Dear friends, today’s topic of conversation, in fact, should be a prologue to all our publications devoted to bone tissue augmentation before implantation. We have already written about sinus lifting, guided bone regeneration, bone blocks and osteotomy, we talked about when and why this should be done, but we left out of the scope of publications perhaps the most interesting question:
Why does bone atrophy occur in the first place?
What is atrophy? What are its reasons? Why does it develop rapidly in some people, literally in a month or two:
and someone walks without teeth for years - and there is no loss of bone tissue?
Is it possible to predict the degree of bone tissue atrophy even before tooth extraction and is there a way to prevent it?
The answers to these questions are important, if only because without understanding the biological mechanisms of atrophy, it is impossible to determine the need for the same preventive augmentation of the socket of an extracted tooth, it is impossible to CORRECTLY choose the method of bone tissue augmentation for a specific clinical case and, most importantly, it is impossible to give a clear and long-term prognosis as a result of osteoplasty.
I will say even more - in many ways, almost all unsuccessful outcomes of bone tissue augmentation are explained, among other things, by a lack of understanding of the processes occurring in the jawbone after tooth extraction. That's why this knowledge is important.
So,
Atrophy is...
According to medical textbooks, atrophy means a lifetime decrease in the volume of cells, tissues and organs , accompanied by a decrease or cessation of their functions. In relation to dentistry and implantology, we can define atrophy as a change in the linear dimensions and volume of the alveolar ridge after the removal of a tooth or teeth.
Atrophy can be reversible or irreversible.
Reversible atrophy is usually caused by the cessation of functioning of an organ or tissue. So, if you do not use your hand for a long time (for example, after a fracture), the muscles of the hand will atrophy.
However, once the function returns, they quickly return to normal.
Irreversible atrophy has a number of causes, of which dysfunction is just one of them. Thus, atrophy of the heart muscle is accompanied by its sclerosis, the replacement of the muscle fibers themselves with connective tissue. The result is chronic heart failure, for which only symptomatic treatment exists so far.
The reversibility of brain atrophy in some people remains controversial.
, atrophy of the alveolar ridge after tooth extraction is classified as dysfunctional, i.e., associated with cessation of function. It would seem a very simple mechanism - “no teeth, no load on bone tissue - presto, atrophy!”
But, in reality, not everything is so simple.
First, dysfunctional atrophy is usually reversible (see muscle example).
Secondly, and this is the question that concerns me first, why do different people have different rates and levels of bone loss?
Why do some patients develop atrophic pesdets within a few weeks after tooth extraction, while others live without teeth for many years, maintaining almost the original volume of bone tissue? Where does this injustice come from?
And so, in order to understand this issue, we need to remember what bone tissue is in general.
Treatment
Treatment of tooth decay is a complex task that requires a professional approach. To date, a number of techniques have been developed that can effectively restore the appearance of teeth and their functionality, as well as stop destructive processes. And timely contact with the dentist plays an important role in this! It is important to remember: missing teeth is not the norm! Even if for some reason one or two of them were lost, it is important to compensate for their absence by installing implants or artificial crowns.
Make an appointment through the application or by calling +7 +7 We work every day:
- Monday—Friday: 8.00—20.00
- Saturday: 8.00–18.00
- Sunday is a day off
The nearest metro and MCC stations to the clinic:
- Highway of Enthusiasts or Perovo
- Partisan
- Enthusiast Highway
Driving directions
Bone tissue is...
We partially touched on this topic when discussing the “Theory of Osteoplasty”. Now let's talk about this in more detail.
The first thing you need to know about bone tissue:
Yes, metabolic processes in it are extremely slow, and after death, unlike soft tissues, it practically does not change its volume and basic properties - and this is the reason why many people, including implant dentists, perceive it is too mechanical, like ordinary inanimate material for sawing and drilling. This attitude leads to a “carpentry approach” to implantation, which can be formulated in one phrase: “the tighter you screw it in, the better it holds.” However, I also wrote about this. You can read about torques and why forces >30 Ncm are bad here>>.
Second, no less important, is that the current state of bone tissue is the result of a biological balance between the processes of osteolysis and osteogenesis. In other words, bone cells divide and die, collagen fibers degrade and form again, calcium moves into and out of bone tissue - and all this happens constantly and continuously.
The third thing you should know about bone tissue is that its main component, both in volume and mass, the intercellular substance (osteomatrix), participates in regeneration exclusively indirectly. Therefore, it is completely useless to drink calcium to “build bone tissue” - and we have already written about this. As well as the fact that the source of “bone formation” is only living cells of bone tissue, osteoblasts and osteocytes. There is a fundamental difference between these cells:
That is, only osteoblasts move and multiply. An osteocyte is a cell that is not capable of division, the main task of which is to produce osteomatrix, forming around itself a structural unit of bone tissue, an osteon (the picture is honestly copied from some textbook):
Consequently, the “denser” the bone tissue, the harder and stronger it is, the fewer osteoblasts, dividing cells, and the more osteocytes, non-dividing cells, it contains. And the “denser” and “harder” the bone tissue is, the worse it will regenerate, that is, recover from damage.
Fourth , the bone tissue is uneven in structure. It has a dense cortex called the “lamina compacta” and a loose interior called “cancellous bone.”
And, depending on the ratio of compact lamina and cancellous bone, alveolar bone is usually divided into biotypes. We talked about them many, many times, for example here>>, here>> and here>>:
So, friends, based on what we know about osteogenesis and bone tissue cells, the regeneration of bone tissue of different biotypes will differ. Knowing this, we can adequately choose the method of bone tissue augmentation – and always achieve a good treatment result.
