- home
- Articles
- Treatment of stomatitis in the mouth in adults and children
Damage to the mucous membranes of the mouth is called stomatitis. The disease can occur in several types, each of which requires a special type of treatment. That is why you cannot take any medications on your own, since the incorrect selection of medications will only aggravate the course of the disease.
What it is
This type of stomatitis is provoked by enteroviruses entering the body. The very concept of “enterovirus” unites a large number of viral infections that actively multiply in the human gastrointestinal tract when they enter it with water, with agricultural products or from animal carriers. The virus can also be transmitted through blood-sucking insects, entering directly into the blood and ultimately leading to the development of vesicular stomatitis.
Due to their increased resistance to high acidity, detergents and even chlorine in running water, enteroviruses can survive in unboiled milk and cold-leavened dairy products, on the surface of vegetables, fruits and herbs for up to three to four months. The only way to combat them is heat treatment at a temperature of at least fifty degrees.
Enteroviral stomatitis does not occur in all people who become ill under the influence of this group of viruses, however, the occurrence of vesicular inflammation during enterovirus infection is far from uncommon, especially if there are microdamages to the mucous membrane in the oral cavity.
Diagnostic methods
Diagnosis in most cases can be made by characteristic symptoms, physical examination, and medical history.
After examining and collecting complaints, the pediatrician will prescribe a series of tests aimed at identifying the type of virus. The doctor may prescribe:
- general urine analysis;
- stool analysis;
- blood tests (general, biochemical, serological, etc.);
- immunohistochemical analysis of tissues (to detect antibodies to enterovirus infection);
- cultures of biomaterial (saliva, throat scrapings, etc.).
An accurate diagnosis may also require a differential diagnosis to exclude other diseases with a similar clinical picture.
Other diagnostic tests are also performed:
- Laboratory Serology is a blood test that detects an increased amount of antibodies. The body produces them to fight the virus in the acute period and during the recovery stage. The analysis allows you to determine ECHO 6, 7, 9, 11, 30 and Coxsackie B1-B6. A negative result does not necessarily mean that you do not have the disease; it just does not detect other types of viruses. PCR is a highly sensitive (100%) and specific (97%) test. Allows the detection of enterovirus RNA in the cerebrospinal fluid. Blood PCR detects the virus in 30% of patients with chronic fatigue syndrome. Source: A.V. Demina, V.A. TERNOVOY, N.I. Shulgina, S.V. Netesov Enteroviruses. Part 3. Laboratory diagnostics, treatment, immunoprophylaxis // Bulletin of the Siberian Branch of the Russian Academy of Medical Sciences, volume 31, No. 3, 2011. An analysis of cerebrospinal fluid is needed if there are symptoms of damage to the spinal cord, brain and their membranes. The fluid is collected by puncturing. With aseptic meningitis, the level of leukocytes is increased. Glucose is normal or slightly reduced. Protein is normal or slightly increased. Troponin I and cardiac enzymes is a blood test to determine the level of these indicators. If they are elevated, it means the heart is damaged. Normally, the serum troponin I level should be from 0 to 0.5 ng/ml. RT-PCR is an analysis to detect common regions of enterovirus RNA. The test has a sensitivity of 95% and specificity of 97%. Approved for the diagnosis of enteroviral meningitis. The best results are obtained if the material for research is cerebrospinal fluid. Sputum, blood and mucus from the respiratory tract, and feces can be examined. However, the result will not be as accurate.
- Instrumental Electroencephalography – assesses the degree and severity of the disease. Chest X-ray - may reveal an increase in cardiac volume in patients with myopericarditis. Echocardiography – performed if myocarditis is suspected. Shows abnormal movement of the walls of the heart chambers. May reveal acute reduction in ejection fraction and ventricular dilatation in severe cases. Examination by an ophthalmologist using a slit lamp is indicated for those children who have hemorrhagic conjunctivitis and corneal erosions. Coxsackie A24 and Enterovirus 70 viruses can be detected from conjunctival smears within 3 days of infection.
