Anatomy and histology
Rice.
1. Microscopic specimen of a periodontal pocket in the area of the primary incisor of a 3.5-year-old child (normal): 1 — gingival margin; 2—remains of enamel cuticle; 3 - bottom of the gum pocket; 4—space that appeared in place of enamel that dissolved during decalcification; 5 - junction of the gum epithelium (6) with the enamel cuticle; 7 - tooth root; hematoxylin-eosin staining. The gum is usually divided into two parts: the cervical (pars collaria), adjacent to the necks of the teeth, and the alveolar (pars alveolaris). The alveolar part of the gum from the vestibule of the oral cavity repeats the bony alveolar elevations (juga alveolaria); on the lingual and palatal side, D. is more even. The edge of the cervical part of the gums (tsvetn. Fig. 1) is called the gingival edge (margo gingivalis). The gingival margin forms gingival, or interdental, papillae (papillae gingivales, interdentales), which stand in the interdental spaces formed by the contacting surfaces of the dental crowns and the interalveolar septum. The slit-like space between the gingival margin and the tooth, 1-1.5 mm deep, is called a gingival pocket; its lower border is the junction of the gum epithelium with the enamel cuticle (cuticula enameli) slightly above the neck of the tooth. With age, the epithelium of the bottom of the gingival pocket separates from the enamel cuticle and the bottom of the pocket deepens to the enamel-cement border (see Teeth). The formation of gingival papillae, gingival pockets, and gingival margins occurs during teething. In old age, after the removal or loss of teeth, the gum in the toothless areas of the jaw becomes denser, and the gingival papillae disappear.
The gum is immovably connected to the periosteum. A loose submucosal layer is present only at the transitional fold, which creates a smooth transition to the mobile mucous membrane of the cheeks and lips. In functional terms, D. is mutually connected with the periodontium (see) and the alveolus; it belongs to the fixing apparatus of the tooth and performs a barrier function.
Rice. 2. Microscopic specimen of human gums (normal): 1 - 3 - stratified squamous epithelium (1 - layer of keratinizing epithelium, 2 - granular layer, 3 - spinous layer); 4 - basal layer of epithelium; 5 - epithelial papillae; 6 and 7 - connective tissue base (6 - papillary layer, 7 - reticular deep layer); hematoxylin-eosin staining.
The gum consists of multilayered squamous epithelium and a connective tissue base (tsvetn. Fig. 2). On D., which is subjected to significant pressure during chewing, the epithelium becomes keratinized. The deepest, basal layer of the epithelium consists of cylindrical or cubic cells, above is a layer of spinous cells, then a granular layer containing keratohyalin grains and the superficial stratum corneum D. This layer of cells is constantly exfoliated; regeneration occurs due to basal and spinous cells. When teeth are lost, the epithelial layer thickens, and the stratum corneum is more clearly defined.
The connective tissue base of the gum consists of two layers: the papillary layer, located superficially, and the reticular layer, located deep. The papillary layer consists of loose connective tissue, forming papillae that project into the epithelium and are located radially towards the surface; vessels and nerves pass through them. Some bundles of collagen fibers are attached to the neck of the tooth and participate in the formation of circular fibers of the tooth (fibrae circulares dentis). The reticular layer of the connective tissue base consists of relatively thick collagen and elastic fibers, intertwined with each other and directly passing into the periosteum, which creates immobility D. Argyrophilic fibers D. form a subepithelial membrane in the form of a continuous mesh, lying in the papillary and reticular layers and in the connective tissue base between collagen fibers and around blood vessels. During the aging process, their collagenization occurs.
In the connective tissue basis of D., in addition to lipocytes (fat cells), fibroblasts, macrophages and mast cells, there are lymphoid elements.
Electron microscopic examination of D. revealed that the cells of the basal and spinous layers of the epithelium are closely connected by desmosomes (see), the cell nuclei contain large clumps of chromatin, their cytoplasm contains mitochondria and other organelles.
As one approaches the surface of the epithelium, the number of mitochondria in the cytoplasm decreases, which is apparently associated with a decrease in the activity of metabolic processes occurring in the cells. Rice.
3. Microscopic specimen of human gums (normal): lumps of glycogen (bright red) are visible in the cells of the spinous layer;
CHIC reaction with additional staining of nuclei with hematoxylin. Rice.
4. Microscopic specimen of human gums (normal): small clumps of RNA (bright pink) are visible in the cytoplasm of the cells of the basal and spinous layers; Stained with pyronin methyl green using the Brachet method.
