 and 58.
The vaccination is done in three stages: the first vaccination is given in the shoulder muscle, the second is given 2 months later, and the third is given several months after the first, depending on age. The drug Gardasil does not contain living or dead viruses, it only contains particles similar to the DNA of the virus. The vaccine also does not contain mercury or the toxic antiseptic component thiomersal. The effectiveness of Gardasil vaccination is 97.9%.
The drug is used in 125 countries of the world, and in 20 of them it is a mandatory item in the vaccination card. It has few side effects, but causes blood thickening, so it is contraindicated for people with bleeding disorders and thromboembolism.
Vaccination may be accompanied by fever and general malaise, but some discomfort is not comparable to the effectiveness of the drug and its ability to protect the body from HPV.
Introduction
Penile warts are the most common sexually transmitted disease in men and are caused by the human papillomavirus (HPV) [1-3].
Penile warts typically present as soft, flesh-colored to brown plaques on the glans and shaft of the penis [4]. To provide an update on the current understanding, diagnosis, and treatment of penile warts, a review was conducted based on a PubMed search using key terms and phrases such as “penile warts” and “genital warts.” The search strategy included meta-analysis, randomized controlled trials, clinical trials, observational studies, and reviews.
Epidemiology
HPV infection is the most common sexually transmitted disease worldwide [4]. In the United States, 50–75% of sexually active people have been infected with HPV at least once in their lives [4, 5]. Infection with HPV does not mean that a person will develop genital warts [5]. It is estimated that 0.5–5% of sexually active young adult men have genital warts on physical examination [6–9]. The peak age of the disease is 25–29 years [7, 10]. Typically, approximately 75% of men who have sexual contact with a partner who has genital warts develop penile warts within 8 months [8].
Etiopathogenesis
HPV is a non-enveloped capsid double-stranded DNA virus belonging to the genus Papillomavirus of the Papillomaviridae family and infects only humans [11]. The virus has a circular genome of 8 kilobases in length, which encodes eight genes, including the genes for two encapsulating structural proteins, namely L1 and L2 [11]. The virus-like particle containing L1 is used in the production of HPV vaccines. L1 and L2 mediate HPV infection [11].
To date, more than 200 types of HPV have been identified, of which more than 100 HPV genotypes have been sequenced [4, 11, 12]. More than 40 types of HPV can be transmitted sexually [4, 11, 12]. HPV can be divided into types depending on the risk of developing cancer: high-oncogenic and low-oncogenic. Approximately 90% of genital warts are caused by low-oncogenic types HPV-6 and/or HPV-11 [2-4, 13]. And for other types (HPV-1, HPV-2, HPV-3, HPV-4, HPV-16, HPV-18, HPV-40, HPV-42, HPV-43, HPV-44, HPV-54, HPV -70, HPV-72 and HPV-81) account for the remaining 10% of infection [14].
It is also possible to become infected with different types of HPV at the same time [8]. In adults, genital HPV infection is transmitted primarily through sexual contact and, less commonly, through oral sex, skin-to-skin, and fomites [8]. In children, HPV infection can occur as a result of sexual abuse, vertical transmission, self-infection, infection through close household contact and through fomites [1, 15]. HPV penetrates into the cells of the basal layer of the epidermis through microtraumas on the skin or mucous membrane [13].
The incubation period of infection ranges from 3 weeks to 8 months, on average 2 - 4 months [12, 16, 17]. The disease is more common in individuals with the following predisposing factors: immunodeficiency, unprotected sexual intercourse, multiple sexual partners, a sexual partner with multiple sexual partners, a history of sexually transmitted infections, early sexual activity, a shorter period of time between meeting a new partner and engaging in sexual intercourse living with him, refusing circumcision and smoking [3, 18, 21]. Other predisposing factors are moisture, maceration, trauma and epithelial defects in the penile region [3].
Histopathology
Histological examination reveals papillomatosis, focal parakeratosis, severe acanthosis, multiple vacuolated koilocytes, vascular distension and large keratohyalin granules [4, 17].
