Metastases in the bones can develop in absolutely any malignant process; for some cancers this is an almost obligatory localization, while for other diseases it is rare. In the metastatic ranking, first place in terms of frequency of occurrence will go to lung metastases, second to liver foci, and third to skeletal metastases.
Metastases in the bones are difficult to treat and promise pain; however, skeletal foci, less than other tumor localizations, shorten life, but can ruin it with a fracture or compression of the spinal cord.
- What types of bone metastases can there be?
- What cancers develop?
- When do skeletal metastases appear?
- Which parts of the skeleton are most often affected?
- Clinical manifestations of bone metastasis
- Why does pain occur?
- How are bone metastases detected?
- Treatment of skeletal lesions
- Why are bisphosphonates needed?
What types of bone metastases can there be?
According to clinical and radiological characteristics, all bone lesions are divided into three groups:
- osteoblastic - with a predominance of compaction beyond the physiological measure, but additionally grown tumor tissue does not impart strength to the bone and can compress the nerves passing nearby;
- osteolytic - destruction of the structure prevails and the likelihood of a fracture increases as the cancer grows;
- mixed - a combination of two types and this situation occurs most often.
It almost never happens that a patient has exclusively osteolytic or only osteoblastic foci; as a rule, a combination with a predominance of either a sparse lytic or an excessive blastic structure is diagnosed.
What cancers develop?
The leader among all malignant processes occurring with metastatic lesions of the skeleton is myeloma - bone destruction begins at the very beginning of the disease and in 100% of clinical cases multiple destruction of bone tissue is noted.
In case of breast and prostate cancer, skeletal metastases are diagnosed in two thirds of patients, and pathological observations reveal the involvement of bones in the malignant process in almost 90% of patients. In breast cancer (BC), mixed and osteolytic variants predominate; in prostate cancer, osteoblastic variants predominate.
A high frequency of bone metastases is observed in lung cancer, but in the small cell variant there are twice as many bone defects, while in the non-small cell variant it occurs in 40% of patients with a tendency towards single or solitary lesions, that is, a single one.
Every fourth person suffering from kidney cancer has skeletal metastases; in bladder carcinoma, bone tumors are much less common.
In case of colon cancer, bone metastasis is detected in every eighth patient, in case of stomach cancer - not often, since the cancer affects the liver and abdominal cavity earlier and more abundantly. Colon cancer tends to be small-focal and multiple secondary formations.
Book a consultation 24 hours a day
+7+7+78
When do skeletal metastases appear?
In malignant processes, the time of appearance of bone metastases varies, while the rate of growth of the lesion depends solely on the individual biological characteristics of the tumor tissue, which change under the influence of treatment and as cancer disseminates.
At the initial treatment, bone lesions in the absence of other manifestations of the cancer process are present in hardly 20% of patients; in the vast majority of cases, tumor lesions of the bones are a sign of cancer dissemination—spread across systems or generalization. This is exactly what happens with breast cancer, non-small cell lung carcinoma and colon cancer.
In prostate cancer, skeletal pathology is often detected simultaneously with a prostate tumor or shortly after the diagnosis of problems in the gonad.
In kidney carcinoma, metastases are often first found in the bones and lung tissue, and then the primary tumor is discovered.
Destructive changes in the spine
Bone destruction is a dangerous process, the further development of which must be prevented at the first signs of pathology. Destructive changes affect not only the bone tissue of the tooth; without appropriate treatment, they can spread to other bones in the body. For example, as a result of the development of spondylitis, hemangiomas, destructive changes affect the spine as a whole or the vertebral bodies separately. Spinal pathology can lead to undesirable consequences, complications, partial or complete loss of mobility.
Spondylitis is a chronic inflammatory disease that is a type of spondylopathy. As the disease develops, pathology of the vertebral bodies and their destruction are noted, which threatens spinal deformation.
There is specific and nonspecific spondylitis. Specific spondylitis is caused by various infections that enter the blood and, with its help, spread throughout the body, affecting bones and joints along the way.
Infectious pathogens include microbacteria:
- tuberculosis;
- syphilis;
- gonorrheal gonococcus;
- coli;
- streptococcus;
- Trichomonas;
- Staphylococcus aureus;
- pathogens of smallpox, typhoid, plague.
Sometimes the disease can be triggered by fungal cells or rheumatism. Nonspecific spondylitis occurs in the form of hematogenous purulent spondylitis, ankylosing spondylitis or ankylosing spondylitis.
Regardless of the cause of the disease, treatment must begin immediately after diagnosis.
Which parts of the skeleton are most often affected?
The localization of bone metastases is determined not by the nosological affiliation of the primary malignant tumor, but by the functional load and the associated development of the blood supply. Multiple foci in the skeleton are more typical for highly aggressive cancer, single and especially one metastasis indicates a favorable prognosis of the disease.