A histochemical study of the gums made it possible to establish the presence of RNA in the cells of the basal and spinous layers. Glycogen is detected in the cells of the spinous layer (tsvetn. Fig. 3 and 4). In connective tissue cells, the RNA content is moderate. Neutral and acidic mucopolysaccharides are determined in the epithelium and connective tissue D. With secondary adentia, there is an increase in neutral mucopolysaccharides in the intercellular substance of the surface layers of the epithelial layer, and a decrease in acidic mucopolysaccharides in the connective tissue.
D.'s blood supply is provided by the gingival branches (rr. gingivales); small arteries predominate, which in the form of loopy branches, dense network-like plexuses and ball-like formations penetrate the connective tissue base D. Capillaries in the form of loops enter the connective tissue papillae and penetrate close to the gingival margin. D.'s capillaries are the most sensitive part of the circulatory system; by their condition one can judge the patol. changes in the body. The outflow of venous blood occurs through the veins accompanying the arteries.
The lymphatic network is divided into superficial and deep. The superficial lymphatic network is formed by lymphatic capillaries, at the confluence of which lacunar expansions are formed. The deep lymph, a large-loop network, is formed mainly by lymph vessels that are connected with the vessels of the periodontium and alveoli and flow into the submandibular, submental and deep cervical lymph. nodes.
Sensitive innervation occurs through the gingival branches (rr. gingivales) of the trigeminal nerve (n. trigeminus). The nerve branches extending from the main trunk of the gingival branch form a plexus, which is located in the connective tissue layer D. Penetrating into the epithelium, the nerve fibers lose their pulpy membrane, sometimes ending in button-like extensions.
The gum is characterized by tactile, thermal, cold and pain sensitivity.
What is gum recession
Normally, the gum tissue fits tightly to the surface of the tooth in the cervical area. It happens that for some reasons (about them in the next subsection of the article), the edge of the gums drops, exposing the neck of the tooth. This is called a recession. This defect is not only a deterioration in the aesthetics of a person’s appearance, but also the occurrence of negative consequences for teeth, bone tissue and, ultimately, for the health of the body as a whole. Without adequate measures, the prolapse can progress, exposing the tooth root. Pathology can develop at any age.
Research methods
In addition to examination, palpation, bacterial, research, they use capillaroscopy (see) and capillarography, which make it possible to establish the condition of the capillaries and determine capillary pressure. The completeness of the blood supply to the gums is determined using rheography (see). According to the proposal of V.I. Kulazhenko (1954), the permeability of capillaries is studied using an apparatus with a dosed vacuum. Counting leukocytes that have emigrated into the oral mucosa is carried out according to the method of M. A. Yasinovsky; in this case, it is possible to determine the intensity of the inflammatory process in the area of D. and the gum pocket during periodontal disease. To establish the severity of chronic inflammation in the D., the Schiller-Pisarev test is widely used: in the presence of an increased content of glycogen in the D., smearing it with a mixture of iodine and potassium iodide solutions gives a brown color, which is clearly visible with the help of a stomatoscope.
Cytol. The study makes it possible to establish the severity of inflammation in D., the quality of the body’s protective reaction, early diagnosis of certain diseases (for example, all forms of acantholytic pemphigus) and makes it possible to monitor the results of treatment. To determine morphol, characteristics of patol, the process in D., a histol study is carried out.
To establish the presence and distribution of D. glycogen, mucopolysaccharides, sulfhydryl and disulfide groups, RNA, and DNA in epithelial and connective tissue cells, histochemistry or cytochemistry is used. methods. The study of oxygen tension in D. is carried out using the polarographic method (the level of oxygen tension changes depending on the degree of periodontal damage). Normally, there is functional mobility of most receptor and effector apparatuses of the oral cavity. In the gum area, the sensitivity of nerve endings to temperature stimuli is determined using thermometry and thermography; Sensitivity disturbance is observed both in local and general pathology.
Treatment of recession
Treatment of gum recession is a complex of therapeutic and surgical measures taken to raise the gingival margin to a normal level. In the early stages of recession, conservative measures are effective; in the later stages, surgical intervention followed by drug therapy is necessary. The first priority is to identify the cause of receding gums. Without its elimination, recession treatment will not bring long-term results. For example, if a defect appeared as a result of gum disease, then without treatment, even after surgical lifting of the gingival margin, after some time the defect will reappear.
Important: experienced dentists (therapists, periodontists, surgeons) practice in our network of clinics. This allows for effective treatment regardless of the stage of recession. Experts warn: the sooner treatment is started, the faster it will be completed.