Causes
Enteroviruses themselves exist everywhere, and it is impossible for humans to avoid encountering them. However, these viruses do not provoke disease in all people, much less the formation of vesicular stomatitis. The most important prerequisite for its onset is a reduced level of the body’s resistance to infections due to weakened immunity.
Main methods of infection:
- airborne droplets (when talking to a carrier, sneezing, coughing);
- contact (through common objects);
- fecal-oral (when the virus gets from manure used for fertilizer onto vegetables, herbs and fruits).
The main viral agents that can be called vesicular stomatitis viruses are enterovirus 71 and Coxsackie viruses.
The risk of the disease in adults is very small; children in the first two to three years of life mainly suffer from this complication of enterovirus infection. Peaks of incidence occur in autumn and spring, and in warmer countries the risk of getting sick increases from mid-summer, since with high air temperatures and high humidity, the lifespan of the virus outside the host’s body increases greatly.
Types of enteroviruses
There are more than 100 causative agents of this infection. The main ones are ECHO, polioviruses (the causative agents of polio), Coxsackie viruses A and B, and enteroviruses that cannot be classified.
Coxsackie viruses are several serotypes of the pathogen belonging to groups A, B and C. Coxsackie viruses type A are the cause of severe forms of enteroviral diseases. These are hemorrhagic conjunctivitis, herpetic sore throat, aseptic meningitis. Type B is more dangerous because it provokes hepatitis, myocarditis, and pericarditis. Source: V.V. Botvinyeva, L.S. Namazova-Baranova, O.B. Gordeeva, O.K. Botvinyev, T.N. Konopleva Modern possibilities for diagnosis, prevention and treatment of Coxsackie enterovirus infection in children // Pediatric pharmacology, article received: 01/22/2012, accepted for publication: 05/12/2012.
ECHO viruses are most dangerous for newborns. In them they cause meningitis, myocarditis, and hepatitis. This often causes death. There are no complications in older children.
Symptoms
Most often, the disease caused by enteroviruses is asymptomatic, but some patients (up to three percent of all infected) experience serious complications. The most common of them is enteroviral vesicular stomatitis with exanthema, i.e. rashes (grayish-white vesicles) localized on the palms, soles and mouth (on the inner surface of the cheeks, on the lips, tongue and even in the throat). It is thanks to this localization of the rash that vesicular stomatitis with exanthema received another name, often used among the people - “arm, leg, mouth” syndrome.
In addition to the characteristic rash with severe itching, increased salivation and pain when swallowing, this disease may be accompanied by increased body temperature and fever, weakness, chills, muscle pain, hyperemia and swelling of the soft tissues of the oral cavity, headaches and pain in the gastrointestinal tract, nausea, vomiting or diarrhea, runny nose and sore throat, and photophobia.
Since rashes appear later than other symptoms, clinic doctors often make the wrong diagnosis: acute respiratory infections, acute respiratory viral infections, allergies, dermatitis, rotavirus infection, herpes, and even simple teething. Accordingly, medications are prescribed that eliminate some of the symptoms, but blur the picture of the underlying disease.
In fact, with a fairly mild course of the disease, no specific treatment for enteroviral vesicular stomatitis is required. The first signs appear five to six days after infection, blisters appear around the third day, and after seven to ten days the patient fully recovers.
The incubation period for this infection can vary from a couple of days to a week. In the initial stages of the disease, the infectiousness of the infected person is much higher than in recent days, however, the elimination of enterovirus in feces can continue for up to a month after the onset of the disease.
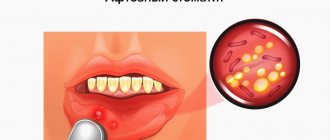
Vesicular stomatitis: before and after photos
The disease vesicular stomatitis mainly occurs in the summer, when insects become more active. 2-6 days after the virus enters the body, a person begins to feel a headache and chills, he has a fever, enlarged cervical lymph nodes, a runny nose, and ulcers affect the lips, gums, inner surfaces of the cheeks and tongue. Rashes with vesicular stomatitis are quite painful, so eating causes severe discomfort.