And finally, the fifth thing you need to know about jaw bone tissue.
Its decline is a direct consequence of disturbances in biological balance, metabolism, osteogenesis and osteolysis, etc.
How does the violation occur?
Again, I wrote about this. I recommend reading it>>.
The body perceives any surgical operation, including tooth extraction, as an injury and reacts to it with an appropriate reaction, inflammation.
Inflammation is a complex pathophysiological process consisting of several smoothly flowing stages:
During inflammation, a number of biologically active substances (BAS) are released, triggering phagocytosis, in which osteoclasts and other macrophages participate. They destroy everything that they consider damaged (and everything damaged is marked in advance with special compounds, antibodies).
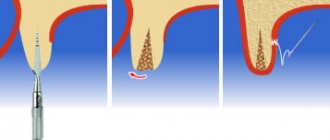
Thus, the process of osteolysis - osteoclasts eat bone tissue, it decreases in volume. And everything would be very sad if osteoclasts did not die from their gluttony - when they die, they secrete a whole series of mediators, the so-called. Bone Morphogenetic Proteins (BMP) or, in foreign languages, BMP (Bone Morphogenetic Proteins), which activate the reproduction and differentiation of fibroblasts and osteoblasts. In other words, they trigger osteogenesis, the growth of new bone:
And here we need to make a couple of important notes:
– the main biologically active substances that trigger phagocytosis (cytokine proteins, etc.) are released during the alterative stage of inflammation, which is known for its violent symptoms. Yes, friends, swelling, pain, increased temperature of the injured area - all this happens in the alteration phase.
– yes, we are all afraid of pronounced post-operative (read, “inflammatory”) symptoms and do a lot to ensure that they are as mild as possible. But an interesting fact is that a weakly expressed alteration stage will not provide the required amount of biologically active substances to trigger osteoclasts, and they, in turn, to regenerate bone tissue. Thus, there is a direct positive relationship between the symptoms of the postoperative inflammatory process and subsequent regeneration: the more pronounced the alterative stage of inflammation, the more factors that control osteogenesis are released.
In fact, the post-traumatic inflammatory process throws our osteolysis-osteogenesis equation out of balance - due to the increased activity of bone-eating cells, osteolysis outweighs:
Fortunately, this process does not last long. Gradually, all processes are balanced again, the rate and degree of osteolysis is almost equal to the degree and rate of osteogenesis.
And the process of atrophy slows down. If we tie it to time and draw a graph, we get the following:
Simply put, the greatest amount of bone loss occurs in the first 4-8 weeks after tooth extraction. Then, the process slows down - and, taking a period of time from 18 to 24 months after removal, we are surprised to note that the linear dimensions of the bone practically do not change:
But let’s return to bone tissue biotypes.
If there is a relationship between the biotype of the alveolar bone and its regenerative capabilities (osteogenesis), then, obviously, there is a relationship between the biotype and the rate of bone atrophy. And you have observed this many times - let’s say, if we see a very strongly atrophied alveolar ridge, then, as a rule, it is of the D1-D2 biotype, and if the shape and volume of the jaw bone after the loss of teeth practically does not decrease over a long period of time, then by 146% D3-D4.
And this is easy to explain, knowing that the bone tissue of the D3-D4 biotype is better supplied with blood, there are more osteoblasts in it, and metabolic processes in it are more intense. Significant atrophy of such an alveolar ridge that requires osteoplasty occurs rarely and, as a rule, only in cases of very, very, very traumatic tooth extraction, or against the background of a chronic inflammatory process, when osteoclasts and other macrophages are active for a very, very, very long period of time .
Symptoms of periodontitis
Let's start with the fact that in the initial stages the disease occurs without symptoms, and it can only be detected at a dentist's appointment; this will require an x-ray. Symptoms appear in the stage of acute periodontitis or as a result of exacerbation of the chronic form. Among the signs of the disease:
- sharp or aching pain;
- swelling of the gums in the affected area;
- feeling as if the tooth has become taller;
- temperature increase;
- sleep disturbance;
- tooth mobility;
- tissue redness;
- pain when touching a tooth or chewing food.
If at least two symptoms occur, contact your dentist.
What in practice?
Knowledge of the principles and patterns of the atrophic process, on the one hand, breaks the pattern and our understanding of osteoplasty, but on the other hand, it provides a very reliable prognostic tool. Using it, you can not only predict the dynamics of changes in bone tissue volumes after removal and implantation, but also clearly explain how different methods of bone tissue augmentation work in different clinical conditions.
What do we know about the patient?
The biotype of bone tissue is something that we can determine from a computed tomogram even before tooth extraction.
How to use it?
Knowing the relationship between the biotype and atrophy, it is possible to more or less reliably determine the indications, for example, for preventive preservation of the socket, including immediate implantation.
And, in theory, such a clear analysis and prognosis of atrophy in relation to a specific clinical case should replace the well-established principle in modern implantology “Everyone does it!” or “That’s how we were taught!”
In addition, we can predict the degree of atrophy and determine whether bone augmentation will be required during delayed implantation even before the teeth are extracted.
and, if necessary, what is the best method to do this?
Or, for example, can we explain why in some cases the transplanted bone block goes away, but in others it does not?
Sinus lift for recovery
The sinus lift procedure is designed to increase bone tissue by elevating the maxillary sinuses. It is used provided that the patient has no pathologies or allergic reactions.
If the patient has a history of chronic runny nose, sinusitis, or multiple septations, the operation will not be performed.
The procedure allows you to increase the missing volume of bone tissue, but there remains a risk of developing a chronic runny nose or inflammatory process in the future.