Neuritis
is an inflammation of the peripheral nerve trunk.
The peripheral nervous system refers to the nerve structures outside the brain and spinal cord (which are in turn called the central nervous system). Excitation (signal) is transmitted along the nerves, allowing the central nervous system to receive information about the state of all organs and systems of our body and control muscle contractions. The tissues of various organs are penetrated by nerve endings, which are connected to the brain, and in most cases to the spinal cord using bundles of nerve fibers enclosed in a sheath of connective tissue. Such bundles are called nerves, and large nerves are called nerve trunks.
With neuritis, nervous tissue is involved in the inflammatory process. This leads to the fact that the signal in some part of the nerve passes worse or does not pass at all. Accordingly, the sensitivity of any area may be lost and the mobility of the muscles innervated by the affected nerve may decrease.
Types of neuritis
A distinction is made between local neuritis and polyneuritis.
Local neuritis
is an inflammation of any one nerve (facial, auditory, oculomotor, glossopharyngeal, radial, sciatic, peroneal, femoral, etc.).
Polyneuritis
is multiple inflammation of the nerves. If the effect of the factor that caused the inflammation is local, only one nerve is affected. Polyneuritis develops under the influence of a systemic factor, which, as a rule, leads to degeneration of the nerve sheath and nerve fibers.
Classification of neuritis
Depending on the number of affected nerves, it is customary to distinguish two forms of neuritis:
- mononeuritis - one nerve is affected;
- polyneuritis - several nerves are affected.
Depending on which nerve is affected, there are:
- neuritis of the facial nerve;
- trigeminal neuritis;
- acoustic neuritis;
- ulnar nerve neuritis;
- other.
At CELT you can get advice from a specialist algologist.
Make an appointment
Causes of neuritis
Local neuritis is caused by:
- local infection;
- local hypothermia;
- injury. Often neuritis develops after a nerve injury;
- compression of the nerve. Thus, neuritis of the axillary nerve can develop due to prolonged use of a crutch, neuritis of the peroneal nerve - due to working in an uncomfortable position, etc.;
- arthritis (in this case the nerve of the joint may become inflamed);
- tumor (if the tumor compresses the nerve).
Multiple neuritis (polyneuritis) can be caused by such reasons as:
- infectious diseases, including measles, herpes, influenza, malaria, diphtheria and some others;
- intoxication. Poisoning with arsenic, lead, mercury, carbon monoxide, phosphorus, bismuth and other highly toxic substances can lead to the development of various types of neuritis. The most common cause of multiple neuritis is alcohol poisoning;
- systemic diseases (diabetes mellitus, rheumatism, gout);
- avitaminosis;
- vascular disorders;
- as well as some other reasons.
Causes of neuritis
In order to correctly prescribe treatment for neuritis, it is necessary to correctly identify the causes that caused it. These are bacteria and viruses, as well as:
- intoxication due to poisoning with alcoholic beverages, medications, food;
- nerve compression;
- injury.
The reasons may lie in a number of diseases:
- diabetes;
- rheumatism;
- metabolic disease;
- excess body weight.
Symptoms of neuritis
The main symptoms of neuritis are:
Pain along the nerve
The most common symptom of neuritis is pain along the affected nerve. The pain, as a rule, is dull in nature and intensifies in the cold, with physical activity or uncomfortable body position.
Sensory impairment
Sensory loss in the area of the affected nerve is common. It can manifest itself in the form of numbness, tingling, or “pins and needles.”
Decreased muscle activity
There is a partial decrease in muscle strength (paresis), a decrease or loss of tendon reflexes, and in some cases, muscle paralysis (complete cessation of muscle activity).
Vegetative and trophic disorders
With neuritis, there may be such vegetative and trophic disorders as depigmentation of the skin, the acquisition of a bluish tint, local hair loss, increased sweating and dry skin, swelling.
Treatment
The choice of therapeutic tactics is determined by the nature of the disease, the intensity of symptoms, the presence of concomitant disorders, as well as the characteristics of the patient’s body.
The First Medical Clinic implements an integrated approach to the treatment of neuropathies, neuritis and neuralgia using unique, highly effective modern methods, such as:
- therapeutic blockades;
- autoplasmotherapy;
- reconstruction of the spine (intervertebral discs);
- photodynamic therapy;
- transcutaneous electrical stimulation;
- ozone therapy and others.