How to treat
Since a sick child is contagious to the entire group of children (adults are least susceptible to the disease), the first step is to isolate him from other children. If you find rashes on the oral mucosa, you need to contact your dentist, who will tell you how to treat vesicular stomatitis.
Most often, no specific treatment is prescribed. In case of increased pain, the child may be prescribed painkillers, local applications and rinses. Antiviral drugs and vitamin-mineral complexes may also be prescribed to support immunity. During the period of illness, it is necessary to carefully observe hygiene, be sure to wash your hands with soap after visiting the toilet and before eating.
Treatment of vesicular stomatitis
When treating vesicular stomatitis, symptomatic therapy is prescribed, including:
- drinking plenty of water;
- complete rest;
- treatment of the oral mucosa with antiseptic solutions;
- taking antipyretic drugs;
- the use of antiviral ointments (oxolinic, redoxol, tebrofen).
As a rule, vesicular stomatitis does not cause complications, and signs of the disease quickly go away if the patient strictly follows the doctor’s instructions.
A childhood viral disease is also treated quite quickly and goes away without a trace if you see a dentist on time. As a medicine, the doctor may recommend taking an immunomodulator, which will help cope with the disease and will be an excellent prophylactic for the prevention of other viral diseases.
Treatment of vesicular stomatitis of the enteroviral type is generally carried out in the same ways as usual, that is, it is symptomatic. The disease cannot be neglected, as there is a risk of developing such serious complications as meningitis, encephalitis and acute flaccid paresis.
Another important point in the treatment of vesicular stomatitis in children is the isolation of children from the group so that the disease is not transmitted to others. And do not forget that hygiene items (in particular, a towel) must be individual.
Prevention
The basis for the prevention of enterovirus infection in a child is compliance with the rules of hygiene:
- washing hands and food before consumption;
- boiling water;
- avoiding places where large numbers of people gather during an epidemic.
- It is extremely important to take measures to increase immunity: follow a routine, eat right, and harden yourself.
In the pediatric medical department, all conditions have been created for the diagnosis and treatment of enterovirus infection in a child. For seriously ill patients, the department operates a 24-hour hospital, where the small patient will be under the constant supervision of qualified medical personnel and doctors. Remember that the sooner the correct diagnosis is made and the type of virus is determined, the easier it will be to cure the child and avoid complications.
Sources:
- G.P. Martynov. Enterovirus (non-polio) infection in children // Siberian Medical Review, 2014.
- V.V. Botvinyeva, L.S. Namazova-Baranova, O.B. Gordeeva, O.K. Botvinyev, T.N. Konopleva. Modern possibilities for diagnosis, prevention and treatment of Coxsackie enterovirus infection in children // Pediatric pharmacology, article received: 01/22/2012, accepted for publication: 05/12/2012.
- A.V. Demina, V.A. Ternova, N.I. Shulgina, S.V. Netesov. Enteroviruses. Part 3. Laboratory diagnostics, treatment, immunoprophylaxis // Bulletin of the Siberian Branch of the Russian Academy of Medical Sciences, volume 31, No. 3, 2011.
Markova Daria Olegovna Clinic
Author of the article
Markova Daria Olegovna
Specialty: pediatrician
Experience: 15 years
The information in this article is provided for reference purposes and does not replace advice from a qualified professional. Don't self-medicate! At the first signs of illness, you should consult a doctor.
Treatment methods for enterovirus infection
Drug therapy is:
- medications to relieve symptoms (antipyretics, painkillers, etc.).
- vitamins and microelements.
To relieve symptoms, a child may be prescribed medications from different groups:
Painkillers and antipyretics to relieve headaches, muscle pain, and fever. These are “Ibuprofen”, “Paracetamol”, “Ibuklin”, “Nurofen for children”, etc.
