Allergic laryngeal edema is a pathological condition characterized by inflammation of the mucous tissues of the larynx and narrowing of its lumen (stenosis). It occurs due to the body’s contact with factors hostile to it – allergens.
Author:
- Sadykhov Rahim Agalarovich
ENT pathology expert
2.40 (Votes: 42)
Allergic laryngeal edema is a pathological condition characterized by inflammation of the mucous tissues of the larynx and narrowing of its lumen (stenosis). It occurs due to the body’s contact with factors hostile to it – allergens, which cause a negative immune reaction. The main danger of edema is depression of respiratory function. As the lumen of the larynx narrows, breathing becomes difficult, which provokes oxygen deficiency, which is life-threatening.
Causes of swelling
Laryngeal edema occurs as a response of the body to an allergen irritant. This reaction is individual - under the same conditions, the same stimulus can cause a serious condition in one person, but not affect another in any way. It depends on the characteristics of the immune system.
Allergens may be the following:
- medications, especially when administered intravenously and intramuscularly;
- pet hair;
- insect bites;
- fungi, mold;
- food (often nuts, milk, eggs, fish, some vegetables, fruits);
- chemical substances;
- dust, pollen.
Burning sensation in the mouth and tongue - causes
Local factors:
- Decreased saliva secretion. The mucous membrane becomes dry, lips and tongue crack. Food and liquid irritate the damaged areas, and they sting quite severely.
- Fungal candidiasis. Popularly known as thrush. Fungi, during their rapid proliferation (which happens when the immune system is weakened), provoke a burning sensation in the oral mucosa and painful sensations.
- Hard dental deposits. The formation of tartar is accompanied by the simultaneous delamination of old layers. The separated particles affect the mucous membrane, causing an unpleasant reaction.
- Allergy. A burning sensation in the mouth is nothing new for those with intolerance to certain foods, medications, and even denture materials.
- Leukoplakia. Excessive keratinization on any part of the epithelium usually does not provoke tingling sensations, but this disease cannot be excluded from the list of possible persons involved.
- Diseases of the tongue. Desquamative glossitis, or “hairy” tongue, is a common cause of persistent burning sensation in the mouth. The papillae become very sensitive.
- Herpetic infection. The blisters, which quickly transform into erosions, cause severe itching and unbearable burning both in the normal state and when eating.
- Grinding of teeth. Unconscious movements of the teeth during sleep, called bruxism, automatically affects the tongue with the appearance of microtraumas on it, and, accordingly, a burning sensation.
- Lichen planus. Erosive damage to the mucous membrane, white ulcers haunt the patient during an exacerbation, causing severe discomfort.
General factors:
- Unbalanced diet
- Blood diseases
- Hormonal disbalance
- Stomach pathologies
- Nervous disorders
- Avitaminosis
- Insulin-dependent diabetes
- Bulimia
In these conditions, a burning taste in the mouth may appear and disappear, as it is a concomitant symptom.
Types of allergic laryngeal edema
There are acute and chronic allergic edema.
Acute allergic edema
In this case, you must call emergency assistance. Difficulty breathing is obvious and sudden, the condition is rapidly deteriorating. A person breathes intermittently and frequently; the muscles of the shoulders, head and back are involved in breathing, the supraclavicular fossae are sunken, and the intercostal spaces are drawn in. The skin turns pale, blue, the pulse increases, and the patient may begin to panic. In the absence of medical assistance, the lumen of the larynx closes completely, which causes asphyxia and death.
Before the arrival of medical workers, those close to the patient should be advised by telephone what to do. Emergency tips for breathing problems:
- interrupt the person’s contact with the substance that caused such a reaction (if this can be determined);
- in case of food poisoning, rinse the stomach;
- free a person from being squeezed by clothing;
- provide a flow of fresh air;
- give an antihistamine.
Chronic allergic edema
In this case, discomfort in the throat and breathing problems occur periodically, without getting worse, but giving the person very unpleasant sensations. This condition is a consequence of certain diseases or systematic contact with an allergen (for example, mold or animal hair in the house). Its symptoms are as follows:
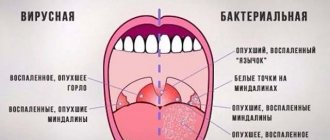
- swelling and redness of the tonsils, uvula and palate;
- difficulty inhaling more than exhaling;
- rapid breathing;
- dyspnea;
- sensation of a foreign body in the throat;
- inability to exercise due to worsening breathing problems.
If you have these symptoms, be sure to consult an otolaryngologist to cure the underlying disease or remove the allergen from your environment.
Chronic allergic edema of the larynx is dangerous because it can sharply and suddenly develop into Quincke's edema - when the increase in clinical manifestations occurs within a few minutes. Quincke's edema is characterized by severe swelling of the neck and face and can spread to the mucous membrane of the larynx, causing severe stenosis. If signs of Quincke's edema appear, you should urgently call an ambulance.
