Herpangina is one of the most common viral diseases in children. Almost everyone experiences this disease in childhood, although this diagnosis also occurs in adults. From a scientific point of view, the very name “herpetic sore throat” was incorrectly given to the disease. Previously, the disease was little studied. Scientists, noticing the similarity of rashes during the disease with those of herpes, came to the conclusion that the causative agent of the disease was the herpes virus, and gave the disease a name that has stuck and is found in the medical literature in exactly this form. Although the disease has nothing in common with herpes infection. It has been established that the cause of herpetic sore throat is enteroviruses - Coxsackie viruses of groups A and B and ECHO viruses (echoviruses). In medical reference books you can find different versions of the names of this disease: aphthous tonsillitis, vesicular pharyngitis, herpetic tonsillitis, herpangina, etc.
As already mentioned, children under ten years of age are at risk: infants, preschoolers and children of primary school age. The severity of the disease depends on the age of the child. The disease is most severe in children in the first year of life. Preschoolers are more often infected because at this age they do not pay due attention to hygiene, have contact with animals and are often in children's groups. To become infected, it is enough to eat unwashed fruit. This should also include the immaturity of immunity at an early age. The disease is highly contagious, and often its outbreaks become epidemic. It is noteworthy that this disease does not occur in babies in the first months of life - the antibodies found in mother's milk create some kind of immunity to herpangina.
One can trace the obvious seasonality of herpetic sore throat: the peak occurs in summer and autumn. As a rule, having been ill once, a child becomes immune to re-infection, so this disease is less common among adolescents and adults.
Infection can occur in one of three ways:
- airborne
- contact
- fecal-oral.
With the airborne method, infection occurs by sneezing, coughing, or talking with a carrier of the virus. In case of contact - through discharge from the nasopharynx. With the fecal-oral method - through dirty hands, through unwashed food, toys and pacifiers, which is especially typical for children.
Even a recovering person can still spread the infection around him for about a month, so it is believed that herpes sore throat is highly contagious: a child can easily become infected in kindergarten from a baby who does not even have obvious symptoms of the disease. If one family member gets sick, most likely everyone will suffer from the disease.
How does infection spread throughout the body? First, the virus from the nasopharynx reaches the intestinal lymph nodes through the lymph flow. Already in the intestines, the virus gains strength and enters the blood, and severe inflammation begins in the oropharynx.
Causes
Herpetic stomatitis, or as it is also called aphthous stomatitis, is dangerous, first of all, for young children. It is a serious viral disease, which, in addition to damaging the oral mucosa, causes general intoxication of the body and provokes malfunctions of the nervous, immune, and reticuloendothelial systems.
Herpes, which is the causative agent of the disease, may not make itself felt for a long time, although infection usually occurs in early childhood.
When the baby’s immunity is weakened, the herpes virus is activated and begins to multiply, causing an increase in temperature, enlargement of the submandibular lymph nodes, acute inflammation of the mucous membrane, and the formation of bleeding and painful ulcers on its surface.
Main reasons:
- decreased baby's immunity;
- previous infectious diseases;
- lack of vitamins;
- insufficient oral hygiene;
- direct contact with patients with herpes stomatitis.
Infants are more likely to become infected with the herpes virus during childbirth, provided the mother has a herpes infection. In children under one year old and school-age children, the virus is activated against the background of an organism weakened by disease and vitamin deficiency.
Cytomegalovirus infection
An infectious disease that is caused by cytomegalovirus (CMV) and is characterized by a variety of clinical forms (from asymptomatic to severe generalized with damage to many organs) and course (acute or chronic). CMV transmission factors can be almost all biological substrates and human secretions that contain the virus: blood, saliva, urine, cerebrospinal fluid, vaginal secretions, sperm, amniotic fluid, breast milk. Potential sources of infection are organs and tissues in transplantology, as well as blood and its products in transfusiology. Routes of transmission of CMV infection: airborne, sexual, vertical and parenteral.