Immunoglobulins stimulate the child's immunity. They are administered by injection - intramuscularly or intravenously. The second option is more effective and common.
Important! Antiviral drugs have not been shown to be highly effective in later stages and are not included in the formal treatment plan. They help at a very early stage, when 5-10 hours have passed since infection. But identifying the disease at this stage is almost impossible.
Vitamins (especially vitamin D) and supplements containing essential microelements (magnesium, zinc, potassium, selenium, calcium) help fight the virus well support the child’s body during this difficult period
Important! Antibiotics do not work against enterovirus infection, since they are antibacterial, not antiviral drugs.
The child should be provided with bed rest, drinking plenty of fluids using solutions to restore water and electrolyte balance, and a special gentle diet. The main purpose of the diet is to reduce intoxication and increase immunity, while being gentle on the digestive system. The diet should have enough vitamins, minerals, and protein.
Clinic, diagnosis and treatment of acute herpetic stomatitis in children
- What is the clinical picture of acute herpetic stomatitis?
- What are the new treatment regimens?
The problem of diseases of the oral mucosa is one of the most important in dentistry.
Acute herpetic stomatitis occupies a special place here, primarily because it accounts for more than 80% of all diseases of the oral mucosa in children. The combined use of virological, serological and immunofluorescence research methods confirms that acute herpetic stomatitis is one of the clinical forms of primary herpetic infection.
The spread of the disease in 71% of cases among children aged 1 to 3 years is explained by the fact that at this age, antibodies received from the mother interplacentally disappear in children, as well as the lack of mature specific immune systems. Among older children, the incidence is significantly lower due to acquired immunity after a herpes infection in its various clinical manifestations.
Great importance in the pathogenesis of the disease is attached to the lymph nodes and elements of the reticuloendothelial system, which is quite consistent with the pathogenesis of the sequential development of clinical signs of stomatitis. The appearance of lesions on the oral mucosa is preceded by lymphadenitis of varying severity. Most often they are observed in severe and moderate stomatitis. As a rule, lymphadenitis is bilateral, submandibular. However, with moderate and severe forms of the disease, simultaneous involvement of the cervical lymph nodes in the process is also possible. Lymphadenitis accompanies the entire period of the disease and persists for 7-10 days after complete epithelization of the elements.
The body's resistance to the disease is determined by its immunological defense. Both specific and nonspecific immune factors play a role in immunological reactivity. Violation of nonspecific immunological reactivity determines the severity of the disease and the periods of its development. Moderate and severe forms of stomatitis led to a sharp suppression of natural immunity, which was restored 7-14 days after the child’s clinical recovery.
The severity of acute herpetic stomatitis is assessed by the severity and nature of toxicosis and damage to the oral mucosa. The development of the disease goes through five periods: incubation, prodromal, period of disease development, extinction and clinical recovery.
| Elements of herpetic stomatitis |
The mild form of acute herpetic stomatitis is characterized by an external absence of symptoms of intoxication; the prodromal period is clinically absent.
The disease begins suddenly with an increase in temperature to 37-37.5°C. The general condition of the child is quite satisfactory. In the oral cavity there are signs of hyperemia and slight swelling, mainly in the area of the gingival margin (catarrhal gingivitis). In most cases, against the background of increased hyperemia, single or grouped lesions appear in the oral cavity, the number of which usually does not exceed six. The rashes are one-time only. The duration of the disease development is 1-2 days.
The period of extinction of the disease is longer. Within 1-2 days, the elements acquire a marble-like color, their edges and center are blurred. They are already less painful. After epithelialization of the elements, the phenomena of catarrhal gingivitis persist for 2-3 days, especially in the area of the anterior teeth of the upper and lower jaw.
In children suffering from this form of the disease, as a rule, there are no changes in the blood, sometimes only towards the end of the disease a slight lymphocytosis appears (in children 1-3 years old, the number of lymphocytes is normally up to 50%). Herpetic complement-fixing antibodies are not often detected during convalescence. In this form, the protective mechanisms of saliva are well expressed: pH 7.4±0.04, which corresponds to the optimal state. At the height of the disease, the antiviral factor interferon appears in saliva from 8 to 12 units/ml. The decrease in lysozyme in saliva is not pronounced.
