15.06.2018
Increased salivation in an adult is a symptom of inflammation or disease of the gums, teeth or internal organs. It is important not only to eliminate excessive salivation, but also to correctly determine its cause, otherwise the recovery will be temporary.
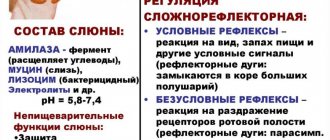
Salivation is considered normal if the volume of saliva does not exceed two liters per day. It is involved in digestion, washing away pieces of food, remnants of drinks and bacterial activity from the teeth. Normally, the process of salivation is invisible to humans - we do not pay attention to it, like, for example, breathing. But if a failure occurs, then too much saliva causes discomfort.
With this disease, saliva accumulates in the mouth too quickly; you constantly have to make sure that it does not leak out and spit. It is inconvenient, unaesthetic, spoils the mood and causes discomfort. In the article we tell you what are the causes of increased salivation in men and women and how to treat it.
How to understand that salivation is increased: symptoms and signs of failure
Saliva is involved in many important processes occurring in the human body. When everything is normal, we do not notice that saliva:
● helps to pronounce words and sounds clearly and correctly;
● enhances the perception of the taste of food and drinks;
● participates in digestion - helps to chew food and also swallow it.
When salivation is increased, several processes are disrupted at once:
● the taste of food changes - salty food becomes too pronounced, and subtle nuances are not felt;
● problems with diction appear – pronouncing some sounds is problematic;
● it becomes painful to swallow food.
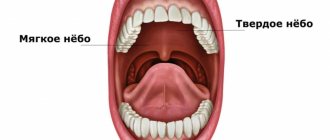
Location of glands
In addition to indirect signs, there are also clear, measurable criteria. If more than two milliliters of saliva is released within five minutes, the patient is diagnosed with increased salivation. The normal value is 2 ml.
Sometimes patients complain of false profuse salivation. This happens when there is injury or inflammation in the mouth and it may seem that there is more saliva than there should be, although the levels are normal: 2 ml in 5 minutes or 2 liters per day.
What are the causes of constant stomach pain?
Constant pain in the stomach often indicates the presence of gastrointestinal disease. Therefore, the causes of pain may be:
- Pancreatitis. With pancreatitis, the patient feels a sharp pain in the upper abdomen. Pain syndromes intensify after eating.
- Cholecystitis,
- Duodenal ulcer,
- Gastritis. Pain appears on an empty stomach and after eating. The cause of gastritis is considered to be irritation of the mucous membrane.
- Food poisoning. Accompanied by nausea and vomiting, frustration, dizziness and headache.
- Stomach cancer. The patient experiences bloody vomiting, rapid weight loss, and bad breath.
Other causes of acute stomach pain:
- Wrong food intake. The appearance of cutting pain after eating is a typical phenomenon for those who eat junk food. If you eat improperly, a large amount of gastric juice is produced and the metabolism in the body is disrupted. You should avoid eating fatty foods, flour, sweets, and alcohol.
- Internal organ injuries.
- Physical exercise. Sports should be done after consulting a specialist.
- Allergy. With allergies, patients experience acute pain in the stomach.
- Infections. For infections of the gastrointestinal tract, the main symptom is acute pain in the stomach.
Specialists from the private medical clinic “KDS Clinic” added that the state of the gastrointestinal tract is affected by the emotional state of the patient, the presence of stress and stress on the nervous system. The systems of the human body are interconnected.
Causes of increased salivation in men and women
The volume of saliva secreted is controlled by the nervous system. When everything is in order with health, it happens naturally and unnoticed by a person. But when problems arise or diseases appear, the process is disrupted. A variety of factors can influence, but most often the cause of increased salivation in adult men and women is one of six factors.
- Oral diseases - gum inflammation, periodontitis, stomatitis, as well as cuts and burns. When bacteria enter the glandular tubules, the body begins to produce more saliva to get rid of them. This is a natural reaction.
- Digestive system problems - abnormal stomach acidity, pancreatic and liver diseases.
- CNS diseases - Parkinson's disease, trigeminal nerve damage, bulbar syndrome, migraine. With these diseases, the natural process of salivation is disrupted. Short-term impairment may occur due to air sickness, seasickness, or problems with the vestibular apparatus.
- Hormones - failures of the hormonal system, in particular the thyroid gland, menopause, diabetes mellitus lead to excessive salivation. Sometimes this is observed in adolescents during the restructuring of the body.
- Smoking and removable dentures can also affect it. Both of these phenomena irritate the mucous membrane, stimulating the overactive functioning of the glands.
- Taking medications - some medications have side effects of increased salivation or, as it is also called, hypersalivation. Most often these are those medications that contain iodine or mercury. For example: lithium, physostigmine, muscarine.
Pilocarpine, nitrazepam also lead to hyperactivity of the glands
What to do with increased salivation depends on the factors that caused it. In some cases, for example, when taking medications, the disease will go away without the intervention of a doctor.