There are congenital and acquired forms of CMV infection. Congenital CMV infection. During antenatal infection of the fetus, infection occurs predominantly transplacentally. During intrapartum infection, CMV enters the body through aspiration of infected amniotic fluid or secretions from the mother's birth canal.
In older children, acquired CMV infection occurs in a subclinical form in 99% of cases. The most common manifestation of this form of CMV infection in children over one year of age is mononucleosis-like syndrome. As a rule, a clinical picture of acute respiratory disease is observed in the form of pharyngitis, laryngitis, and bronchitis.
Infections caused by the sixth, seventh and eighth types of herpes viruses Type six herpes viruses (HHV-6) can cause erythematous and roseolous rashes (sudden exanthema), lesions of the central nervous system and bone marrow in immunocompromised children. Herpesvirus type seven (HHV-7) causes neonatal exanthema
For the diagnosis of herpes infection, cytological, immunofluorescent, serological and PCR methods are valuable. Virological testing for herpes infection reveals complement-fixing antibodies to HSV-1 or -2 in the mother's blood, fetal cord blood and amniotic fluid. PCR method. The material for testing for herpes is blood, throat swabs, the contents of blisters, ulcers, and urine.
The study of specific antibodies of various subclasses: IgM, IgG1-2, IgG3 and IgG4 to herpes viruses is important. The detection in the blood serum of children of specific immunoglobulins M, IgG3, IgG1-2 in a titer > 1:20, viral antigen and specific immune complexes with antigen indicates the severity of the infectious process (active phase), and the determination of only specific IgG4 is regarded as the latent phase of infection or carriage of maternal antibodies.
Main symptoms and signs of the disease
Acute herpetic stomatitis in children develops gradually and is preceded by an incubation period lasting from two days to 3 weeks.
Early symptoms of the disease are:
- burning in the mouth;
- increased salivation;
- headache, nausea, general weakness;
- increased body temperature;
- enlargement of the submandibular lymph nodes;
- the appearance of bad breath.
«
If the parents do not respond to the first signs, after a few days the mucous membrane becomes covered with multiple rashes. Small painful blisters itch, respond with acute pain to the touch, and when they rupture, a cloudy liquid flows out of them. The rash appears on the baby’s gums, cheeks, tongue, lips, and wings of the nose.
Herpes stomatitis can affect not only a school-age child, but also an infant.
The mild form of the disease can be easily treated at home; in moderate and severe forms, hospitalization of the small patient is indicated.
Acute herpetic stomatitis
Acute herpetic stomatitis is a highly contagious disease of the oral mucosa and gums. It can be considered an independent disease, since the cause is primary infection with the herpes virus. This disease mainly affects children under three to five years of age, who have reduced local (oral mucosa) and general immunity. In older children, the disease appears less frequently (primary infection occurs without symptoms of acute herpetic stomatitis), but even mature people are at risk of this disease in some cases. The incubation period, i.e. the time from infection to the first symptoms ranges from 2-26 days.
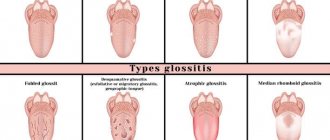
Symptoms of acute herpetic stomatitis . The disease begins with a feeling of general malaise. Obvious symptoms of herpes stomatitis appear after a latent period, most often after 10-14 days. Redness of the mucous membrane is observed, small bubbles appear on the tip of the tongue, oral mucosa, gums (at the everyday level they are referred to as herpes on the gums ), and palate. The blisters quickly burst and the formation of lesions is possible - erosions, afts (stage or phase of aphthous stomatitis), ulcers. Additional and concomitant symptoms of herpes stomatitis (acute): pain (even severe) in the oral cavity, increased salivation, bad breath, swelling of the cervical lymph nodes, low-grade fever, headache. In practice, depending on the degree of damage to the mucous membrane and the general condition of the body, there are mild, moderate and severe forms (in childhood, sometimes requiring hospitalization) of acute herpetic stomatitis. Accurate diagnosis is carried out using laboratory tests.