The moderate form of acute herpetic stomatitis is characterized by fairly clearly defined symptoms of toxicosis and damage to the oral mucosa during all periods of the disease. Already in the prodromal period, the child’s well-being worsens, weakness, loss of appetite appear, the child is capricious, there may be catarrhal tonsillitis or symptoms of an acute respiratory disease. The submandibular lymph nodes enlarge and become painful. The temperature rises to 37-37.5°C.
As the disease progresses (catarrhal phase), the temperature reaches 38-39°C, headache, nausea, and pale skin appear. At the peak of the rise in temperature, increased hyperemia and severe swelling of the mucous membrane, elements of the lesion appear both in the oral cavity and on the skin of the face in the perioral area. In the oral cavity there are usually from 10 to 20-25 lesions. During this period, salivation increases, saliva becomes viscous and viscous. Severe gingivitis and bleeding gums are noted.
Rashes often recur, as a result of which, when examining the oral cavity, one can see elements of the lesion that are at different stages of clinical and cytological development. After the first eruption of lesions, body temperature usually drops to 37-37.5°C. However, subsequent rashes are usually accompanied by a rise in temperature to the previous levels. The child does not eat, sleeps poorly, and symptoms of secondary toxicosis increase.
An ESR of up to 20 mm/hour is observed in the blood, often leukopenia, sometimes slight leukocytosis. Band and monocytes within the higher limits of normal, lymphocytosis and plasmacytosis. An increase in the titer of herpetic complement-fixing antibodies is detected more often than after suffering a mild form of stomatitis.
The duration of the period of extinction of the disease depends on the resistance of the child’s body, the presence of carious and damaged teeth in the oral cavity, and irrational therapy. The latter factors contribute to the fusion of lesion elements, their subsequent ulceration, and the appearance of ulcerative gingivitis. Epithelization of the lesion elements takes up to 4-5 days. Gingivitis, severe bleeding and lymphadenitis last the longest.
With a moderate course of the disease, the pH of saliva becomes more acidic, reaching 6.96 ± 0.07 during rashes. The amount of interferon is less than in children with a mild course of the disease, but does not exceed 8 units/ml and is not detected in everyone. The content of lysozyme in saliva decreases more than in mild forms of stomatitis. The temperature of the unchanged oral mucosa is in accordance with the child’s body temperature, while the temperature of the affected elements in the degeneration stage is 1.0-1.2°C lower than the temperature of the unchanged mucosa. With the beginning of regeneration and during the period of epithelization, the temperature of the affected elements rises to 1.80 and remains at a higher level until complete epithelization of the affected mucosa.
The severe form of acute herpetic stomatitis is much less common than the moderate and mild form.
During the prodromal period, all the signs of an incipient acute infectious disease occur: apathy, adynamia, headache, musculocutaneous hyperesthesia and arthralgia, etc. Symptoms of damage to the cardiovascular system are often observed: bradycardia and tachycardia, muffled heart sounds, arterial hypotension. Some children experience nosebleeds, nausea, vomiting, and pronounced lymphadenitis of not only the submandibular, but also the cervical lymph nodes.
During the development of the disease, the temperature rises to 39-40°C. The child has a mournful expression on his lips and painfully sunken eyes. There may be a mild runny nose, coughing, and the conjunctivae of the eyes are somewhat swollen and hyperemic. Lips are dry, bright, parched. In the oral cavity, the mucous membrane is swollen, clearly hyperemic, with pronounced gingivitis.
