The most common form of gingivitis is catarrhal gingivitis, which affects the gums, causing superficial inflammation. Most often, this disease affects children and young people under 35 years of age. In older patients, as a rule, chronic catarrhal gingivitis is diagnosed.
Teeth polishing with pastes - 1,200 rubles.
Polishing one tooth with paste - 50 rubles.
Coating with a fluoride-containing product (1 row of teeth) - RUB 1,500.
Coating with fluorine-containing varnish (1 tooth) - 250 rubles.
Retraction of hypertrophied gums in the area of 1 tooth - 600 rubles.
At CELT you can get advice from a dental specialist.
- The cost of a dental consultation is 1,000
- The cost of an orthodontist consultation is 2,000
Make an appointment
Causes of gingivitis
Gingivitis does not always progress as a separate disease. It often appears in the background:
- Imbalance in the hormonal system.
- Disturbances in the gastrointestinal tract.
- Diseases of the cardiovascular system.
- Infections and inflammatory processes.
Internal factors in the development of pathology are as follows:
- Fall of immunity.
- Growth of wisdom teeth.
- Lack of vitamins P and C.
- Allergy.
- Diabetes.
- Metabolic disorders.
- Chronic gastrointestinal diseases.
- Severe mental disorders.
Among the external causes of gingivitis:
- Smoking or improper breathing.
- Burns and mechanical damage to the mucous membrane.
- Incorrect installation of the seal.
- Irregular brushing of teeth.
- Infections.
In more than 50% of cases, the development of pathology occurs due to pathogens that penetrate the oral cavity with food and liquid. If you brush your teeth incorrectly and irregularly and do not use floss, a thick plaque will appear. Often inflammation begins due to a burn or mechanical damage to the gums. A lack of nutrients in the diet and serious stress can reduce immunity, which will also lead to the development of pathology.
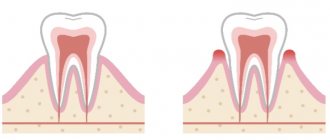
Acute gingivitis
The clinical picture of acute gingivitis gives classic signs of inflammation: swelling, redness, local increase in gum temperature, pain, disruption of normal gum function. Against this background, bleeding gums and even ulceration are observed. The general condition, with rare exceptions, is not impaired. Upon examination, inflammation of the gum tissue is determined, which extends either to the interdental gingival papillae (papillary gingivitis) or to the marginal gum (marginal gingivitis). The papillae, margin and attached gingiva may be affected (diffuse gingivitis). The intensity of inflammation varies from slight to pronounced. False periodontal pockets may occur due to swelling of the gums. The presence of deposits in the form of tartar or plaque is noted. In the acute form, the gum surface is smooth, shiny, bright red, swollen, and bleeds easily upon probing.
There are: Acute gingivitis caused by dental plaque. This group of gingivitis includes forms that can be caused by: microbial infections, systemic factors, medication, mechanical, thermal and chemical damage.
Gingivitis simplex acuta (simple acute gingivitis) Simple acute gingivitis is a form of gingivitis accompanied by a classic acute inflammatory reaction in response to physical and microbial damage.
Acute necrotizing ulcerative gingivitis This disease, also called Gingivitis acuta ulcerosa necroticans (Plauta-Vincet gingivitis), is characterized by pain, necrosis of the interdental gingival papillae and lymph node reaction. Progressive stages are characterized by the formation of craters with exposed alveolar bone. If left untreated, this disease can progress through necrotizing ulcerative gingivitis-periodontitis into ulcerative stomatitis, and then, in the form of Cancer oris or Noma, lead to death. If the disease is not stopped in time, an irreversible process of tissue loss occurs.
Gingivitis specifica acuta (acute specific gingivitis) Acute specific gingivitis includes specific infectious diseases of the gums as a result of exposure to tuberculosis bacteria, Candida albicans, Actinomyces israelii, Treponema pallidum.
Acute viral gingivitis Gingivitis is caused by herpes simplex viruses, as well as Herpes zoster and cytomegaly.
Gum abscess Gum abscess is an acute disease of the upper gums and leads to purulent melting of the interdental papillae and gingival tissue with the appearance of severe pain.
Complications and outcomes. Acute local gingivitis, when the cause that caused it is eliminated, can result in recovery. Acute generalized gingivitis, when the disease of which it is a complication is eliminated, also usually disappears. Chronically ongoing catarrhal, ulcerative and hypertrophic gingivitis is often a prestage of periodontitis.