In cases of chronic allergies, the person is usually aware of their condition and should always keep antihistamines on hand to stop the progression of the condition. Such drugs are prescribed by the doctor individually - there are different types of antihistamines, and it is important to choose the ones that suit you.
When the causes of itching are ENT diseases
The most common causes of severe itching in the throat are associated with diseases of the ENT organs:
- sinusitis;
- tonsillitis;
- pharyngitis;
- fungal infection of the pharynx (mycosis).
In each of the above diseases, itching inside the throat is a consequence of exposure to foreign agents on the human mucous membranes.
In case of sinusitis, tonsillitis and pharyngitis, such agents are pathogenic microorganisms that penetrate the larynx, pharynx or nose from the outside. The causes of fungal infection, respectively, are pathogenic fungi.
Bacteria and fungi often inhabit human mucous membranes, but for them to become more active and trigger the inflammatory process, it is enough for favorable conditions to arise for their reproduction. Such “favorable” factors are decreased immunity, hypothermia, stress, and the presence of chronic diseases. Also, a common cause of the development of diseases of the ENT organs is infection of one person from another by airborne droplets or contact-household methods.
Tonsillitis is caused primarily by streptococci. Pathogenic microorganisms settle in the palatine tonsils, causing severe inflammation in them. At the same time, the throat not only hurts greatly, but also itches and itches.
With pharyngitis, the inflammatory process covers the mucous membrane of the pharynx. In this case, the patient complains not only of an itchy throat, but also of a strong dry cough and a feeling of a lump in the throat.
Sinusitis is an inflammation of the maxillary sinuses. A feeling of severe itching in the throat occurs when mucous masses flow from the nasal cavity along the back wall of the pharynx and irritate its mucous membrane.
The main sign of mycosis (fungal infection) is a white coating on the surface of the mucous membrane of the oropharynx. Inflammation is caused mainly by fungi of the genus Candida. Mycosis can be provoked by a sharp decrease in immunity, frequent diseases of the pharynx, diabetes mellitus, and taking antibacterial and hormonal drugs.
The variety of diseases of the ENT organs that cause a feeling of severe itching is quite understandable: all ENT organs are interconnected with each other, and an infection from the nose, for example, easily spreads to the pharynx or ear.
Therefore, it is necessary to treat an ear, nose or throat disease in a timely manner to prevent the development of complications.
Diagnosis and treatment
At the appointment, the doctor collects anamnesis, examines and palpates the larynx. If necessary, bronchoscopy and laryngoscopy procedures, X-rays, and computed tomography are performed.
Allergic swelling of the larynx is treated with medication or surgery. Medicines include antihistamines, which suppress the action of histamine, and glucocorticosteroids, which block the inflammatory response and swelling and suppress the immunological response to the allergen. Surgical intervention is a tracheostomy, an emergency measure when a person is at immediate risk of suffocation - inserting a breathing tube into the trachea through a small incision in the throat.
Doctor MOM® for the treatment of cough and sore throat
In the complex treatment of cough and sore throat, the use of herbal medicines from the Doctor MOM® line - syrup and herbal cough lozenges - is indicated. Thanks to the unique1 “FITO BRONHO formula”2 based on medicinal plant extracts, the products in the Doctor MOM® line have a complex effect, helping to both relieve unpleasant symptoms and eliminate their cause - inflammation.
The main actions of Doctor MOM® syrup and herbal cough lozenges are:
- Eliminating the cause of cough – inflammation;
- Removing infection from the body3;
- Combating unproductive and unproductive cough.
Prevention
As preventative measures, as well as after an attack, it is recommended:
- strengthen immunity;
- perform moderate physical activity;
- use halotherapy and climatotherapy (stay at sea and in the mountains);
- use air purifiers;
- adhere to a diet excluding highly allergenic foods and products containing preservatives and chemical additives.
If you are concerned about breathing problems of any kind, we are always ready to provide assistance, make the correct diagnosis and begin treatment immediately. Call and make an appointment at the Ear, Nose and Throat Clinic!
Treatment options
To effectively treat dryness, sore throat and cough, it is necessary first of all to act on the cause of their occurrence - inflammation. To make an accurate diagnosis, you should consult a doctor who, depending on the anamnesis (history of the development of the disease), complaints and examination, will immediately suggest a particular disease or prescribe additional examinations and consultations. Since dryness, tickling and cough are not a diagnosis, but only one of the symptoms of the disease, it is necessary to carry out comprehensive treatment, and not limit ourselves to just eliminating unpleasant symptoms. Elimination of pathogens.
In case of infectious origin of tickling and cough, therapy is prescribed that acts on the pathogen - antiviral, antibacterial or antifungal drugs for systemic use (orally or by injection, in the form of rectal suppositories). The selection of an antibiotic or antiviral agent is carried out by a doctor. Under no circumstances should you independently cancel and replace one drug with another or stop taking it earlier - this can lead to the progression of the process or its transition to a chronic stage.