After 1-2 days, lesions up to 20-25 begin to appear in the oral cavity. Often, rashes in the form of typical herpetic blisters form on the skin of the perioral area, the skin of the eyelids and conjunctiva of the eyes, the lobes of the ears, on the fingers, like a panaritium. Rashes in the oral cavity recur, and therefore at the height of the disease in a seriously ill child there are about 100 of them. The elements merge, forming extensive areas of mucosal necrosis. Not only the lips, cheeks, tongue, soft and hard palate are affected, but also the gingival margin. Catarrhal gingivitis turns into ulcerative-necrotic. A sharp putrid odor from the mouth, profuse salivation mixed with blood. Inflammation in the mucous membranes of the nose, respiratory tract, and eyes worsens. Streaks of blood are also found in secretions from the nose and larynx, and sometimes nosebleeds are observed. In this condition, children need active treatment from a pediatrician and dentist, and therefore it is advisable to hospitalize the child in a boxed ward of a children's or infectious diseases hospital.
In the blood of children with severe stomatitis, leukopenia, a band shift to the left, eosinophilia, single plasma cells, and young forms of neutrophils are detected. In the latter, toxic granularity is very rarely observed. Herpetic complement-fixing antibodies are, as a rule, always detected during the period of convalescence.
Saliva has an acidic environment (pH 6.55±0.2), which can then be replaced by more pronounced alkalinity (8.1-8.4). Interferon is usually absent, the content of lysozyme is sharply reduced.
The diagnosis of acute herpetic stomatitis is made based on the clinical picture of the disease. The use of virological and serological diagnostic methods, especially in practical healthcare, is difficult. This is primarily due to the difficulty of conducting special research methods. In addition, with these methods, results can be obtained at best towards the end of the disease or some time after recovery. Such a retrospective diagnosis cannot satisfy the clinician.
It should be emphasized that in recent years the immunofluorescence method has been increasingly used. The high percentage of coincidences (79.0±0.6%) of the diagnosis of acute herpetic stomatitis, according to immunofluorescence data, with the results of virological and serological studies make this method the leading one in diagnosing the disease.
The doctor’s tactics when treating patients with acute herpetic stomatitis should be determined by the severity of the disease and the period of its development.
Due to the peculiarities of the course of acute herpetic stomatitis, rational nutrition and proper organization of feeding the patient occupy an important place in the complex of therapeutic measures. Food must be complete, that is, contain all the necessary nutrients, as well as vitamins. Therefore, it is necessary to include fresh vegetables, fruits, berries, and juices in your diet. Before feeding, the oral mucosa should be anesthetized with a 2-5% solution of anesthetic emulsion.
The child is fed predominantly liquid or semi-liquid food that does not irritate the inflamed mucous membrane. It is necessary to give the child enough fluids. This is especially important during intoxication. During meals, natural gastric juice or its substitutes should be given, since when there is pain in the mouth, the enzymatic activity of the stomach glands reflexively decreases.
Local therapy for acute herpetic stomatitis has the following objectives:
- relieve or reduce painful symptoms in the oral cavity;
- prevent repeated eruptions of lesions (reinfection) and promote their epithelization.
From the first days of the disease, given its etiology, in local treatment, serious attention should be paid to antiviral therapy. For this purpose, it is recommended to use 0.25% oxolinic, 0.5% tebrofen ointments, Zovirax, solutions of interferon and neoferon.
It is recommended to use the listed medications repeatedly (3-4 times a day) not only when visiting a dentist, but also at home. It should be borne in mind that antiviral agents must be applied to both the affected areas of the mucosa and areas that do not contain elements of the lesion, since they have more of a preventive effect than a therapeutic one.
During the period of extinction of the disease, antiviral drugs can be discontinued.
Particular importance should be attached to keratoplasty agents at this time. These are primarily oil solutions A and B, sea buckthorn oil, caratoline, rosehip oil, ointments with methyluracil, and an oxygen cocktail.
A study of the state of local immunity in children with acute herpetic stomatitis revealed that it correlates with the nature of the pathological process, therefore we consider it pathogenetically justified to include measures aimed at their elimination in a comprehensive treatment regimen.