Symptoms of catarrhal gingivitis
The sooner treatment for acute catarrhal gingivitis begins, the lower the risk of subsequent complications. Symptoms that should promptly contact your dentist include the following:
- bleeding, redness and swelling of the gums;
- itching in the gums;
- increased body temperature;
- bad breath, unpleasant taste;
- pain in the gums when eating or pressing on them;
- general malaise, fatigue.
Indications
You need to immediately begin treatment for catarrhal gingivitis if you find:
- Swelling of the gums.
- Bleeding after eating or brushing teeth.
- Acute pain and burning in the gum area.
- Bad breath.
- Putrid or bloody taste in the mouth.
- Changes in gum color and density.
Contraindications
It is not recommended to start treatment if you have:
- Psychological and nervous diseases.
- Cardiovascular pathologies.
- Problems with blood clotting.
- Chronic diseases in the acute stage.
- Allergic reactions to anesthesia.
A specialist will give you a full list of contraindications during a face-to-face consultation.
History of the disease
When collecting anamnesis, it was established that gums have been bleeding when brushing teeth or biting off hard food for several years; the patient does not observe individual oral hygiene (brushing teeth once a day). According to the patient, the last time he visited the dentist was 2 years ago. The patient himself associates severe pain in the gums with a recent flu.
Previous and concomitant diseases
Allergological anamnesis is not burdened. The patient denies the presence of hepatitis, HIV, herpes virus, cardiovascular diseases, disorders of the nervous system, digestive and respiratory systems. As a child, he suffered from acute respiratory diseases. 2 weeks ago I had the flu.
Bad habits - smoking.
Forms of catarrhal gingivitis
Depending on the nature of the lesion, there are:
- acute catarrhal gingivitis - characterized by rapid development and one-time inflammation, limited in time;
- chronic catarrhal gingivitis is a continuation of acute; in the absence of treatment, it is practically asymptomatic, but with regular exacerbations.
The scale of inflammatory processes determines two forms of gingivitis:
- localized - part of the gum is inflamed, no more than 1 - 3 teeth;
- generalized - the entire gum on one or both jaws is inflamed.
The severity of the disease is as follows:
- mild - the periodontal papillae are affected;
- medium - the free area of the gums is affected;
- severe - the alveolar region of the gum is affected.
Catarrhal stages
For this form there are stages:
- acute - characterized by the rapid onset and development of the disease, significant bleeding and pain, bright red color of the mucous membranes near the tooth root;
- chronic - the color acquires a bluish tint, symptoms appear slowly, and there is no pain during brushing, and exacerbation is associated with decreased immunity.
Due to the low level of symptoms and the widespread sluggish form, the patient does not attach sufficient importance and does not increase the level of sanitation. Until the symptoms turn into significant problems.
Treatment of catarrhal
Effective treatment of catarrhal gingivitis begins with professional hygienic cleaning using ultrasound technology in a dental clinic by a specialist.
At the same time, preventive cleansing must be carried out every six months for each patient, regardless of the presence of gingivitis. This is due to the fact that food and bacteria can get into the invisible part of the tooth under the gum, causing the formation of hard stone that cannot be removed with an ordinary toothbrush, floss or brushes.
After cleaning, the doctor will recommend rinsing the mouth with a chlorhexidine solution (has an antiseptic effect) or special liquids for the oral cavity, as well as using an antibacterial gel twice a day (for example, Cholisal).
Important! Before applying the gel, to ensure absorption, dry the gums with a cotton swab or pad. In this case, the gel will better adhere to the gums. During application, saliva will form, no need to spit, swallow, because the gel is harmless to the stomach. After Cholisal, do not eat for 2 hours and do not drink liquids for 30 minutes.
During treatment, experts recommend using a soft brush to avoid additional injury to the inflamed gums. In normal times, medium hardness is recommended to ensure sufficient removal of contaminants.
Hypertrophic gingivitis
Refers to forms of the disease when the cause lies not only in violation of hygiene procedures, but in concomitant diseases or changes affecting the body.
Characteristic signs are an increase in gum volume, which is associated with a chronic form or fibrosis of connective tissues. The teeth in the front row are most susceptible.