Clinical manifestations
Penile warts are usually asymptomatic and may occasionally cause itching or pain [3, 8, 13]. Genital warts are usually located on the frenulum, glans penis, inner surface of the foreskin and coronal sulcus [3, 8, 13]. At the onset of the disease, penile warts typically present as small, discrete, soft, smooth, pearly, dome-shaped papules [3, 7, 14].
Lesions may occur individually (Fig. 1) or in clusters (grouped) (Fig. 2) [8]. They can be pedunculated or broad-based (sessile). Over time, papules can coalesce into plaques [14]. Warts may be filiform, exophytic, papillomatous, verrucous, hyperkeratotic, cerebriform, fungiform, or cauliflower-like (Figure 33-5). The color may be flesh-colored, pink, erythematous, brown, violet, or hyperpigmented. [4, 23]
Diagnosis
The diagnosis is made clinically, usually based on history and examination. In vivo dermatoscopy and confocal microscopy help improve diagnostic accuracy [24]. Morphologically, warts can vary from finger-shaped and pineal-shaped to mosaic [24 – 26]. Among the features of vascularization one can find glomerular, hairpin and punctate vessels [26]. Papillomatosis is an integral feature of warts [4]. Some authors suggest using the acetic acid test (whitening of the surface of warts when acetic acid is applied) to facilitate the diagnosis of penile warts.
The sensitivity of this test is high for hyperplastic penile warts, but for other types of penile warts and subclinical infected areas the sensitivity is considered low. Skin biopsy is rarely warranted but should be considered in the presence of atypical features (eg, atypical pigmentation, induration, attachment to underlying structures, hard consistency, ulceration, or bleeding), when the diagnosis is uncertain, or for warts that are refractory to various treatments. Although some authors propose PCR diagnostics to, among other things, determine the HPV type that determines the risk of malignancy, HPV typing is not recommended in routine practice [13].
Differential diagnosis
Differential diagnosis includes pearlescent penile papules, Fordyce granules, acrochordons, condylomas lata in syphilis, molluscum contagiosum, granuloma annulare, lichen planus, lichen planus, seborrheic keratosis, epidermal nevus, capillary varicose lymphangioma, lymphogranuloma venereum, scabies ku, syringoma, post-traumatic neuroma, schwannoma, bowenoid papulosis and squamous cell carcinoma [7].
Pearly penile papules
Present as asymptomatic, small, smooth, soft, yellowish, pearly white or flesh-colored, conical or dome-shaped papules with a diameter of 1 - 4 mm (Fig. 6). The lesions are usually uniform in size and shape and symmetrically distributed [27]. Typically, papules are located in single, double or multiple rows in a circle around the crown and groove of the glans penis. Papules tend to be more noticeable on the dorsum of the crown and less noticeable towards the frenulum[27].
Fordyce granules
- these are enlarged sebaceous glands. On the glans and shaft of the penis, Fordyce granules appear as asymptomatic, isolated or grouped, discrete, creamy yellow, smooth papules with a diameter of 1 - 2 mm (Fig. 7) [28 - 30]. These papules are more noticeable on the shaft of the penis during erection or when the foreskin is pulled [28, 30]. Sometimes a dense chalky or cheese-like material can be squeezed out of these granules [28].
Acrochordons
, also known as skin tags (“skin tags”), are soft, flesh-colored to dark brown, pedunculated or broad-based skin growths with a smooth contour (Fig. 8) [31,32]. Sometimes they may be hyperkeratotic or have a warty appearance [33]. Most acrochordons measure between 2 and 5 mm in diameter, although they can sometimes be larger, especially in the groin. Acrochordons can appear on almost any part of the body, but are most often seen on the neck and intertriginous areas [31,32]. When they appear in the penile area, they can mimic penile warts.