- Most often, secondary cancer screenings occur in the spongy bones, the vertebrae, which are abundantly fed with blood, and mainly in the lumbar and thoracic spine, which are under high load.
- Next in frequency are metastases in the pelvic bones - almost half of all cases, typical locations are the ilium and pubic bones.
- Metastasis is half as common in the bones of the skull and lower extremity, where damage to the femur predominates.
- The chest, mainly the ribs and sternum, are involved in the malignant process in almost 30% of cases.
Psychological support
Cancer is always a serious stressful situation associated with a strong negative emotional shock. A person who is faced with this disease should be surrounded by his family and friends and provide him with full support. In addition, professional psychological assistance is also important, which can be obtained in special groups and from specialists in the form of counseling. The main thing is that a person should not be left alone with his illness. Anadolu doctors are well aware of the importance of psychological support, so the patient can always count on a caring and attentive attitude.
The material was prepared in agreement with Anadolu physician and medical oncologist Yeshim Yildirim.
Clinical manifestations of bone metastasis
Contrary to popular myths, skeletal metastasis often occurs without significant pain and even without symptoms at all. Osteoblastic lesions are less often accompanied by pain than osteolytic lesions.
Dangerous manifestations of metastatic bone lesions:
- hypercalcemia - a significant increase in calcium concentration due to the destruction of the bone matrix leads to a severe condition that requires correction of metabolism, essentially resuscitation measures;
- fracture - destruction of half the diameter of a bone or vertebra is sufficient to cause it; every eleventh patient with a pathological fracture requires urgent surgical care;
- syndrome of compression or compression of the spinal cord by fragments of a broken thoracic or lumbar vertebra, complicated by severe neurological disorders below the damage zone;
- impairment of motor activity up to paralysis is possible when the spinal cord is compressed in the cervical region by an osteoblastic lesion or damaged by fragments during lytic destruction.
Complications of bone metastasis have a fatal impact on the patient’s condition and actively interfere with adequate treatment, which can shorten life expectancy with an absolute lack of quality.
Prevention measures
Due to the special diagnostic method, greater accuracy in detecting changes in density is possible.
There is an ultrasound technique called densitometry. Thanks to this technique, even minimal indicators of density reduction can be determined. Other hardware interventions are ineffective in the early stages. For comparison: an X-ray machine will show a result of twenty-five to thirty percent.
Experts discuss some signs that indicate the progression of this disease: a decrease in height of more than ten millimeters, the vertebral part is curved, the lower back and thoracic part hurt, especially during active physical activity, you get tired quickly, and your performance is minimal.
An active life is the best preventative measure for the development of this disease. This:
- balanced diet: correct ratio of proteins, fats, carbohydrates, large amounts of fresh vegetables and fruits;
- walking in clean air;
- morning exercises, physical training, not for wear and tear;
- minimizing bad habits such as cigars, alcoholic beverages and drinking coffee drinks;
- relaxing and toning massages.
Note! Before selecting exercises, approach it consciously; it would not be superfluous to consult a doctor or a fitness instructor. Over the course of several months of combining a balanced diet with moderate physical activity, inert mass increases by several percent.
Why does pain occur?
Pain is caused by three reasons:
- destruction of the richly innervated periosteum by a cancerous conglomerate;
- irritation of pain receptors in the periosteum by biologically active waste products of cancer cells;
- involvement of muscle nerve endings in the metastatic node.
Unbearable pain is not always associated with skeletal metastasis; as a rule, this is a consequence of the high aggressiveness of tumor cells in the terminal stage of the process, when the concentration of biologically active substances in the blood is enormous - cytokines, which literally “burn” the nerve endings of even tissues not affected by the tumor. With a high degree of malignancy of the primary tumor, pain is observed more often and more intensely. The most obvious example is widespread and persistent pain in completely intact bones due to lung adenocarcinoma; surgery to remove the affected lung completely cures the pain.
Stages of multiple myeloma
Stage 1 - characterized by mild anemia, calcium remains within normal values, M-protein is low, the number of bone lesions is no more than 5.
Stage 2. Moderate anemia (hemoglobin within 85-100 g/l), there is an increase in calcium (up to 3 mmol/l) and M-protein. There is also an increase in the number of osteolysis foci. For the second stage, their number should not exceed 20.
Stage 3 multiple myeloma is diagnosed when at least 1 of the following symptoms is detected:
- Hemoglobin is below 85 g/l, which corresponds to severe anemia.
- Exceeding the calcium value by more than 3 mmol/l.
- M-protein level is more than 70 g/l.
- The number of bone lesions is more than 30.
How are bone metastases detected?