Causes:
- hormonal changes in the body - pregnancy, menopause, hormonal changes in adolescents;
- disruptions of the endocrine system or other hormonal imbalances;
- malocclusion;
- poorly installed fillings (overhanging edges).
Attention! Hypertrophic gingivitis is associated with chronic processes that occur asymptomatically, aggravated by exacerbation of other diseases.
Hypertrophic forms
Stages:
- edematous - the peculiarity lies in the structure of the gum papillae, which increase not due to inflammation caused by plaque, but due to loose swelling (occurs with hormonal changes);
- fibrous - a change in the size of the gum occurs due to the growth of fibrous tissue due to the influence of traumatic factors (overhanging filling, crown or malocclusion), in this case the gum becomes dense.
Treatment of hypertrophic
Actions to combat this form are aimed at eliminating the causes that caused the disease as a consequence - normalizing or maintaining hormonal levels, high-quality dental fillings, installing suitable implants and correcting the bite.
However, regardless of the strength of the symptoms, hygienic sanitation in the dental clinic is mandatory. Further, if necessary, anti-inflammatory therapy is prescribed to reduce pain and relieve swelling from the gums:
- a course of sclerosing injections into the gums;
- pads with heparin ointment for healing;
- tissue excision.
In the absence of the necessary timely treatment, the edematous form will transition to fibrous.
Ulcerative gingivitis
Vincent's gingivitis is a severe form, accompanied by the accumulation of a critical mass of microbes under the gums and on the gingival surface and necrotic tissue death with the formation of ulcers against the background of a general decrease in oral immunity.
This disease is caused by:
- poor hygiene;
- decreased immunity;
- exacerbation of chronic diseases.
Diabetes mellitus, AIDS, vitamin deficiency, leukemia - a list of some diseases that cause the ulcerative form of gingivitis.
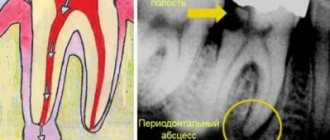
Diagnosis of the disease
Diagnosis of catarrhal gingivitis involves examination by a doctor and laboratory tests.
The latter allow you to determine indicators such as:
- bleeding gums;
- degree of inflammation;
- amount of microbial plaque.
When conducting an examination, the dentist pays special attention to the following factors:
- how full the blood vessels of the gums are;
- red gums;
- integrity of the periodontal junction;
- the presence and amount of plaque and tartar;
- presence of signs of destruction of the interalveolar septa.
Types of gingivitis
Based on how the disease progresses, the following types of gingivitis are distinguished:
- Acute - when it appears suddenly and its course sharply intensifies.
- Chronic - the inflammatory process proceeds slowly and the condition worsens gradually.
- Aggravated gingivitis - an increase in symptoms of chronic inflammation.
- Gingivitis in remission is a state of subsidence of symptoms.
According to the form, it is customary to distinguish the following types of gingivitis:
- catarrhal, manifested by swelling and redness of the gums;
- ulcerative, when dead areas of gum appear;
- hypertrophic, characterized by a sharp increase in gums and bleeding;
- atrophic, manifested in thinning of the gums;
- desquamative, characterized by redness and severe detachment of the upper layer of the mucosa.
According to the degree of prevalence in the oral cavity, gingivitis is divided into local (partial) and generalized (extensive).
Treatment of the disease
Treatment of chronic catarrhal gingivitis involves a set of measures aimed at eliminating the already emerging consequences of the disease, as well as the causes that caused it. Typically, it begins with a professional teeth cleaning at the dentist's office.
The course of treatment is selected individually and depends on the form, severity and nature of the disease. Often the patient is prescribed mouth rinsing with antiseptic solutions and the oral cavity is sanitized. It involves treating caries, filling teeth, and replacing incorrectly installed fillings. This approach eliminates the possibility of relapse of the disease in the future.
Drug therapy consists of treating the oral cavity with antiseptic solutions and applications of special ointments. When treating the chronic form, it is possible to massage the gums.
It is worth noting that treatment is often carried out in combination with a diet that excludes foods that irritate the gums and is rich in vitamins A, B, E.
Treatment of chronic catarrhal gingivitis of any severity has been successfully carried out by dentists at the CELT clinic for several years now.
Gingivitis in adults: causes of the disease
The disease, which affects all categories of people (children, adults, pregnant women), occurs primarily due to weakened immunity and poor oral hygiene.