Condylomas lata
are skin lesions in secondary syphilis caused by the spirochete, Treponema pallidum [34, 35]. Clinically, condylomas lata appear as moist, grey-white, velvety, flat or cauliflower-like, wide papules or plaques. They tend to develop in warm and moist areas of the genitals and perineum [36]. Secondary syphilis is characterized by a nonpruritic, diffuse, symmetrical maculopapular rash on the trunk, palms, and soles [34]. Systemic manifestations include headache, fatigue, pharyngitis, myalgia and arthralgia [34]. Erythematous or whitish eruptions on the oral mucosa, as well as alopecia and generalized lymphadenopathy may be observed [36].
Typically molluscum contagiosum
presents as discrete, smooth, firm, dome-shaped, yellowish, pearly white or flesh-colored waxy papules with a characteristic central umbilical depression (Figs. 9 and 10) [37-39]. In the pediatric age group, lesions are most often observed on the trunk and intertriginous areas, while in adults, molluscum is most often observed on the lower abdomen, upper thighs and genital area (Fig. 9) [39]. The size of the lesions ranges from 1 to 5 mm in diameter, and the number usually does not exceed 20 [38, 39].
Granuloma annulare
is a benign, self-limiting inflammatory disease of the dermis and subcutaneous tissue. The pathology is characterized by asymptomatic, firm, brownish-purple, erythematous or flesh-colored papules, usually arranged in a ring. As the condition progresses, central involution may be noted. A ring of papules often grows together to form a ring-shaped plaque. Granuloma is usually located on the extensor surfaces of the distal extremities, but can also be detected on the shaft and glans penis [41, 42].
Ringworm
is a chronic inflammatory dermatosis characterized by numerous, asymptomatic, discrete, flat, flesh-colored, shiny, pinhead-sized papules (Figure 11). The most favorite locations are the abdomen, chest, limbs and penis [43 – 45]. The lesions are usually located in groups [43].
Lichen planus of the skin
is a chronic inflammatory dermatosis manifested by flat, polygonal, purple, pruritic papules and plaques (Fig. 12) [46]. Most often, the rash appears on the flexor surfaces of the hands, back, torso, legs, ankles and glans penis [47]. Approximately 25% of lesions occur on the genitals [47].
Seborrheic keratosis
usually presents as an asymptomatic, well-circumscribed, round or oval brownish plaque with a warty surface (Fig. 13). Often the lesions may appear shiny and greasy and are therefore incorrectly called seborrheic (oily) keratoses [48]. Most often located on the face, chest, back and limbs. They are rare on the penis [49]. HPV is found in approximately 70% of seborrheic keratosis cases in the genital area versus 5% outside the genital area [49].
Epidermal nevus
is a hamartoma arising from embryonic ectoderm that differentiates into keratinocytes, apocrine glands, eccrine glands, hair follicles and sebaceous glands. The classic lesion is a solitary, asymptomatic, well-circumscribed plaque that follows Blaschko's lines. The onset of the disease usually occurs in the first year of life. Color varies from flesh to yellow and brown. Over time, the lesion may thicken and become warty.
Capillary varicose lymphangioma is a benign saccular dilatation of cutaneous and subcutaneous lymph nodes. The condition is characterized by clusters of bubbles resembling frog eggs (Fig. 14). The color depends on the content: whitish, yellow or light brown color is due to the color of the lymph fluid, and reddish or bluish color is due to the presence of red blood cells in the lymph fluid as a result of hemorrhage [51]. The blisters may undergo changes and acquire a warty appearance [50]. It is most often found on the extremities, less often in the genital area [52].
Lymphogranuloma venereum
is a sexually transmitted disease caused by Chlamydia trachomatis. The disease is characterized by a transient painless genital papule and, less commonly, an erosion, ulcer or pustule followed by inguinal and/or femoral lymphadenopathy known as buboes [34, 53].
Scabies
In humans, caused by the parasitic mite Sarcoptes scabiei var hominis, it is characterized by burrows, erythematous and papular rashes and intense itching (often worse at night) [54]. Erythematous papules, caused by a hypersensitivity reaction to mites, range in size from 1 to 2 mm in diameter (Fig. 15) [54].