Complications of the disease . In the absence of timely treatment of this disease, dangerous consequences and complications are possible. The disease can unnoticeably progress to chronic recurrent herpetic stomatitis . A herpes infection can spread to the eyes and cause worsening or even loss of vision. The spread of infection to the brain can cause inflammation (encephalitis) with all the ensuing consequences.
Classification and diagnosis
Herpetic stomatitis is classified both according to the severity of the disease and the characteristics of its course.
According to the characteristics of the course, acute and chronic (recurrent) forms are distinguished. Acute stomatitis is characterized by a sudden onset, pronounced symptoms, and rapid development. Without proper treatment, it quickly becomes chronic and can drag on for years, periodically exacerbating.
Based on the degree of severity, there are mild, moderate, and severe forms.
In mild forms, the following are noted:
- slight increase in body temperature;
- redness, swelling, inflammation of the gums;
- swollen lymph nodes;
- a small number of painful ulcers.
The average degree is characterized by:
- significant increase in body temperature;
- general weakness, nausea, headache;
- inflammation of the oral mucosa;
- the appearance of a blistering rash on the inner surface of the cheeks, gums, tongue, and around the mouth.
The severe form causes:
- temperature rise to a critical level;
- lymphadenitis of the cervical, submandibular lymph nodes;
- a sharp disturbance in general well-being;
- the appearance of severe muscle pain, headache;
- nausea, vomiting;
- multiple rashes that spread to the eyelids, conjunctiva, and perioral area.
Diagnosing the disease is not difficult for an experienced doctor. It is based on an analysis of the main symptoms, the order of clinical manifestations of the disease, the nature, and multiplicity of ulcers.
It is necessary to differentiate herpetic stomatitis from viral stomatitis; for this, in the first few days of the disease, a cytological examination of scrapings from erosions and aphthae should be done.
How long does the disease last and how many days is the child contagious?
Depending on the complexity of the form, herpes stomatitis in children lasts from several days to 2-3 weeks. With a mild form, the main symptoms disappear on the third or fourth day, treatment of a moderate form takes one to two weeks. The severe form is the most dangerous; healing lasts for weeks and requires mandatory hospitalization of the baby.
The disease is characterized by a high degree of contagiousness precisely during the period of exacerbation.
The infection is transmitted by airborne droplets (including through kissing), when using shared dishes, cutlery, toys, and hygiene items.
Herpes is contagious and can easily be transferred to healthy parts of your own body.
It is necessary to wash your hands thoroughly after treating the surface affected by the sores with medications to prevent the spread of the virus.
Herpes simplex virus types 1 and 2
The term “herpes infection” (HI) is usually used to refer to diseases that are caused by HSV-1 and HSV-2. The source of HSV infection are sick people with various forms of the disease, including latent ones, as well as virus carriers.
HSV-1 is transmitted by airborne droplets and contact. When the virus gets on the skin during a cough or sneeze, it is contained in droplets of saliva and survives for an hour. On wet surfaces (washbasin, bathtub, etc.) it remains viable for 3-4 hours, which is often the cause of disease outbreaks in preschool institutions. Infection can occur through kissing, as well as through household items that are infected with the saliva of a patient or virus carrier. HSV-2 is transmitted sexually or vertically. With the latter, infection occurs during childbirth (contact with the mother's birth canal), transplacentally or through the cervical canal in the uterine cavity. Due to the fact that viremia occurs during generalization of infection, transfusion or parenteral transmission of HSV-2 infection is also possible. HSV-2 usually causes genital and neonatal herpes.
Children are most susceptible to GI between 5 months and 3 years of age. Depending on the mechanism of infection, acquired and congenital forms of HI are distinguished. Acquired HI can be primary and secondary (recurrent), localized and generalized. A latent form of GI is also isolated.