The development of the inflammatory process occurs at a low speed, so the disease is often not noticeable for a long time to an ordinary person who is far from dentistry. However, if you do not consult a doctor in a timely manner, serious complications may develop, which can lead to a more painful course of the disease and lengthy treatment.
There are three stages of development of gingivitis:
- mild (the disease affects only the spaces between the teeth);
- medium (the disease affects the edge of the gum);
- heavy.
The more time passes without treatment, the further the lesion spreads, eventually covering the oral mucosa.
The causes of the disease are divided into internal and external.
External ones include:
- injuries;
- burns of the oral cavity;
- influence of radiation;
- effects of heavy metals on the human body.
The internal reasons are as follows:
- development of molars (often during their growth, soft tissues are injured, which causes bleeding);
- lack of vitamins and minerals in the diet, which leads to decreased immunity;
- gastrointestinal diseases;
- various infections;
- neglected carious formations.
Recommendations after treatment
To avoid the occurrence of catarrhal gingivitis after treatment, you need to follow 7 rules:
- Lead a healthy lifestyle and support your immune system. Consume a vitamin-mineral complex and a sufficient amount of proteins, carbohydrates and fats.
- Prevent the transition of chronic diseases to the acute stage. Treat chronic diseases of the cardiovascular and hormonal systems, gastrointestinal tract.
- At least 2 times a year, carry out professional cleaning of the oral cavity to remove soft and hard plaque and prevent the formation of tartar.
- Use a toothbrush with medium hardness. Too soft does not sufficiently clean teeth from plaque, and hard ones can injure the enamel and cause pain with high sensitivity.
- Properly clean the oral cavity and the space between the teeth using floss and irrigator.
- Visit the dentist regularly in order to promptly detect inflammatory processes and eliminate them at an early stage.
- Choose the right toothpaste with sodium, fluoride, potassium nitrogen and other components. Entrust this task to your doctor.
If you follow these recommendations after treatment, you will confidently avoid a recurrence of catarrhal gingivitis.
Make an appointment through the application or by calling +7 +7 We work every day:
- Monday—Friday: 8.00—20.00
- Saturday: 8.00–18.00
- Sunday is a day off
The nearest metro and MCC stations to the clinic:
- Highway of Enthusiasts or Perovo
- Partisan
- Enthusiast Highway
Driving directions
How and with what to treat catarrhal gingivitis?
Diagnosis of catarrhal gingivitis is not difficult; chronic gingivitis is clearly visible to the naked eye. To be sure, you can do a number of specific tests - and when they confirm the diagnosis, prescribe treatment. It will consist of the following stages.
- Eliminating the cause of gingivitis. This could be cleaning teeth from plaque and tartar, removing an incorrect filling, reinstalling a denture, taking a course of vitamins, etc. Very often, signs of gingivitis begin to disappear without a trace immediately after the removal of tartar.
- If recovery is slow, rinsing with a disinfectant solution is prescribed - usually a 0.06% chlorhexidine solution, but there may be other antiseptics - at the discretion of the doctor. Gargles with medicinal herbs and medicinal applications to the gums of chlorophyllipt, propolis, and special ointments can also be prescribed.
- If this is not enough, treatment is carried out with antibiotics, non-steroidal anti-inflammatory drugs, as well as gum massage, electrophoresis, etc.
There are also folk methods for treating chronic catarrhal gingivitis - rinsing with natural antiseptics brewed in milk - chamomile, sage, oak bark infusion. But you need to keep in mind that these medications alone will not eliminate the cause of gingivitis, so it will start again and again until you see a dentist. However, such remedies are excellent for consolidating the resulting therapeutic effect and preventing relapses of the disease.
There is another method of treating chronic gingivitis - injections of autoplasma containing platelets. So far, this method is rarely used as research into its effectiveness continues.
How to treat gingivitis in each specific case, and how long the treatment process will last, should be determined by the dentist. After all, the patient can be content with the disappearance of external signs of gingivitis, while the inflammatory process will continue, threatening complications.
If you have a problem similar to that described in this article, be sure to contact our specialists. Don't diagnose yourself!
Why you should call us now:
- We will answer all your questions in 3 minutes
- Free consultation
- The average work experience of doctors is 12 years
- Convenient location of clinics
Single contact phone number: +7
Make an appointment