Oral lichen planus, or stomatodermatosis , is a chronic disease of the oral cavity. It is characterized by abundant formation of papillomas, plaques and erosions in the oral cavity, accompanied by inflammatory and degenerative damage to the oral mucosa. This is one of the most common pathologies of the oral cavity, affecting the back of the cheeks, gums, lips, tongue and surface of the hard palate. The likelihood of this disease occurring largely depends on the individual predisposition of the patient. The disease is not transmitted by contact.
Causes of the disease
Lichen planus occurs under the influence of a number of factors, among which the most common is immuno-allergic. When the body's immunity decreases under the influence of external and internal factors, T-lymphocytes cannot cope with their protective function.
Factors that provoke the development of oral lichen planus include:
- Chronic stress;
- Strong shocks;
- Diseases of the gastrointestinal tract;
- Diabetes;
- Hypertension;
- Grynszpan syndrome;
- Injuries to the oral mucosa;
- Incorrectly installed dentures;
- Fillings that injure the oral mucosa;
- Prostheses made of dissimilar materials;
- Long-term use of tetracycline;
The risk group also includes patients whose work involves developing camera film or who come into contact with paraphenyldiamine.
How dangerous is lichen planus?
Lack of treatment or a severe stage of the disease can lead to damage to the entire skin, severe discomfort and a significant decrease in immunity.
Lichen planus on the scalp can cause irreversible hair loss, and on the nail plates - nail deformation (thinning, splitting, rejection of the nail plate, even nail lysis).
A pathological lesion in the eye area can lead to blurred vision or narrowing of the tear duct.
The erosive form of the disease often leads to the formation of scars, and the result of lesions of the genital mucosa can be narrowing of the vagina or phimosis.
Also, some forms of the disease are prone to malignancy and degeneration into squamous cell skin cancer.
Symptoms of the disease
There are six types of oral lichen planus. This is a typical, exudative-hyperemic, hyperkeratotic, erosive-ulcerative, bullous and atypical form. They are united by the formation of foci of inflammation on the oral mucosa, the appearance of defects and erosions. In some particularly severe forms of the disease, the patient may complain of itching and burning sensation in the mouth and difficulty eating. In milder forms, the disease may not manifest itself at all.
Typical lichen planus is the most common form, occurring in half of patients. White nodules appear on the mucous membrane of the oral cavity. Merging, they resemble lace.
The esscudative-hyperemic form is characterized by the appearance of gray papillomas on the edematous mucous membrane.
The hyperkeratotic form is one of the least common forms, which is characterized by the formation of gray spots that rise above the affected surface. Over time, these plaque spots become rougher and flake off.
Erosive-ulcerative is the most severe form of the disease, occurring in 23% of cases. Multiple erosions and ulcers covered with fibrinous plaque appear on the lining of the oral cavity. There is a strong burning sensation in the mouth, and when trying to remove plaque, bleeding and pain occur.
The bullous form is a relatively rare variety, occurring in 3% of cases. Accompanied by the appearance of dense blisters, inside of which there is hemorrhagic exudate. After the bubbles open, erosions form.
Atypical form - occurs slightly more often than bullous - in 4% of cases. This form is characterized by dilation of the mouth of the salivary gland, as well as inflammation of the lips and gums.
Quite often, one patient can develop several forms of lichen planus in parallel. Often one form can flow into another. Ringworm is a chronic disease prone to relapse.
Lichen planus of the oral mucosa, modern methods of local treatment
Lichen planus (LP) is a nodular chronic disease that occurs on the skin and visible mucous membranes. With this disease, the mucous membrane of the oral cavity and the red border of the lips are often affected. The disease is more common in women aged 40 to 65 years [1, 3]. The causes of lichen planus have not been fully elucidated. There are neurogenic, viral, bacterial, and autoimmune theories of this disease. Recently about those suffering from this disease. This is explained by increased contact with viral infection, a significant change in the body’s reactivity, as well as an increased frequency of psycho-emotional stress [4]. The main place in the frequency of lichen planus lesions is the skin. Papules on the skin are up to 2 mm in diameter, purple in color, with hyperkeratosis, dense consistency, with polygonal contours and an indentation in the center [3, 5].
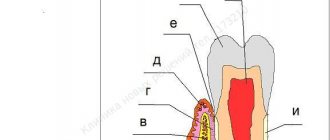
According to a number of authors, the frequency of lesions of the oral mucosa varies from 60 to 80% [2, 4]. A unique clinical picture is presented by lichen planus on the red border of the lips (Fig. 1-a) and tongue (Fig. 1-b).