Typically, syringomas
are asymptomatic, small, soft or firm, flesh-colored or brown papules measuring 1–3 mm in diameter [55]. They are usually found in the periorbital areas and on the cheeks [55]. However, syringomas can appear on the penis and buttocks. When located on the penis, syringomas can be mistaken for penile warts.
Traumatic neuromas
are tumors of the nerve sheaths in which the ratio of axons to Schwann cell bundles is approximately equal [56, 57]. This pathology is the result of regenerative proliferation of injured or damaged nerve fibers. Traumatic penile neuromas can result from penile trauma such as circumcision and dorsal penile neurotomy (used to treat premature ejaculation) [56 – 59]. Clinically, traumatic penile neuromas present as skin-colored or erythematous papules or nodules on the glans or shaft of the penis [56 – 59].
Schwannomas
- These are neoplasms originating from Schwann cells. Schwannoma of the penis usually presents as a single, asymptomatic, slowly growing nodule on the dorsal side of the penile shaft [60, 61].
Bowenoid papulosis
is a precancerous focal intraepidermal dysplasia that usually appears as multiple red-brown papules or plaques in the anogenital area, particularly the penis [62]. The pathology is consistent with squamous cell carcinoma in situ. Progression to invasive squamous cell carcinoma occurs in 2–3% of cases [62].
Typically squamous cell carcinoma
penis manifests itself as a nodule, ulcer or erythematous lesion [63]. The lesions may appear warty, leukoplakia, or sclerosis [63, 64]. The most favored site is the glans penis, followed by the foreskin and shaft of the penis [63].
Complications
Penile warts can be a cause of significant concern or distress for the patient and their sexual partner due to their cosmetic appearance and contagiousness, stigmatization, concerns about future fertility and cancer risk, and their association with other sexually transmitted diseases [65, 66]. ]. It is estimated that 20 – 34% of affected patients have underlying sexually transmitted diseases. Patients often experience feelings of guilt, shame, low self-esteem and fear [67]. Individuals with penile warts have higher rates of sexual dysfunction, depression, and anxiety compared to the healthy population [65, 68]. This condition can have a negative psychosocial impact on the patient and negatively affect their quality of life. Large exophytic lesions may bleed, cause urethral obstruction, and interfere with sexual intercourse. Malignant transformation is rare, except in immunocompromised individuals [74, 75]. Patients with penile warts are at increased risk of developing anogenital, head and neck cancers as a result of co-infection with high-risk HPV [4,76].
Forecast
If no treatment is given, genital warts may resolve on their own, remain unchanged, or increase in size and number [3]. Approximately one third of penile warts regress without treatment, and the average time until they disappear is approximately 9 months [4, 77]. With proper treatment, 35 to 100% of warts disappear within 3 to 16 weeks [65]. Although warts resolve, HPV infection may persist, leading to recurrence [4]. Relapse rates range from 25 to 67% within 6 months after treatment [7, 78]. Among patients with subclinical infection, recurrent infection (reinfection) after sexual intercourse, and those with immunodeficiencies, a higher percentage of relapses occurs [72].
Treatment
Active treatment of penile warts is preferable to follow-up because it leads to faster resolution of the lesions, reduces fears of infecting a partner, relieves emotional stress, improves cosmetic appearance, reduces social stigma associated with penile lesions, and relieves symptoms (eg, itching, pain or bleeding) [3, 7, 77]. Penile warts that persist for more than 2 years are much less likely to resolve on their own, so active treatment should be offered first [14]. Counseling of sexual partners is mandatory. Screening for sexually transmitted diseases is also recommended.
Active treatments can be divided into mechanical, chemical, immunomodulatory and antiviral [80]. There are very few detailed comparisons of different treatment methods with each other. Effectiveness varies depending on the treatment method. To date, no one treatment has been proven to be consistently superior to other treatments. The choice of treatment should depend on the physician's skill level, patient preference and tolerance to treatment, as well as the number of warts and the severity of the disease. The comparative effectiveness, ease of administration, side effects, cost and availability of the treatment should also be taken into account. In general, self-administered treatment is considered less effective than self-administered treatment [6].