Pathology
Damage to the gums
observed with fractures and dislocations of teeth, with jaw fractures, as well as during tooth extraction surgery. Damage to D. can be caused by chemicals. substances, for example, arsenic in the treatment of pulpitis; in this case, necrosis D. may occur. Thermal burns are possible.
As a rule, due to the increased regenerative ability of the oral mucosa, damage heals quickly and no special treatment is required. If there is a significant rupture of D., sutures are placed on the wound; In this case, soft, non-irritating food is recommended.
Inflammatory processes
, acute and chronic, may be of local origin or be a symptom of a general disease of the body. Inflammation of the gums - gingivitis (see) - can occur as a result of the traumatic effect of an incorrectly manufactured denture, overhanging edges of a filling, or tartar; The pathological process may acquire the character of acute inflammation, hypertrophy or atrophy. Thus, often, as a reaction to chronic injury, granulations grow, which are partially or completely covered with a thin layer of epithelium, taking on the appearance of mushroom-shaped formations - gingival polyps.
D. inflammation occurs with pericoronitis, periodontitis (see), periostitis and osteomyelitis of the jaws (see Jaws); D. becomes swollen, hyperemic, and painful. D. is always involved in the process of periodontal disease (see).
Hyperemia and cyanosis of the gingival margin, as well as ulcerative gangrenous changes occur with C-vitaminosis (see Scurvy).
The gums, like the entire mucous membrane of the oral cavity, react to many pathol processes in the body, and gingivitis often occurs as a symptom of a general disease.
Often the first signs of diseases of the blood system are hemorrhagic, ulcerative-necrotic, hyperplastic processes in the D. In patients with gout. diseases due to the increased content of histamine in the blood serum, there is a persistent dilation of D.’s capillaries, which contributes to the occurrence of hron and inflammation in it. Some collagen diseases (systemic lupus erythematosus, scleroderma, etc.) are accompanied by catarrhal inflammation D. In some diseases of the cardiovascular system, radiation damage to the maxillofacial area, necrosis of the oral mucosa appears, which usually begins from the gingival margin.
Tuberculous lesion
D. is sometimes observed in active forms of pulmonary tuberculosis. At the same time, small gray-yellow tubercles appear on the D.; when they decay, painful superficial ulcerations of irregular outlines with seemingly corroded, pitted edges are formed, the gingival margin relatively soon becomes uneven, sometimes the epithelium of the bottom of the physiol. The gingival pocket loses contact with the tooth, a patol, gingival pocket is formed, and the necks of the teeth are exposed. Tuberculous lupus, when localized on the oral mucosa, according to G. A. Vasiliev and I. G. Lukomsky, also causes changes in the bone tissue of the alveoli, reminiscent of the picture of periodontal disease.
Syphilis
appears on the gums in all three periods. Hard chancre occurs more often in the area of the front teeth, sometimes in the form of a small spot of carmine-red color; in this case, an increase in regional lymph nodes is observed. Elements of the secondary period of syphilis on the oral mucosa are a spotted rash represented by papules, less often roseola. The tertiary period of syphilis is characterized by the appearance of focally located tubercles, usually in the area of two to four teeth, but a larger area may be involved in the process; the mucous membrane thickens, turns red, and becomes lumpy.
Actinomycotic process
in D. it develops as a result of the introduction of fungus through the patol, gum pocket;
There is no isolated D. lesion; actinomycosis of the soft tissues of the oral cavity usually develops. Rice.
1. Hard gingival fibroma (indicated by an arrow). Rice. 2. Fibromatous growth of the gums (indicated by an arrow). Neoplasms
. On D., a benign tumor on a stalk is more often observed - epulis (see). Fibroma D. also belongs to benign tumors (Fig. 1). Gingival fibromatosis differs from fibroma in the diffuse nature of the growth of fibrous connective tissue, the spread of the process to the gums as a whole; sometimes the disease is limited to several teeth (Fig. 2), often on both jaws. Fibromatous growths can cover a significant part of the crowns of the teeth and interfere with the closure of teeth and chewing. Unlike hypertrophic gingivitis, fibromatous gums are dense and there are no signs of inflammation.
A cancerous ulcer may be detected on the gum, usually resulting most often from a cancerous tumor of the jaw (see Jaws); Unlike an ulcer of inflammatory origin, it is painless, without a tendency to epithelialization.
Reasons for the formation of a recession
The main reason for receding gums is poor circulation in the tissues surrounding the tooth (i.e., periodontal disease).