Rice. 1. Lichen planus. Erosive-ulcerative form with damage to the lips (a) and tongue (b). Pronounced mesh pattern of whitish-bluish color on the lips and lateral surfaces of the tongue
In most patients, individual small papules with a polygonal base are identified. The papules are connected to each other by keratotic bridges. Keratification gives the papules a whitish-bluish tint [4].
Today, there are six main clinical forms of lichen planus of the oral mucosa (LI) and the red border of the lips: typical, hyperkeratotic, exudative-hyperemic, erosive-ulcerative, bullous, atypical. According to some data, the pigmented form is extremely rare [1, 2].
Signs of lichen planus are milky-white rough areas of keratinization and the appearance of fine meshwork, the so-called Wickham mesh (Fig. 2 - a, b).
In the exudative-hyperemic form with an increase in the inflammatory reaction, patients complain of pain, aggravated by eating, a burning sensation, and dryness. The mucous membrane is hyperemic and edematous. Against this background, patterns of fused papules forming “fern leaves” are clearly visible. More often, this form is observed on the mucous membrane of the cheeks and gums [5, 9].
The erosive-ulcerative form was characterized by a more pronounced inflammatory-destructive process in the epithelium of the oral mucosa. Against the background of edematous and hyperemic mucous membranes, polygonal erosions stand out, surrounded by a pattern of fused papules. The erosions are covered with a fibrinous coating and bleed easily when touched. This form is more common on the buccal mucosa, retromolar region, and lateral surfaces of the tongue [1, 2, 3, 4]. Combinations of this form with desquamative gingivitis are often observed. The general condition of patients is characterized by low-grade fever and weakness, complaints of pain, aggravated by eating, dryness and burning in the mouth.
The bullous form is most often localized on the cheeks and dorsal surface of the tongue in the form of blisters of various sizes, having a dense covering surrounded by papules. When they open, the blisters form large erosive surfaces; differential diagnosis with pemphigus vulgaris is necessary [3, 8, 9, 10]. Patients complain of the inability to eat any food due to severe pain. The general condition of patients is dominated by weakness and weight loss.
Rice. 2. Clinical manifestations of lichen planus on the oral mucosa - the inner surface of the cheeks (a) the corners of the mouth and tongue (b)
The increase in the incidence of this pathology at dentists' appointments has led to the need to improve local treatment of lichen planus. Currently, patients with lichen planus are treated with corticosteroids, which are used as injections once every 1-3 days, 1-1.5 ml of the drug for each erosion, for a course of 8-12 injections. The disadvantage of this method is the possibility of formation of atrophic scars at injection sites [2, 5].
Methods and means of treating lichen planus localized on the oral mucosa by dermatovenerologists have not changed over the past years. Today, local therapy in the oral cavity is reduced to the administration of corticosteroid ointments in the form of applications; however, the ointments, oils, creams and pastes used do not simultaneously have an adhesive, anti-inflammatory and angioprotective effect. Such treatment does not prevent the development of relapses of the disease [1, 3, 6, 7].
In connection with all of the above, to increase the effectiveness of treatment of manifestations of lichen planus on the oral mucosa, it is advisable to use agents that have an adhesive, anti-inflammatory and angioprotective effect.
Purpose of the study: to increase the effectiveness of complex therapy of lichen planus by using the developed multicomponent adhesive ointment in combination with Imudon.
Materials and research methods
A total of 56 patients were observed, aged from 32 to 75 years, among whom there were 26 men and 30 women. The subjects were divided into 3 groups, depending on the local treatment performed. General treatment in all groups consisted of taking Persen 1 capsule 3 times a day, prednisolone 25 mg every other day. The first group consisted of 16 patients who received traditional local treatment: applications of sea buckthorn oil, 5% solution of anesthesin in peach oil for 20 minutes 3-4 times a day.
The second group included 20 patients, in which local therapy was carried out using the developed ointment (RF patent for invention No. 2355411, application No. 2008108770 dated 03/11/2008). The ointment contains hydrocortisone, Solcoseryl dental adhesive paste, 5% solution of vitamin C, vitamins A and E.
In the third group, 20 patients were treated with the developed ointment in combination with Imudon.