The role of gastroesophageal reflux disease in the course of chronic pharyngitis
Many works are devoted to the issues of diagnosis, clinical course and treatment of chronic pharyngitis. Most of them describe new methods of examination and treatment. However, the number of patients with chronic pharyngitis at appointments with ENT doctors is not decreasing.
Chronic pharyngitis is a common polyetiological disease characterized by inflammatory-dystrophic changes in the mucous membrane of the posterior pharyngeal wall [4].
Depending on the pathomorphological changes, catarrhal, hypertrophic, subatrophic and atrophic pharyngitis are distinguished. A mixed form of chronic pharyngitis is often found.
Patients with chronic pharyngitis complain of a sore, tickling sensation in the throat, increased salivation, which necessitates frequent coughing and expectoration of accumulated contents. At the same time, dryness in the throat, a feeling of incomplete swallowing of food, and the “lump symptom” may be disturbing [6].
The disease is painful for patients. Patients repeatedly seek medical help from various specialists and undergo multiple courses of treatment. However, most of them never receive real help and are left alone with their problems.
Many domestic and foreign works have studied in detail the influence of waste products of various microorganisms and viruses on the mucous membrane of the oropharynx. However, this etiological factor is not the root cause of the disease, i.e. the occurrence of chronic pharyngitis depends not so much on the nature and virulence of the microorganism, but on the degree of disruption of the biochemical processes of both the mucous membrane and the body as a whole [4].
According to A.Yu. Ovchinnikov, chronic pharyngitis in most cases is a disease of a non-infectious nature, since the qualitative and quantitative composition of the microflora sown from the mucous membrane of the pharynx in patients with chronic pharyngitis differs little from that in persons with normal condition of the mucous membrane of the oropharynx [5].
The true causes of the disease are far from understood. Obviously, further work and the introduction of new modern views and research methods into clinical practice are necessary.
An equally important and common problem is chronic cough. About a third of patients seeking medical help complain of chronic cough.
Physiologically, coughing is a protective reflex aimed at removing excess secretions, dust or smoke from the respiratory tract. This is a quick strong exhalation, as a result of which the tracheobronchial tree is cleared of foreign bodies [8, 9].
According to the Richard S. Irvin classification of 2000, acute cough is considered to be a cough lasting no more than three weeks (most often against the background of an acute viral infection), subacute cough lasting more than three but less than eight weeks, chronic cough more than eight weeks [8, 9] .
Despite the fact that cough is often associated in patients with pathology of the bronchopulmonary system, it can occur in a number of diseases, varied in their pathogenesis and location of damage [4].
Richard S. Irvin in 1990 conducted a prospective study of the causes of chronic cough. As a result, several diseases were identified that are characterized by chronic cough. Of those examined, 54% were diagnosed with postnasal drip syndrome, 31% had bronchial hyperreactivity, 28% had gastroesophageal reflux, 7% had chronic bronchitis, 12% had other causes of cough, and In almost 10% the cause could not be determined. Moreover, almost a quarter of those examined had two causes of cough, and 3% had three causes.
Currently, the problem of gastroesophageal reflux disease (GERD) and its extraesophageal manifestations has increasingly begun to be raised at world gastroenterological forums. Interest in this problem is not accidental. Foreign colleagues have identified and are actively studying the relationship between the pathology of the upper respiratory tract and gastroesophageal reflux.
The term GERD is used by most clinicians and researchers to denote a chronic relapsing disease caused by spontaneous, regularly recurring retrograde entry of gastric and/or duodenal contents into the esophagus, leading to damage to the distal esophagus and/or the appearance of characteristic symptoms (heartburn, retrosternal pain, dysphagia) [7, 3, 2], which basically allow one to suspect GERD in a patient. However, in some patients the disease has less typical manifestations - reflux-associated cardiac, pulmonary and ENT organs. They are often underestimated, especially in the absence of specific symptoms of GERD, which can lead to underdiagnosis and incorrect patient management tactics.
According to the International Classification of Gastroesophageal Reflux Disease adopted in Montreal in 2006, chronic pharyngitis is one of the presumed extra-esophageal manifestations of gastroesophageal reflux disease. There is currently no substantiated evidence of this relationship.
The purpose of the work is to develop an algorithm for the examination and treatment of patients with chronic pharyngitis, to evaluate the effectiveness of antireflux therapy in the treatment of chronic pharyngitis.
The patients we observed were examined before the start of treatment, as well as during the treatment process. Immediate results were assessed no earlier than two months after the start of therapy directly by the patients themselves (who were offered a specially designed questionnaire), as well as using the above objective methods.
In the course of the study for the period 2005-2006. We examined 37 patients with chronic pharyngitis aged from 19 to 70 years who applied for a consultation at the Moscow Regional Clinical Hospital. Among them there were 14 men, 23 women. 17 patients suffered from chronic subatrophic pharyngitis, chronic catarrhal pharyngitis occurred in 11 people, hypertrophic pharyngitis in 9. The patients were divided into three groups; the first group consisted of 16 patients who were diagnosed with GERD with high gastroesophageal reflux , the second group was 8 patients with GERD without high pathological reflux, the third group was 13 patients in whom there was no evidence of GERD based on the results of 24-hour pH monitoring. Thus, among the patients with chronic pharyngitis we examined, 24 people suffered from GERD (Tables 1, 2).