The periodontium not only holds the tooth in the alveolus, but also nourishes the bone tissue. Without proper nutrition, bone atrophy begins, which, among other things, provokes gum loss. The process can be caused by a number of factors. What causes receding gum line:
- insufficient oral hygiene;
- improper brushing technique;
- formation of periodontal pockets;
- periodontal diseases;
- poor-quality dentures or incorrectly installed braces;
- mechanical, thermal and chemical injuries to the gums;
- pathologies of occlusion (malocclusion);
- metabolic disease;
- lack of nutrients and vitamins in the diet;
- age-related changes (physiological recession).
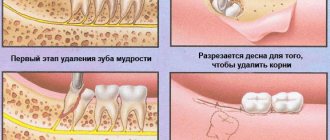
Operations
The most common operation on the gum is gingivectomy - excision of the D. area within the patol, gingival pocket for periodontal disease. Benign tumors are removed along with the surrounding gum, often with the periosteum. When cutting out trapezoidal mucoperiosteal flaps during surgery on the alveolar process, the incision is made along the bottom of the gingival pocket; when suturing such a wound, they usually strive to restore the anatomical relationships of all elements of D. In acute odontogenic inflammation (periostitis, osteomyelitis of the jaw), an incision to open the abscess is made along the transitional fold, i.e., along the border of the gum with the mobile mucous membrane of the vestibule of the mouth.
Bibliography:
Bolotina Z. L. and Mikhailovskaya T. S. Current state of the issue of gum biochemistry, in the book: Problems, ter. Dentistry, ed. A. I. Marchenko, V. 4, p. 5, Kyiv, 1969; Vorobyov V. and Yasvoin G. Anatomy, histology, embryology of the oral cavity and teeth, M.-L., 1936; Gemonov V.V. Histochemical study of the activity of some enzymes in the mucous membrane of the human oral cavity, Dentistry, No. 1, p. 30, 1969, bibliogr.; Zhilina V.V. Glycogen content in the gingival epithelium in normal and pathological conditions, in the book: Theory and practice of dentistry, ed. L. I. Falina et al., c. 5, p. 150, M., 1961, bibliogr.; Kulazhenko V.I. Periodontal disease and its treatment using vacuum, p. 36, Odessa, 1960; Novik I. O. Periodontal disease (pathogenesis, clinical picture and treatment), Kyiv, 1964; Rybakov A. I. and Ivanov V. S. Clinic of therapeutic dentistry, M., 1973, bibliogr.; Uvarov V. M., Rusak M. K. and Kalinin V. I. Organs of the oral cavity in diseases of the blood, L., 1975, bibliogr.; Falin L. I. Histology and embryology of the oral cavity and teeth, M., 1963; Eichel V. Oxidative enzymes of gingiva, - Ann. NY Acad. Sci., v. 85, p. 479, 1960; Kraus BS, Jordan RE a. AbramsL. Dental anatomy and occlusion, a study of the masticatory system, Baltimore, 1969; Listgarten MA The infrastructure of human gingival epithelium, Amer. J. Anat., v. 114, p. 49, 1964; Plenk H. Topo-histochemische Untersuchungen an den Nerven der Gingiva, in the book: Histochem. d. Ultra-struktur, hrsg. v. H. Zimmermann, S. 439, Jena, 1971, Bibliogr.; Rateitscha k KH Prophylaxe und Frtihbehandlung der Gingivitis und Parodontitis, Soz.- u. Pravent. Med., Bd 20, S. 309. 1975, Bibliogr.; Schroeder HE a. Munzel-Pedrazzoli S. Correlated morphometric and biochemical analysis of gingival tissue, J. Microscop., v. 99, p. 301, 1973; Schultz - Haudt SD Observations on the acid mucopolysaccharides of human gingiva, Oslo, 1957, bibliogr.; Schumacher G. - H. Odontographie, Lpz., 1972, Bibliogr.; Schumacher G. - H. u. Schmidt H. Anatomic und Biochemie der Zahne, Stuttgart, 1972.
I. F. Romacheva.
Non-invasive (conservative) treatment methods
The appearance of the first signs of a beginning recession is a signal for an immediate visit to the periodontist. At the very beginning of the disease, the problem can be solved without surgery. But the patient should prepare for a long, complex course of treatment. First, it is necessary to eliminate existing and potential foci of infection in the oral cavity. This means that you need to cure dental diseases (if any) and perform professional teeth cleaning using a hardware method. The second stage will involve curettage of periodontal pockets, after which local anti-inflammatory therapy (treatment of gums with special gels, ointments, solutions) will be prescribed. If necessary, the doctor will prescribe a course of antibacterial therapy (taking antibiotics).