Characteristics of the components of the developed multicomponent adhesive ointment (PAM).
Vitamins “C”, “A” and “E” have an antioxidant effect and help strengthen the walls of the microvascular bed of the oral mucosa. Solcoseryl dental adhesive paste (Reg. No. 015194/01-2003) provides acceleration of healing, pain relief and protection of the wound surface. In addition, the paste ensures high adhesion of the medicinal components introduced into the composition to the moist mucous membrane, and, as a result, guarantees long-term deposition of all medicinal components of the PAM on its surface. Hydrocortisone has an anti-inflammatory effect and also promotes epithelization of erosions.
Imudon is an immunostimulating agent prepared from a mixture of protein substances with antigenic properties, extracted by lyophilization from bacteria, which under normal conditions are causative agents of inflammatory diseases of the pharynx and oral cavity. The drug was used in the form of tablets, which were recommended to be dissolved in the mouth without chewing, at intervals of 2 hours.
The clinical effectiveness of the treatment methods was assessed by daily measuring the area of the altered mucous membrane using a millimeter grid according to the formula: S=m1+m2+m3+m4 / n, where m1, m2, m3, m4 is the area of each erosion on the inner surface of the cheeks, palate, gums and lips, n – number of measurements.
The patients were treated at the Regional Clinical Dermatovenerological Dispensary in Stavropol.
The research materials were subjected to mathematical processing on a personal computer using statistical software packages Exel 2007, Statistica for Windous 5.0. The results are presented as the arithmetic mean and its standard error (M±m).
Research results and discussion
Monitoring of erosion healing processes was carried out on days 7, 14, 21 and 28. It was noted that the effect of local treatment in the first group was significantly lower than in the second and third. The main disadvantage of local treatment of the first group was that the agents used were easily washed off with saliva and food, so the anti-inflammatory and angioprotective effect did not have a lasting therapeutic effect, and the healing of papules on the mucous membrane was slow.
On the 7th day, the characteristic mesh pattern remained on the oral mucosa in all patients of the first group; epithelialization was noted in 13.2% of formations. On the 14th day, epithelization of 20.4% of erosions was observed, on the 21st day – 39.5%. On the 28th day, epithelization of 45.6% of formations was observed.
Final healing of erosions by the end of the second month of observation was observed in only 2 patients (12.5%), in 5 patients of this group (31.3%) complete epithelization of erosions of the oral mucosa occurred within 2 to 3 months after the start of treatment.
In the second group, epithelization processes occurred faster than in the first, including due to the good adhesion of the ointment to the moist mucous membrane of the oral cavity. Observation of the patients of the second group on the 7th day showed that in all patients epithelization of 41.2% of papules occurred, on the 14th day healing of 51.4% of formations was noted and on the 21st day – 68.3% of papules. In 1 patient (5%) against the background of old papules, new elements of damage to the mucous membrane appeared. On the 28th day, healing of 73.5% of formations was observed. In 7 patients (35%) of this group, complete healing of mucosal papules was noted by the end of the second month of treatment. In the third group, on the 7th day in all patients, epithelization of 46.5% of formations was observed, on the 14th day - 75.2% of papules, on the 21st day - 91.7%, in 1 patient (5%) appeared new formations. On the 28th day, 95.1% of patients had complete healing of the papules of the oral mucosa. There were no allergic reactions or complications during treatment.
Clinical case
Patient S., 50 years old, amb card No. 3564.
Complaints: feeling of dry mouth, pain when eating. Objectively: there is a white hyperkeratotic plaque in the form of a mesh on the mucous membrane of the cheeks and tongue. The epithelium in some places sloughs off, revealing painful erosions (Fig. 3).
Rice. 3. Patient S., 50 years old. Lichen planus of the oral mucosa, typical form
Differentiated diagnostics with diseases similar in clinical picture were carried out. Excluded: flat leukoplakia, secondary syphilis, lupus erythematosus. To differentiate one type of keratosis from another, fluorescent light was used (in Wood's rays, lichen planus rashes glow pale blue).
Diagnosis: lichen planus of the oral mucosa, typical form.
Treatment. A course of general therapy was prescribed using sedatives (Persen, 1 capsule 3 times a day) and prednisolone 25 mg every other day.
Local treatment: use of the developed ointment 2-3 times a day in combination with the resorption of Imudon tablets (6-8 tablets per day). Already on the 14th day, healing of more than half of the formations on the mucous membrane of the oral cavity and lips was noted; the appearance of new papules was not noted. On the 28th day, complete healing and epithelization of changes in the oral mucosa were noted.