For emergency relief from acute pain (this is of particular importance for neuralgia), they resort to blockades of nerves or their roots. The method is based on the administration of painkillers directly to the affected area. The high concentration of the active substance at the site of pathology allows you to almost instantly block the transmission of the pain impulse and ensure pain relief.
Treatment of neurology
High therapeutic effectiveness in treating neurological diseases is demonstrated by the method of plasma therapy - the use of platelet autoplasma. A small volume of the patient's venous blood is centrifuged. The result is plasma with a high content of platelets, sources of bioactive substances such as growth factors. Plasma injection leads to the release of these growth factors at the site of pathology, where they activate tissue regeneration processes. As a result, swelling and inflammation are relieved, pain is reduced, and pathological changes are eliminated.
If nerve damage is caused by spinal pathologies, reconstruction of the intervertebral disc and photodynamic therapy can help reduce the symptoms of the disease, as well as eliminate the cause of the disease. During reconstruction, the medicine is injected directly into the intervertebral disc, which stimulates its self-healing processes. In photodynamic therapy, a photosensitizing drug is applied to the skin in the area of the affected nerve and the area is exposed to laser radiation. As a result, the source of pathology is destroyed by high-energy oxygen.
With transcutaneous electrical stimulation, short pulses of electric current are applied to the area where the diseased nerve passes.
The required amount of therapeutic assistance can only be determined by a specialist after diagnostic procedures. If you have signs of nerve damage, we recommend that you contact the First Medical Clinic in a timely manner.
You can make an appointment for a consultation and appointment by phone
Treatment methods for neuritis
Neuritis must be treated. At the first signs of the disease, you should consult a neurologist. If treatment for neuritis is not started on time, the risk of developing paresis and muscle paralysis increases.
Treatment of neuritis is aimed, first of all, at eliminating the cause that caused it. If neuritis is of infectious origin, antibacterial therapy or antiviral drugs are used. If neuritis is of toxic origin, it is important to remove toxins from the body.
Drug treatment
In addition to antibacterial or antiviral drugs, the course of treatment for neuritis usually includes:
- B vitamins
- drugs that improve blood microcirculation
- drugs that increase the conductivity of nerve fibers
Massage
Massage of the muscles innervated by the affected nerve is recommended. Massage can be combined with heat therapy (infrared sauna).
More information about the treatment method
Physiotherapy
For neuritis, physical therapy methods such as electrophoresis, diadynamic therapy, SMT therapy, ultrasound therapy, magnetic therapy, and laser therapy can be used.
More information about the treatment method
Make an appointment Do not self-medicate. Contact our specialists who will correctly diagnose and prescribe treatment.
Rate how useful the material was
thank you for rating
Diagnosis of neuritis
Specialists at the CELT Pain Clinic pay special attention to differentiating neuritis from:
- multiple sclerosis;
- brain tumors;
- circulatory disorders in the brain.
Facet blockade
- Cost: 10,500 rub.
- Duration: 15-30 minutes
- Hospitalization: 2 hours in hospital
More details
In addition to examination and history taking, electroneuromyography can be used. Thanks to it, you can assess the degree of nerve damage and predict how the disease will progress.
Neuralgia: causes
Most often, neuralgia affects nerves passing through canals and through openings that have a small diameter. She may be:
- Primary – appeared independently, not against the background of other diseases;
- Secondary – developing against the background of inflammation, tumor or other abnormal processes that negatively affect the nerve.
| Type of neuralgia | Initiating factors of development |
| Trigeminal neuralgia | In 95% it is initiated by compressive pressure on the trunk and branches of the nerve. The reasons for the development are the following:
|
| Intercostal neuralgia | The causes of intercostal neuralgia, which initiate compression of the nerve roots, are as follows:
|
| Neuralgia of the submandibular and sublingual nodes | The causes of intercostal neuralgia, which initiate compression of the nerve roots, are as follows:
|
Causes of inflammation of the trigeminal nerve
There are several reasons leading to inflammation of the nerve ducts:
- Poor blood supply associated with physical compression of the nerve. First of all, this is swelling caused by diseases of the ENT organs. The resulting tumor can also pinch the nerves.
- Inflammation associated with dentistry. This includes gingivitis, periodontitis, caries, pulpitis, and eruption of wisdom teeth. Each of these diseases can lead to suppuration, abscesses, swelling and bacterial infections of tissues.
- Medical error by an anesthesiologist - if the injection was given unsuccessfully and the needle got into a nerve, pain cannot be avoided.
- Hypothermia causes muscles to lose their elasticity, which leads to pinching of the nerves passing between the fibers.