In our study, in seven patients we observed reflux-esophagitis grade A, in two - grade B. At the same time, one patient with reflux-esophagitis grade B had high alkaline reflux. Among our patients there was not a single one with reflux esophagitis of degrees C and D.
Our study revealed pH fluctuations from 2.0 to 8.5 at the level of the upper third of the esophagus.
After 24-hour pH monitoring when the diagnosis of GERD was made, antireflux therapy was included in the standard treatment of chronic pharyngitis. Therapy was carried out for at least two months. During therapy, there is a significant improvement in the course of chronic pharyngitis, as well as in 24-hour pH monitoring data, while numerous courses of standard treatment for chronic pharyngitis for these patients turn out to be ineffective.
Preliminary results allow us to judge the significant pathogenetic role of GERD in the development and course of pharyngitis. In this regard, we believe that:
- patients under the supervision of an otorhinolaryngologist with a diagnosis of chronic pharyngitis should be consulted by a gastroenterologist.
- all patients with chronic pharyngitis require fibroesophagogastroduodenoscopy
- If endoscopic signs characteristic of GERD are detected, daily high pH-metry is indicated
- 24-hour pH measurements should be performed in patients who clinically do not respond to standard therapy for chronic pharyngitis, regardless of the presence of complaints characteristic of GERD and endoscopic findings in the esophagus.
D.M. Mustafaev, Z.M. Ashurov, V.A. Isakov, V.G. Zenger, S.V. Morozov, S.G. Tereshchenko, V.L. Shabarov, N.G. Lyubimova, A.S. Epanchintseva, L.V. Gibadullina.
Moscow Regional Scientific Research Clinical Institute named after. M.F. Vladimirsky, Moscow (director - senior doctor of sciences of the Russian Federation, corresponding member of the Russian Academy of Sciences and the Russian Academy of Medical Sciences, professor G.A. Onoprienko)
Increased salivation in women during pregnancy
A common cause of hypersalivation in women is pregnancy. When a woman is preparing to become a mother, the hormonal background of the body changes greatly, and with it many processes: blood circulation, digestion.
Pregnancy affects all systems at once:
● endocrine;
● nervous;
● digestive.
Often, expectant mothers experience problems with their teeth and gums, such as gingivitis. This disease also affects the amount of saliva produced.
Healthy and inflamed gums
Causes of increased salivation at night in adults
During sleep, processes in the body go slower, including the secretion of saliva. But glitches may occur. Here are the main factors that cause too much saliva to be produced during sleep:
● breathing through the mouth, not through the nose - often happens when a person sleeps on his back;
● malocclusion – the mouth remains open during sleep, the tongue dries out and the body decides that more saliva is needed;
● poor sleep - too much sleep when a person is not sure that he is sleeping. This can lead to the body considering the dream as reality and secreting saliva as if during the day.
This is what an open bite looks like - the tongue protrudes forward
Salivation during sleep
Sometimes, when a person wakes up, he notices wet spots on the pillow. This usually happens due to extreme fatigue and sound sleep. However, if salivation during sleep becomes a pattern, you should consult a doctor.
The main factors that provoke the secretion of saliva during sleep.
- Malocclusion or missing teeth. Saliva flows out because the teeth do not close completely.
- Difficulty in nasal breathing: runny nose, deviated nasal septum, colds. All this forces you to breathe through your mouth. Since the lips do not close, the accumulated fluid flows out. This is often accompanied by snoring.
- Deep sleep.
Treatment of increased salivation
Depending on the cause of hypersalivation, different doctors provide treatment:
● dentists solve problems of local oral diseases;
● endocrinologists for hormonal disorders;
● gastroenterologists, if the problem is diseases of the digestive system;
● neurologists, if the failure is due to problems with the central nervous system.
A dentist will help identify the cause, and a therapist will refer you to a specific specialist.
Treatment with medications
In addition to eliminating the causes associated with disruption of the internal organs, the doctor may prescribe medications that eliminate the symptoms. For example:
● riabal;
● scopolamine;
● platiphylline.
Taking medications without a doctor's prescription is prohibited!
We do not recommend purchasing or taking medications without consulting a doctor. Each drug has contraindications and side effects: from glaucoma to liver, heart, and vascular diseases.
You should not risk your life and health to save time or money on a visit to the clinic.
Botox treatment
For short-term symptom relief, Botox injections are sometimes used. It blocks nerve signals, reducing tubule activity. This method helps to quickly get rid of the problem, but, unfortunately, the effect does not last long.
Facial massage and muscle relaxation
It will help if the cause is related to nervous tension, stress or central nervous system pathologies.
Removal of glands
It is prescribed extremely rarely, only in cases where all other methods and elimination of the causes of the disease have not helped. Removal, even partial, can damage the facial nerves.