Conclusion
The data obtained showed that the treatment carried out in the first group was not effective enough compared to the second and third groups. The use of the developed ointment (second group), especially in combination with Imudon (third group), made it possible to accelerate the healing of papular rashes, prevent the development of complications and shorten the period of complete epithelization of the affected mucous membrane in lichen planus.
References: 1. Akinfeeva V.B. Treatment of the erosive-ulcerative form of lichen planus of the oral mucosa using "GalavitPL" / V.B. Akinfeeva: Abstract. dis. Ph.D. honey. Sci. – M., 2007. – 24 p. 2. Belyaeva N.S. Improving diagnostics and complex treatment in the clinical examination system of patients with lichen planus of the oral mucosa / N.S. Belyaeva: Abstract. dis. Ph.D. honey. Sci. – Perm, 2010. – 24 p. 3. Borovsky E.V. Diseases of the mucous membrane of the oral cavity and lips/E.V. Borovsky, A.L. Mashkileison // Guide for doctors. – M.: MEDpress, 2001. – 320 p. 4. Grigoryan A.A. Development and clinical application of a new wound-healing agent for the treatment of diseases of the oral mucosa in children and adolescents / Grigoryan A.A., Sirak S.V., Sirak A.G. [and others] // Modern problems of science and education. – 2013. – No. 2. – P. 41. 5. Libik T.V. Clinic, diagnosis and treatment of periodontal diseases in patients with lichen planus of the oral mucosa / T.V. Libik: Author's abstract. dis. Ph.D. honey. Sci. - Perm. – 2010. – 24 p. 6. Kochkonyan T.S., Gasparyan A.F., Bykov I.M., Ladutko A.A., Erichev I.V. Processes of lipid peroxidation and the antioxidant system of oral fluid during fixed prosthetics // Kuban Scientific Medical Bulletin. – 2008. – No. 3-4. – pp. 37-39. 7. Sirak S.V. Features of the choice of antimicrobial drugs for local treatment of inflammatory periodontal diseases in children and adolescents / Sirak S.V., Shapovalova I.A., Pugina Yu.N. [and others] // Pediatric dentistry and prevention. – 2008. – T.7, No. 4. – pp. 61-63. 8. Sirak S.V. Experimental study of the anti-inflammatory and regenerative properties of dental gel based on plant components, glucosamine hydrochloride and dimexide / Sirak S.V., Zekeryaeva M.V. // Periodontology. – 2010. – No. 1. – P. 46-50. 9. Sirak S.V. The use of a multicomponent adhesive ointment in combination with an immunomodulatory drug in the complex therapy of pemphigus / Sirak S.V., Kopylova I.A., Chebotarev V.V. [and others] // Periodontology. – 2012. – T. 17, No. 2. – P. 62-65. 10. Sirak S.V. Experience of using local wound-healing agents in the treatment of pemphigus vulgaris localized on the oral mucosa and lips / Sirak S.V., Chebotarev V.V., Sirak A.G., [etc.] // Medical Bulletin of the North Caucasus. – 2013. – T.8, No. 1. – pp. 59-62.
Treatment
For different forms of the disease, a different course of medications is prescribed. If the disease is asymptomatic, drug treatment may not be necessary. If erosions and ulcers have already formed, it is necessary to begin treatment as quickly as possible to avoid worsening the condition.
Inflammatory processes are controlled by the use of corticosteroids. Local treatment is carried out to relieve pain and accelerate tissue regeneration. To avoid the development of candidiasis, antifungal drugs are prescribed.
Electrophoresis and phonophoresis are also effective. In rare cases, when erosions do not heal for a long time, surgical intervention is indicated.
In all cases, without exception, the oral cavity is sanitized and the source of inflammation is removed (for example, periodontitis, caries or pulpitis).
How to cure lichen planus?
The composition and tactics of treatment for lichen planus depend on the degree of spread of the lesion, on the cause and localization of the pathology, on information about the effectiveness of previously administered therapy. Thus, treatment of the disease involves the use of systemic and external medications, as well as phototherapy.
Among the most effective medicinal groups of drugs for the treatment of lichen planus, experts identify:
- antihistamines;
- multivitamin complexes;
- antifungal agents;
- systemic corticosteroids;
- systemic retinoids, etc.