The patient carries out treatment at home (as prescribed by the doctor)
The therapy prescribed to the patient includes podofilox solution or gel (0.5%), imiquimod (3.75% or 5% cream) and 15% synecatechin ointment (Polyferon E) [13, 80, 81].
Podofilox 0.5% solution or gel is derived from podophyllotoxin, a plant resin that, during cell division, destroys microtubules at the time of replication. This stops mitosis and causes tissue necrosis. Thus, podofilox has been shown to be effective in the treatment of penile warts [79, 82]. Podofilox solution or gel (0.5%) is applied topically twice daily for 3 consecutive days, followed by a four-day break. Can be used at home [7]. The weekly cycle can be repeated up to four times [7]. The effectiveness of wart removal ranges from 45 to 77% [7]. Side effects include local discomfort, itching, irritation, burning, pain, xerosis, erythema, erosion, ulceration and post-inflammatory hyperpigmentation or hypopigmentation at the application site [7, 14]. To minimize local side effects, podophyllotoxin should be washed off 1 to 4 hours after application. Sexual contact should be avoided while podophyllotoxin is still on the skin [79].
Imiquimod is available as 3.75 and 5% cream. Imiquimod enhances the host innate and cellular immune response and combats HPV by binding to skin dendritic cells and macrophages through toll-like receptors [7, 9]. This leads to the synthesis and release of pro-inflammatory cytokines such as interferon alpha (IFN-α), tumor necrosis factor alpha (TNF-α) and interleukins: IL-1, IL-6, IL-8 and IL-12 [7, 79]. Secreted cytokines stimulate local immune effects that are toxic to HPV. Imiquimod also acts on cellular immunity by activating Langerhans cells, thereby increasing the presentation of antigens to T cells. Studies have shown that topical application of 5% Imiquimod cream is beneficial in the treatment of penile warts [83]. 5% imiquimod is applied three times a week until the lesion is completely removed or for 16 weeks, while 3.75% imiquimod is applied daily in the evening for 8 weeks [9, 79]. The effectiveness of wart removal is similar to podofilox [7]. Side effects of topical imiquimod include local irritation, itching, burning, erythema, vesicles, erosions, ulceration and hypopigmentation at the application site. Flu-like symptoms are very rare [14, 79]. To minimize local adverse effects, the treatment area should be washed with soap and water 6 to 10 hours after application.
Synecatechin ointment is an aqueous extract of green tea (Camellia sinensis) leaves and is available as a 10 and 15% ointment. The drug is believed to act by reducing viral replication by upregulating genes associated with apoptosis and modulating genes involved in the proinflammatory response to HPV infection [7, 79]. Synecatechin ointment is a safe and effective treatment for penile warts in immunocompetent men aged 18 years and older [13, 84]. It is recommended to use synecatechin ointment three times daily for 16 weeks [6, 7]. The ointment should not be washed off until the next use [6]. Two phase III randomized, double-blind studies (n = 1005) showed that the rate of complete removal of warts and their recurrence after 12 weeks of genital warts was significantly higher than in the control group (P < 0.001 and P < 0.001, respectively) [6]. Adverse effects include itching, burning, discomfort, irritation, pain, erythema, swelling, induration, vesicular rash, erosion and ulceration at the application site, occurring in approximately 20% of patients. Staining underwear is another unpleasant aspect of using this drug. A single-blind randomized controlled trial (n=42) showed that cryotherapy plus 15% synecatechin ointment was more effective in the treatment of external genital warts compared with cryotherapy alone (-5.0 lesions vs -2.1 lesions, respectively, P =0.07) [85].
Treatment methods used in the clinic
Methods used in the clinic include podophyllin, liquid nitrogen cryotherapy, bichloroacetic acid or trichloroacetic acid, oral cimetidine, surgical excision, electrocoagulation and carbon dioxide laser therapy [80, 81].