No infection has such a variety of clinical manifestations as the herpes virus. It can cause damage to the eyes, nervous system, internal organs, mucous membrane of the gastrointestinal tract, oral cavity, genitals, can cause cancer, and has a certain significance in neonatal pathology and the occurrence of hypertension. The spread of the virus in the body occurs through hematogenous, lymphogenous, and neurogenic routes.
The frequency of primary herpesvirus infection increases in children after 6 months of life, when antibodies received from the mother disappear. The peak incidence occurs at the age of 2-3 years. HI often occurs in newborns; according to a number of authors, it is diagnosed in 8% of newborns with general somatic pathology and in 11% of premature infants.
According to WHO, diseases caused by the herpes simplex virus (HSV) are the second leading cause of death from viral infections after influenza. Solving the problem of diagnosing and treating herpesvirus infection with manifestations on the oral mucosa is one of the most important tasks of practical medicine.
In the last decade, the importance of herpesvirus diseases as a public health problem has been constantly growing throughout the world. Members of the human herpesvirus family infect up to 95% of the world's population.
Primary forms of GI include: infection of newborns (generalized herpes, encephalitis, herpes of the skin and mucous membranes), encephalitis, gingivostomatitis, Kaposi's eczema herpetiformis, primary herpes of the skin, eye, herpetic panaritium, keratitis. Primary HI occurs due to initial human contact with HSV. As a rule, this occurs in early childhood (up to 5 years). In adults aged 16-25 years who do not have antiviral immunity, primary HI may more often be caused by HSV-2. 80-90% of initially infected children carry the disease latently, and only in 10-20% of cases are clinical manifestations of the disease observed.
Secondary, recurrent forms of GI are herpes of the skin and mucous membranes, ophthalmic herpes, and genital herpes.
How and with what to treat herpetic stomatitis in children
As Dr. Komarovsky notes, treatment of herpetic stomatitis in children, regardless of age, depends on the severity of the disease, the general condition of the patient’s immune system, and the presence or absence of concomitant diseases.
The main question that interests young parents is which doctor should they contact if they suspect herpetic stomatitis. Both a qualified pediatrician and a dentist can advise the child.
Therapeutic methods include both general and local treatment. Common activities include:
- prescription of antiviral drugs (acyclovir, Zovirax, Herpevir, Virolex);
- taking antipyretic and painkillers (paracetamol, Panadol, Eferalgan, Tylenol);
- prescription of antihistamines (diazolin, claritin, erius, fenistil);
- correction of the immune system (immudon, sodium nucleinate);
- vitamin therapy (vitamin C, ascorutin, multivitamins, B vitamins).
Children of older preschool and school age are recommended to be treated with broad-spectrum antibiotics to avoid possible complications.
For newborns and infants, antibiotic therapy is prescribed only as a last resort, with preference given to local therapy:
- applications of painkillers (solution of lidocaine, trimecaine, pyromecaine);
- treating the baby’s oral cavity with antiseptics (solutions of furatsilin, potassium permanganate, brilliant green, blue);
- Treatment of aphthae with iodine should be avoided, as it causes a burn to the mucous membrane;
- the use of antiviral medications in the form of ointments, lotions, solutions (interferon, acyclovir);
- applying an oil solution of vitamin A, sea buckthorn or rosehip oil, solcoseryl to the mucous membrane of the baby’s mouth).
If the symptoms of the disease do not disappear on the 3-4th day of treatment, but only intensify, the child is indicated for treatment in a hospital setting, otherwise stomatitis will become chronic, from which it is impossible to get rid of it.
Treatment of herpes in children
It is impossible to eliminate the herpes virus from the body, so the goal of treatment is to reduce its activity , eliminate symptoms by activating the immune system, achieve stable remission and prevent complications.