At the Department of Pediatric Therapeutic Dentistry of the Moscow State Medical University, the drug imudon from Solvay pharma was prescribed to 80 children aged 2 to 4.5 years in the complex treatment of acute herpetic stomatitis. 40 children were diagnosed with mild, 38 children with moderate and 2 with severe forms of stomatitis.
Imudon is a mixture of lysates: 0.050 g (dry product) Lactobassillus acidophilus, fermentatum, helveticus, lactis Streptococcus pyogenes (2 var.), faecalis, faecium, sanguinis Staphilococcus aureus Klebsiella pneumoniae, Corynebacterium pseudodiphteriticum, Fusiformis fusiformis, Candida albicans.
Preservative: Sodium mercurothiolate: 0.0125 mg.
Excipients: lactose, mannitol, saccharin, sodium bicarbonate, anhydrous citric acid, precirol fine, magnesium stearate, polyvinylpyrrolidone.
pharmachologic effect
Imudon is intended for local specific immunotherapy of diseases of the oral cavity and pharynx. The effect of the drug on the immune system is expressed in an increase in the phagocytic activity of macrophages, an increase in the content of lysozyme in saliva, as well as an increase in the number of immunocompetent cells and the content of local antibodies (class A immunoglobulins). Thus, imudon has a therapeutic specific antimicrobial and anti-inflammatory effect, and also, by increasing the immune local protective barrier, ensures the prevention of relapses.
The first group consisted of children treated with 0.5% tebrofen ointment, the second group included children treated with interferon solution. In the third group, on the day of treatment, in addition to 0.5% tebrofen, imudon was prescribed, and in the fourth group, imudon + interferon. Children took Imudon tablets 5-6 times a day, no earlier than 30-40 minutes after treating the oral cavity with antiviral ointment, and dissolved it in the oral cavity.
Criteria for clinical and laboratory assessment of the therapeutic effectiveness of the drug imudon:
- The therapeutic effect is the average recovery time.
- Analgesic effect.
- General and local reactions to the drug.
- Influence on the state of local immunity.
Recovery was considered to be the epithelization of the lesion elements without a complete cure of the child from acute herpetic stomatitis, the duration of which is determined not only by the end of the epithelization of the lesion elements, but also by the duration of gingivitis and lymphadenitis, as well as deviations in the general well-being of the child.
As can be seen from table. 1, timely correction of local immunity increases the effectiveness of ongoing treatment measures and allows for faster recovery of children with AHS.
The effectiveness of the drug was manifested in groups 3 and 4 on the second day in case of contacting a doctor on the first day of the disease: erosions did not develop into aphthae, and the surrounding mucous membrane was not infiltrated.
Table data 1 indicate the advantage of complex therapy for OGS over generally accepted methods of treatment, its high efficiency, confirmed by a reliable reduction in the time of epithelization of elements and recovery of children.
The more effectively the drug stops the disease, the faster it normalizes the pathological infectious process, the more actively the factors of local immunological defense are restored. (Table 2).
We have given a high assessment of the effectiveness of the new regimen of complex therapy for AHS using stimulating immunotherapy, in particular imudon; It was concluded that there is a fundamental need for an integrated approach to the treatment of acute herpetic stomatitis with the mandatory inclusion of imudon, both a stimulating and a replacement agent for the correction of local immunity.
Thus, the high effectiveness of imudon in the treatment of AHS due to the immune correction of saliva has been established. Imudon has a therapeutic, anti-inflammatory effect, reduces the time for epithelization of lesions. There were no complications or side effects when using the drug imudon. Children used the drug with pleasure, as it has a pleasant, minty taste that does not irritate the mucous membrane. Apparently due to the mint aroma there is a weak analgesic effect.
All this allows us to recommend imudon in the complex therapy of acute herpetic stomatitis in children.
In conclusion, it should be noted that acute herpetic stomatitis, occurring in any form, is an acute infectious disease and requires in all cases the attention of a pediatrician and dentist in order to provide comprehensive treatment, eliminate contact of a sick child with healthy children, and take measures to prevent this diseases in children's groups.