Liquid 25% podophyllin, derived from podophyllotoxin, works by stopping mitosis and causing tissue necrosis [7]. The drug is applied directly to the penile wart once a week for 6 weeks (maximum 0.5 ml per treatment) [7]. Podophyllin should be washed off 1 to 4 hours after treatment and should not be applied to areas with high skin moisture [7]. The effectiveness of wart removal reaches 62% [7]. Due to reports of toxicity, including death, associated with the use of podophyllin, podofilox is considered preferred, which has a much better safety profile [7].
Liquid nitrogen, the treatment of choice for the treatment of penile warts, can be applied using a spray or cotton-tipped applicator directly to and 2 mm around the wart [79]. Liquid nitrogen causes tissue damage and cell death by rapidly freezing to form ice crystals. The minimum temperature required to destroy warts is -50°C, although some authors believe that -20°C is also effective [86].
The effectiveness of wart removal reaches 75% [79]. Side effects include pain during treatment, erythema, desquamation, blistering, erosion, ulceration and dyspigmentation at the application site. A recent phase II parallel randomized trial in 16 Iranian men with genital warts showed that cryotherapy using Wartner's formulation containing a mixture of 75% dimethyl ether and 25% propane was also effective. Further research is needed to confirm or refute this conclusion. It must be said that cryotherapy using Wartner’s composition is less effective than cryotherapy using liquid nitrogen [86].
Bichloroacetic acid and trichloroacetic acid can be used to treat small penile warts, as their ability to penetrate the skin is limited [79]. Each of these acids works by coagulating protein followed by cell destruction and consequently removing the penile wart [7]. A burning sensation may occur at the application site. Relapses after using bichloroacetic or trichloroacetic acid occur as often as with other methods. The drugs can be used up to three times a week [7]. The effectiveness of wart removal ranges from 64 to 88% [7].
Cimetidine, an H2 receptor antagonist, is thought to act by enhancing cellular immunity against HPV [87]. The recommended dose is 25 - 40 mg/kg/day orally. The drug is safe, painless and well tolerated [88].
Electrocoagulation, laser therapy, carbon dioxide laser, or surgical excision work by mechanically destroying the wart and can be used in cases where there is a fairly large wart or cluster of warts that is difficult to remove with conservative treatment methods [4, 79, 89, 90]. Mechanical treatment methods have the highest percentage of effectiveness, but their use has a higher risk of scars on the skin. Local anesthesia such as Nanorap (hydrogel with 2.5% lidocaine and 2.5% prilocaine with 50% active substances in nanocapsules), which is applied to the lesions without occlusion 20 minutes before the procedure, or a mixture of local anesthetics (EMLA) applied on occluded lesions an hour before the procedure should be considered as measures that reduce discomfort and pain during manipulation [44]. General anesthesia may be used to surgically remove large lesions.
Alternative Treatments
Patients who do not respond to first-line treatments may respond to other treatments or a combination of treatments [75, 79]. Second-line therapy includes topical, intralesional, or intravenous cidofovir, topical 5-fluorouracil, and topical ingenol mebutate.
Antiviral therapy with cidofovir may be considered for immunocompromised patients with refractory warts [14]. Cidofovir is an acyclic nucleoside phosphonate that competitively inhibits viral DNA polymerase, thereby preventing viral replication [79, 91].
Side effects of topical (intralesional) cidofovir include irritation, erosion, post-inflammatory pigmentary changes, and superficial scarring at the application site [88]. The main side effect of intravenous cidofovir is nephrotoxicity, which can be prevented with saline hydration and probenecid [91].
Topical 5-fluorouracil is also effective in the treatment of penile warts [92]. 5-fluorouracil is a fluoropyrimidine antimetabolite that is an analogue of pyrimidine nucleoside. The drug blocks the action of thymidylate synthase and thereby stops the production of DNA. A systematic review of the Cochrane database of six randomized placebo-controlled trials involving 988 patients with genital warts found that topical 5-fluorouracil was more effective than no treatment or placebo (relative risk: 0.39; 95% confidence interval: 0. 23-0.67) [92]. The authors caution that further research is needed due to the lack of high-quality randomized placebo-controlled trials [92]. Side effects of topical 5-fluorouracil include pain, burning, inflammation and ulceration at the application site [79].