Diagnosis of skeletal injuries is not complicated, but high-tech, they begin with an isotope examination - osteoscintigraphy, which reveals minimal cancerous tumors. The “hot spots” illuminated by the isotope are then subjected to radiography or, better yet, computed tomography (CT). PET is the “queen” of evidence; unfortunately, it is an expensive study, so it is not very suitable for monitoring the effectiveness of therapy.
Bone resorption markers are not suitable for identifying foci in the skeleton; they have not been actively used in practical oncology.
Blood tests allow one to suspect a tumor lesion in the bone marrow, which often accompanies metastasis to the sternum.
Treatment of skeletal lesions
Is it possible to cure bone metastases? Definitely, treatment can prolong life if you feel well. On the one hand, skeletal lesions are a manifestation of the spread of cancer throughout the body, on the other hand, they are a sign of a relatively favorable prognosis of the disease in the absence of tumors in other tissues and visceral (internal) organs, which gives years of life when the process stabilizes.
At the stage of bone metastasis, the question of radical treatment is no longer raised, but surgery is not excluded if the histological structure is favorable and the lesion is solitary - the only bone lesion. So, in case of lung or kidney cancer with metastasis to the humerus or thigh, a one-stage intervention can be performed with removal of the diseased organ and bone resection with prosthetics, but after several months of chemotherapy.
Chemotherapy is the main method of treating bone lesions, the drug regimen is determined by the primary tumor. For breast and prostate cancer, hormonal therapy shows good results.
Supplementing chemotherapy with local radiation can improve the overall outcome of therapy, relieve pain and reduce the likelihood of fracture. So, if the cervical vertebrae are affected, radiation therapy is mandatory already at the first stage.
The operation is necessary if there is a threat of compression (compression) of the spinal cord by a broken vertebra; as a rule, the affected part of the vertebra is removed - laminectomy. With long-term stabilization (more than six months) as a result of chemotherapy, the question of removing the affected bone of the limb and replacing it with a prosthesis can be raised, if there are no other manifestations of cancer.
Spondylitis is the cause of destruction of the vertebral bodies
With tuberculous spondylitis, damage to the vertebral bodies of the cervical and thoracic spine is noted. The pathology leads to the development of single purulent abscesses, cuts, often irreversible paralysis of the upper limbs, the formation of a pointed hump, deformation of the chest, and inflammation of the spinal cord.
With brucellosis spondylitis, damage to the lumbar vertebral bodies is noted. X-ray photographs show fine focal destruction of the vertebral bone bodies. Serological testing is used for diagnosis.
Syphilitic spondylitis is a rare pathology that affects the cervical vertebrae.
In the typhoid form of the pathology, damage occurs to two adjacent vertebral bodies and the intervertebral disc connecting them. The process of destruction in the thoracolumbar and lumbosacral sector occurs quickly, with the formation of multiple purulent foci.
Damage to the periosteum of the vertebral bodies in the thoracic region occurs with actinomycotic spondylitis. As the pathology develops, purulent foci and punctate fistulas form, the release of whitish substances, and destruction of bone tissue are noted.
As a result of spinal trauma, aseptic spondylitis can develop, in which inflammation of the spinal bodies is noted. The pathology is dangerous because it can be asymptomatic for a long time. In this case, patients may learn about the destruction of the spine with a delay, when the vertebra takes on a wedge-shaped shape and foci of necrosis appear in the spine.
What is a spinal hemangioma?
Destruction is a pathology that can affect both soft tissues and bones; patients often experience hemangiomas of the vertebral bodies.
Hemangioma is a benign tumor neoplasm. The development of hemangioma can be observed in humans regardless of age. Pathology often occurs in children due to improper development of blood vessels in the embryonic period.
Usually, no obvious disturbances are observed from the newly formed tumor, since it does not manifest itself with any symptoms, but this depends on its size and location. Discomfort, some disturbances in the functioning of internal organs, and various complications can cause the development of hemangioma in the auricle, kidneys, liver and other organs.
Despite the fact that the tumor is a benign neoplasm, children experience accelerated growth in width and depth of soft tissue without metastasis. There are hemangiomas of the mucous membrane, internal and bone tissues (vertebral hemangioma).
Hemangiomas of the vertebral bodies are extremely rare in children. They develop as a result of congenital defects in the structure of blood vessels. When an increased load falls on the affected vertebra, hemorrhage occurs, activating the work of cells that destroy bone tissue, and this is how the destruction of the vertebral bodies occurs. Thrombi (blood clots) form at the site of the lesion, and in place of the destroyed bone tissue, new vessels appear, again defective. With a new load on the damaged area of the spine, they burst again and hemorrhage occurs. All these processes, one after another, lead to the formation of hemangioma of the vertebral bodies.