Pain relief
. However, cough and severe sore throat, as a rule, are subjectively difficult for patients to tolerate, causing severe discomfort and disrupting their usual way of life. Therefore, it is difficult to do without the use of symptomatic medications to reduce the severity of complaints. For this purpose, a variety of local remedies are used: tablets and lozenges, sprays, rinsing solutions. If your throat is very sore, frequent warm drinks, warming and distracting procedures can help soothe the irritation of the mucous membranes. If you have a painful, obsessive, prolonged non-productive cough, you may need to prescribe antitussive drugs.
What to do if your palate itches
The choice of therapeutic course is determined by the specifics of the provoking disease:
- For minor injuries, drug treatment is not a prerequisite - regular rinsing of the mouth with warm solutions and infusions of medicinal herbs is enough to help relieve swelling and relieve minor suppuration;
- If stomatitis is diagnosed, antiseptic treatment, application of compresses, and the use of ointments and creams for mucous tissues are prescribed;
- Detection of herpes diseases requires treatment with drugs aimed at eliminating viral infections. The most popular include Acyclovir and Zovirax;
- The presence of systemic diseases requires the regular application of anti-inflammatory compresses based on bactericidal drugs, as well as physiotherapeutic procedures.
- Detection of caries requires the appointment of sanitation of the oral cavity, which allows to normalize the condition of the teeth and gums, eliminate deposits of plaque and tartar, and also prevent further spread of the disease.
- Vitamin deficiency is the basis for adjusting the daily diet and strengthening the immune system, providing comprehensive recommendations designed for a long period.
- Formation of a neoplasm on the surface of the palate. In this case, we are talking about serious clinical indications that require mandatory surgical intervention.
Practice shows that choosing the right method for treating palatal itching based on diagnostic results is not particularly difficult - the main thing is to correctly identify the provoking factor. First of all, doctors recommend eliminating the inflammatory process, excluding its further development.
Preventing itching
To avoid the formation of inflammation and infection of the oral cavity, you can follow a number of rules, which include:
- Systematic monitoring of the condition of the oral cavity, teeth and tissues;
- Periodic health rinses;
- Control over the consumption of foods and drinks that are at risk;
- Regular – at least once every six months – visits to the dentist for check-ups;
- Strengthening the immune system, careful handling of hygiene items, and compliance with dental hygiene standards.
Such precautions will help you protect yourself from the occurrence of infection and its subsequent development without much effort.
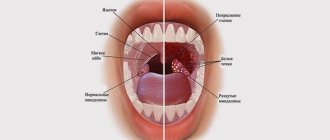
Anatomy of the pharynx
The pharynx is located behind the nasal and oral cavities; begins at the base of the skull and reaches the lower edge of the 6th cervical vertebra, where it narrows in a funnel-shaped manner and passes into the esophagus.
There are three sections of the pharynx:
- upper – nasopharynx
- middle – oropharynx
- lower – laryngopharynx
Nasopharynx
In the nasopharynx there is an accumulation of lymphoid tissue, which forms the pharyngeal tonsil - adenoids. Also in the nasopharynx are the tubal tonsils, which are located around the pharyngeal openings of the auditory tube.
This part of the pharynx is visualized only with the help of instruments or video endoscopic examination.
Oropharynx
The oropharynx is precisely that part of the pharynx that attracts attention when examined by an otolaryngologist and is accessible for examination by the patient himself.
It is located behind the oral cavity and is delimited by the pharynx. The pharynx is an opening formed above by the soft palate and uvula, on the sides by the anterior and posterior arches, and below by the root of the tongue. Between the anterior and posterior palatine arches there are another lymphoid accumulations - the palatine tonsils.
The palatine tonsils, arches, and uvula are subject to friction at the time of swallowing, due to which their mucous membrane may appear redder (hyperemic), in contrast to the entire oral cavity, gums, etc. But this is just a physiological factor.
The mucous membrane of the posterior pharyngeal wall contains elements of lymphoid tissue that visually resemble granules. The mucous membrane of the oropharynx has a dense network of vascular and lymphatic capillaries with rich sensory innervation, and therefore pathological processes are accompanied by symptoms - pain and discomfort in the throat, sensations of dryness, etc.1
hypopharynx
The laryngopharynx begins at the level of the upper edge of the epiglottis and passes into the initial part of the esophagus.
This part is also visualized only using instrumental and video endoscopic methods. This area is visually inaccessible to the patient.
Diseases of the oral mucosa are accompanied by various pathomorphological changes. Inflammation is one of the most common pathological processes of the mucous membrane of the mouth and pharynx and is a manifestation of the body’s protective reaction to the influence of a pathogenic factor. The course and outcome of the inflammatory process depends on the reactivity of the body, localization, activity and duration of action of the pathogenic factor.2