Preliminary studies have shown that topical application of ingenol mebutate gel is effective in the treatment of genital warts [93 – 95]. Ingenol mebutate acts by inducing cell death in proliferating keratinocytes and stimulating an inflammatory response characterized by neutrophil infiltration. Local skin irritation may occur within 24 to 48 hours [94, 95]. The relapse rate is unknown.
Prevention
Genital warts can be prevented to a certain extent by delaying the onset of sexual activity and limiting the number of sexual partners [3]. Latex condoms, when used consistently and correctly, reduce HPV transmission. Sexual partners with anogenital warts should be treated.
HPV vaccines are effective before sexual activity in the primary prevention of infection [5]. This is because vaccines do not provide protection against disease caused by vaccine-derived HPV types that an individual acquired through previous sexual activity [96]. The Advisory Committee on Immunization Practices of the Centers for Disease Control and Prevention, the American Academy of Pediatrics, the American College of Obstetricians and Gynecologists, the American Academy of Family Practice, and the International Human Papillomavirus Society recommend routine vaccination of girls and boys with the HPV vaccine [81, 97 – 101].
The target age for vaccination is 11–12 years for girls and boys [100–102]. The vaccine can be administered as early as 9 years of age [97]. Three doses of HPV vaccine should be given at month 0, months 1–2 (usually 2), and months 6 [97]. Catch-up vaccination is indicated for men under 21 years of age and women under 26 years of age if they have not been vaccinated at the target age [99–102]. Vaccination is also recommended for men who are homosexual or immunocompetent under the age of 26 years, if they have not been vaccinated previously [100, 101]. Vaccination reduces the likelihood of becoming infected with HPV and subsequently developing penile warts and penile cancer. Vaccinating both men and women is more beneficial in reducing the risk of genital warts of the penis than vaccinating only men, since men can acquire HPV infection from their sexual partners. The prevalence of anogenital warts decreased significantly from 2008 to 2014 due to the introduction of the HPV vaccine [103].
The annual percentage change among men aged 20–24 years was -6% (P=0.005) [103]. The decline in prevalence is most likely the result of mass vaccination among women. A systematic review and meta-analysis of six studies (n=27,078) found that the quadrivalent HPV vaccine is effective in preventing anogenital warts in both men and women [104]. The 9-valent vaccine (Gardasil-9), which replaced the 4-valent vaccine (Gardasil), targets HPV types 6, 11, 16, 18, 31, 33, 45, 52 and 58 and contains their viral particles [96, 101 , 105]. The 9-valent vaccine is effective in preventing penile warts. The bivalent vaccine (Cervarix) targets only HPV types 16 and 18 and is not effective in preventing penile warts [97]. Data on the safety of HPV vaccines are encouraging [102].
Conclusion
Penile warts are a sexually transmitted disease caused by HPV. This pathology can have a negative psychosocial impact on the patient and negatively affect his quality of life. Although approximately one third of penile warts resolve without treatment, active treatment is preferred to speed up the resolution of warts, reduce fears of infection, reduce emotional distress, improve cosmetic appearance, reduce social stigma associated with penile lesions, and relieve symptoms.
Active treatment methods can be mechanical, chemical, immunomodulatory and antiviral, and often combined. So far, no one treatment has been proven to be superior to others. The choice of treatment method should depend on the physician's level of proficiency in this method, the patient's preference and tolerability of treatment, as well as the number of warts and the severity of the disease. The comparative effectiveness, ease of use, side effects, cost and availability of the treatment should also be taken into account. HPV vaccines before sexual activity are effective in primary prevention of infection. The target age for vaccination is 11 - 12 years for both girls and boys.