Treatment of hemangioma
In children, hemangioma of the external integument is more common than of internal organs or the spine. Depending on the structure of the tumor, the pathology can be:
The tumor does not affect the further development of the child in any way; it looks like a cosmetic defect. But since tumors tend to grow quickly, doctors recommend constantly monitoring its condition; if it grows actively, immediate treatment will be required.
For these purposes it is used:
- cryodestruction;
- sclerosis;
- cauterization;
- surgical intervention.
One of the most effective methods is cryodestruction - removal of capillary superficial hemangiomas, which are most common in children. This method can be used when the tumor is actively growing. It should not be used to treat cavernous or combined hemangiomas, since traces of ugly scars may remain on the skin. Cryodestruction is a method of removing a tumor using liquid nitrogen, which destroys its structure. To completely remove the tumor, it is necessary to undergo three treatment sessions, after which the damaged skin tissue will begin to regenerate.
Destructive changes in bone tissue are a pathology that requires timely diagnosis and proper treatment. This approach to pathology will help to avoid many diseases of the skeletal system and complications in the future.
The process of destruction in the bone structure, which gradually leads to its replacement with malignant tissue, granulation, pus - this is bone destruction. The progressive pathological process is accompanied by a decrease in bone density and an increase in their fragility. Harmony in the development of bone tissue up to the age of twenty occurs normally and naturally. After this age limit, the formation of such tissues becomes slower, and the destructive process only worsens.
Bones are a solid organ in our body, their functions are to provide musculoskeletal and protective functions. They consist of hydroxyapatite, a mineral substance, about 60-70% of the bone's weight, and organic type I collagen, about 30-40%.
When this composition changes, bone density decreases. This is one of the reasons why it is more difficult for older people to recover from any injuries than for a person at a young age. Small negative external factors can easily lead to injury, because weak bones are more susceptible to impact. A number of factors can speed up this process.
Why are bisphosphonates needed?
The use of bisphosphonates for skeletal metastases has become the standard of adequate therapy.
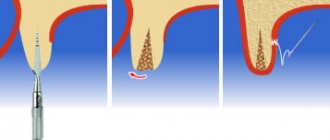
Human bones are constantly renewed: osteoclasts destroy, and osteoblasts build up tissue; normally, the processes are balanced; in the presence of a malignant tumor, osteoclasts become overactive. Bisphosphonates are similar in structure to the bone matrix, therefore, after introduction into the body, they are sent to the bones, where they have a detrimental effect on osteoclasts activated by cancer products, while simultaneously relieving pain and protecting against fractures.
Bisphosphonates can be treated for about two years; if sensitivity to them is lost, the monoclonal body denosumab plays a similar role. Demosumab and bisphosphonates are classified as osteomodifying agents (OMAs).
To prescribe OMA, it is not enough to identify “hot” lesions during osteoscintigraphy; they are used in cases of tumor lesions proven by radiological methods.
Chemotherapy and OMA are the main treatments for skeletal lesions, but they are not the only ones. Treatment of bone metastases should be comprehensive; only a combination of radiation and drugs, with the correction of metabolism and the addition of palliative surgery, can relieve pain and return the patient to an active life.
When and what is needed and possible in each specific clinical case of cancer, the specialists of our clinic know. Find out more, call:
Book a consultation 24 hours a day
+7+7+78
| More information about treatment at Euroonco: | |
| Oncologist consultation | from 5,100 rub. |
| Emergency oncology care | from 12,100 rub. |
| Chemotherapy appointment | RUB 6,900 |
| Palliative care in Moscow | from 44,300 rubles per day |
Bibliography:
- Aliev M.D., Teplyakov V.V., Kallistov V.E., Valiev A.K., Trapeznikov N.N. / Modern approaches to surgical treatment of metastases of malignant tumors in the bones // Practical Oncology, No. 1(5) (March), 2001
- Belozerova M. S., Kochetova T. Yu., Krylov V. V. Practical recommendations for radionuclide therapy for bone metastases // Malignant tumors, No. 4, 2016, Special issue 2.
- Kondratyev V.B., Martynyuk V.V., Lee L.A. / Bone metastases: complicated forms, hypercalcemia, spinal cord compression syndrome, drug treatment // Practical Oncology, No. 2 (June), 2000
- Manzyuk L.V., Bagrova S.G., Kopp M.V., Kutukova S.I., Semiglazova T.Yu./ The use of osteomodifying agents for the prevention and treatment of bone tissue pathology in malignant neoplasms // Malignant tumors: Practical recommendations RUSSCO #3s2, 2022 (vol. 7)
- Snegova A. V., Bagrova S. G., Bolotina L. V., Vladimirova L. Yu., Gorbunova V. A., Kogonia L. M./ Prevention and treatment of bone tissue pathology with osteomodifying agents (OMA) in malignant neoplasms // Malignant tumors, No. 4, 2016, Special issue 2.