The most effective medicine against most manifestations of the herpes virus in children is the substance acyclovir. Treatment uses both oral and local medications. Source: I.F. Barinsky, L.M. Alimbarova, A.A. Lazarenko, F.R. Makhmudov, O.V. Sergeev Vaccines as a means of specific immunocorrection for herpetic infections // Questions of Virology, 2014, pp. 5-11
A comprehensive treatment regimen for acute herpetic infection includes:
- antiviral-antiherpetic drugs - tablets, injections and ointments - based on acyclovir;
- surface antiseptics for the prevention of secondary bacterial infections;
- immune stimulants – herbal and interferon derivatives;
- multivitamins and vitamins in therapeutic doses;
- antipruritic antihistamines;
- antipyretics;
- hepatoprotectors – in case of severe intoxication;
- diet therapy with sufficient amounts of protein and exclusion of foods that are sources of arginine.
In severe general condition, bed rest is recommended. Only a doctor can decide how to treat herpes in a child.
Treatment with folk remedies at home
When treating herpes stomatitis in children, it is extremely important to prevent the development of complications and transition to a chronic form. Therefore, all folk remedies are auxiliary in nature and should not replace full treatment.
To strengthen the child's immunity, a decoction of echinacea leaves, ginseng root, and rose hips is well suited.
Rinsing will help relieve itching, burning and pain. For these purposes, you can use decoctions of chamomile flowers, sage, calendula inflorescences, St. John's wort, alder cones, rose petals, and oak bark.
The healing of ulcers and aphthae is facilitated by treating their surface with brilliant green, blue and iodine; they have a drying effect. An alcohol solution of propolis helps well, it relieves the inflammatory process and has an analgesic effect on the oral mucosa. Use with caution to treat small children.
Newborns and infants are recommended to lubricate the inflamed oral mucosa with natural honey. This should be done with extreme caution, since honey is a fairly strong allergen.
Possible complications
Primary infection with herpetic stomatitis is highly treatable. Within 7-10 days, with proper treatment, the child can fully recover. Without appropriate drug therapy, the following complications may develop:
- herpetic keratoconjunctivitis (a dangerous herpetic eye infection that leads to blindness);
- dehydration (due to refusal to eat and drink).
To avoid undesirable consequences, it is necessary to consult a doctor at the first symptoms of the disease, strictly adhere to all instructions, give the baby plenty of fluids, monitor oral hygiene, and wash your hands after each treatment of a surface affected by herpes.
Prevention in children
Preventing infection with the herpes virus is extremely difficult, since 90% of the population are carriers of it. It is important to delay infection as much as possible; the younger the child, the more difficult the disease is to tolerate. It is necessary to avoid contact with people who have an acute herpes virus. From infancy, the baby should be taught to use personal hygiene products, not allowed to drink from someone else’s mug after someone else, or to use used spoons, forks, and plates. You should not kiss someone who has a herpetic sore on their lips.
To prevent herpetic stomatitis, you need to do general strengthening of the child’s immune system, systematically give him B vitamins, multivitamin complexes, and carry out hardening procedures.
Types of disease in children
There are 80 types of herpes virus, of which 8 are dangerous to humans. The nature of the disease and the type of herpetic rash depend on the type of herpes simplex virus (HSV):
- Type 1 HSV - looks like cold-like rashes in the form of blisters on the lips, causes herpetic stomatitis and herpetic encephalitis.
- Type 2 HSV – manifests itself as a rash on the genitals (genital herpes).
- Type 3 HSV – causes chickenpox and recurrent herpes zoster.
- The 4th type of HSV - Epshane-Barr virus, causes malignant lymphoma and infectious mononucleosis - an acute viral disease with fever, damage to the respiratory tract, lymph nodes, liver, spleen and blood.
- Type 5 HSV – cytomegalovirus; affects the respiratory system, internal organs, intestines, eyes, brain, nervous and urinary systems.
- Type 6 HSV - causes viral eczema - exanthema - pseudorubella-type rash;
- The 7th and 8th types of HSV have not been sufficiently studied. Source: A.G. Lateral Herpesvirus infections in children - an urgent problem of modern clinical practice // Children's infections, 2010, No. 2, pp. 3-7