- Bacterial infections, in particular tetanus and polio.
- The cause of inflammation of the trigeminal nerve, which is difficult to diagnose, is the psychological state of a person - frequent experiences, stress, and nervous disorders.
To determine the cause of inflammation, you need to consult a specialist.
Diagnosis of trigeminal neuralgia
A preliminary diagnosis can be made by a neurologist based on the patient’s complaints, studying the history of his disease and an objective examination of the face with an assessment of symmetry at rest and when trying to smile. Also, during the consultation, the doctor may conduct additional tests, asking the patient to close his eyes, purse his lips, frown, etc.
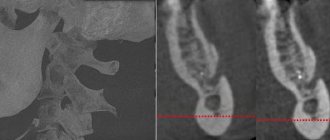
Laboratory and instrumental diagnostics of trigeminal neuralgia include the following examinations:
- general blood and urine tests;
- computed tomography (CT) and magnetic resonance imaging (MRI);
- radiography of the paranasal sinuses;
- panoramic radiography of the oral cavity;
- electroneuromyography to determine the localization of inflammation.
Neuralgia: symptoms
Clinical manifestations of neuralgia include pain symptoms. It manifests itself in attacks and affects the area of innervation. In addition, the patient may suffer from redness of the skin in the affected area, lacrimation, and convulsive muscle contractions.
| Type of neuralgia | Clinical manifestations |
| Trigeminal neuralgia | The syndrome is characterized by attacks of severe shooting pain along the line of the trigeminal nerve on the left or right. They can be short-term (lasting up to two minutes) or long-term burning pain (lasting up to three days). This symptom most often affects one side of the face. In addition, a spasm or tic of the facial muscles may develop. The pain may involve the eyes, jaws and ears. |
| Intercostal neuralgia | Symptoms of intercostal neuralgia are as follows:
|
| Neuralgia of the submandibular and sublingual nodes | It is characterized by the sudden development of pain symptoms affecting the submandibular area on one side. The anterior two thirds of the tongue hurt; the attack can last from a couple of minutes to one hour. In this case, irradiation to the neck, occipital and temporal regions is possible. Against this background, swelling of the tongue and the area under the lower jaw is possible, and there are disturbances in salivation. |
The most common types of neuralgia are:
Intercostal neuralgia
Intercostal neuralgia is compression and pinching (and sometimes irritation) of nerves and nerve ganglia that are located in the intercostal area.
Symptoms of intercostal neuralgia: pain is constant or paroxysmal, and can be shingles.
Pain is usually felt only in one half of the chest (in the intercostal spaces). Sometimes patients complain of impaired sensitivity, tension in the back muscles, pain increases with coughing, deep breathing, body movements and physical activity, as well as with palpation of the sore area. Trigeminal neuralgia
Typical trigeminal neuralgia is characterized by pain on one side of the face, which manifests itself as an attack. The pain is severe in intensity, stabbing in nature, and lasts for several seconds.
As a rule, pain is triggered by something. Thus, it can occur when hypothermia, overheating, chewing, articulation or touching the corresponding part of the face.
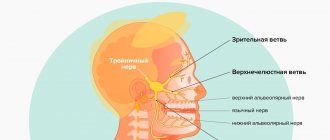
The trigeminal nerve is divided into three branches:
- optic branch: responsible for the sensitivity of the forehead and eyelids
- maxillary branch: responsible for the sensitivity of the area from the eyes to the upper lip
- mandibular branch: responsible for the lower lip and the area from the lower jaw to the neck
Neuralgia of the occipital nerve
Neuralgia of the occipital nerve is accompanied by pain in the head area of a shooting nature.
The pain syndrome occurs due to a pinched nerve. As neuralgia progresses, the roots of the cervical spine (from which the occipital nerves are formed) can be affected - the pain becomes constant, and any, even the slightest movements of the head during an attack can be accompanied by nausea, vomiting and sometimes fainting. Pain can also radiate (spread) to the temple, forehead, and eyes. Neuralgia of the external cutaneous nerve of the thigh
The disease develops gradually and is characterized by unilateral damage. Patients complain of a feeling of tingling, numbness, and burning, which first occurs in certain areas of the thigh. Over time they become permanent. The pain appears over several months. Sensitivity along the anterior outer surface of the thigh is impaired. The pain is caused by compression of the fibers of the external cutaneous nerve of the thigh under the inguinal ligament. Some researchers consider such neuralgia to be a manifestation of osteochondrosis.