Causes of candidal stomatitis
Normally, the yeast-like organism Candida is in the body of every person and does not harm him in any way. When certain conditions arise, fungi begin to actively multiply, which leads to inflammation of the oral mucosa. Such factors include:
- metabolic failures;
- diabetes;
- diseases of the endocrine system;
- hypovitaminosis;
- chronic pathologies of the gastrointestinal tract;
- long-term antibiotic therapy;
- pregnancy;
- use of birth control pills;
- bad habits (alcohol abuse, smoking), etc.
In addition to the mentioned endogenous (internal) causes of candidiasis, there are exogenous (external) causes. These are chemical and mechanical conditions that lead to disruption of the integrity of the skin and oral mucosa. These include: plaque and tartar, sharpened edges of teeth, uncomfortable dentures, chemical contamination, etc.
Stomatitis in children
Viral stomatitis
One of the most common contagious species. After the incubation period is completed, blisters form on the oral mucosa. Within a few hours they burst, turning into round or oval ulcers.
It is easy to “recognize” viral stomatitis in children: by its perfectly even shape and characteristic yellow coating on areas of erosion. Single spots often combine into larger lesions. The palate, tongue, and cheeks are inflamed and have a crimson-red tint.
Acute herpetic stomatitis
The second most common is herpetic stomatitis in children, the symptoms of which are the same as those of viral stomatitis. The onset of the disease resembles the flu: high temperature (up to 41°), aches, headache and muscle pain, enlarged lymph nodes.
First, a scattering of small bubble formations becomes noticeable (there can be quite a lot of them, up to twenty). They are grouped on the palatine arch, tongue, cheeks, and sometimes on the skin - near the lips and nose. The mucous membranes swell, the gums are also red and inflamed. In place of the burst bubbles, single or merged areas of erosion are formed, quickly becoming covered with a yellowish or whitish coating.
Recovery is long, from 10 days to two weeks. As a rule, infants who have reached six months of life and small children under three years of age become ill. During this period, the natural protection against the herpes virus obtained from the mother’s blood disappears.
Chronic herpetic stomatitis
Herpes is a virus that cannot be expelled from the body. Infection with it is also inevitable; in civilized countries, any person is a carrier of the infection. This is why herpetic stomatitis in a child with a weakened immune system periodically recurs. Provoking factors are colds, hypothermia, taking corticosteroid drugs, chronic tonsillitis, caries, microtrauma of the gums.
The external manifestation of the disease does not differ from the acute form of this type of stomatitis: the same blisters and ulcers. However, with a chronic course of the disease with periodic exacerbations, there is no acute period: there is no jump in temperature, the child remains active, although the lymph nodes enlarge.
Chronic aphthous stomatitis in children
The disease often develops against the background of food or drug allergies, so children with identified allergopathology are at risk. The treatment of stomatitis in children with this feature is also carried out together with the dentist by an allergist, and sometimes by a gastroenterologist.
Outwardly it manifests itself as the formation of painful round lesions covered with a dense grayish coating - aft. All aphthae have a clear shape and a bright rim. They are much larger in size than ulcers: they can reach 5-10 mm.
Unlike herpetic manifestations, with aphthous stomatitis the rise in temperature is slight, although there is weakness, the gums do not swell or redden. Aphthae are few in number (sometimes one lesion appears on the tongue or under the tongue, on the cheek), touching them causes severe pain.
The disease is provoked by staphylococcus, a microbe that lives in carious teeth and dental (soft) plaque. The disease appears more often if the child has congenital, acute or acquired pathology of the gastrointestinal tract, or some kind of immune disorder.
Bacterial stomatitis
Painful areas of bacterial stomatitis are small in size, uneven, and covered with a dense yellow coating. Sometimes yellowish dense crusts form on the baby’s lips, there is a clear putrid smell of breath, and drooling occurs. Mucous membranes are inflamed, dark or purple-red. It can be seen that the gums are loose and bleeding. The general condition also suffers: there are complaints of aches, headaches, and nausea.
Bacterial stomatitis in children is caused by staphylococcal and streptococcal bacteria. Treatment must be specific, fast and correct.
Candidal stomatitis
Candida fungi cause this type of disease that affects newborns. A characteristic sign of the disease is the formation of a cheesy, homogeneous milky coating over the entire area of the tongue and cheeks, on the gums, and sometimes on the lips. If this layer is removed, a painful, bleeding ulcer will be exposed.
A characteristic sign is the appearance of a sour odor from the infant’s breath. The baby does not take the breast and bottle and is capricious.
General approaches to the treatment of childhood stomatitis
Depending on the type of stomatitis in children, treatment will vary significantly. Nevertheless, there are general principles, the observance of which will alleviate the baby’s condition and will not aggravate the course of the disease.
- Careful oral care is necessary: antiseptic rinsing before and after meals, mandatory but careful brushing of teeth with a brush with the softest bristles. Infants can wipe the inside of their cheeks with a special napkin soaked in an antiseptic composition.
- Food for a sick child should be warm, so as to cause as little pain as possible when chewing. Spicy, sour, irritating mucous membranes and solid foods are prohibited. Purees, broths, and pureed porridge are preferred. Whole milk and juices should be excluded for a while.
- On the recommendation of a doctor, you can apply an anesthetic gel or spray to the gums and mucous membranes before meals.
- To recover faster, your baby needs to drink plenty of fluids.
The dishes of a sick child should be kept separately and carefully handled, especially if there are other children in the house. It is important to provide him with a separate towel and toys. If a newborn is sick, nursing mothers should definitely take care of the cleanliness of their breasts, nipples, and bottles.
The most important point, common to all types of disease, is not only timely and correct, but also sufficient treatment. This means that even with significant relief of the condition, you need to complete the course of taking medications prescribed by your doctor. If treatment is interrupted earlier, pathogenic pathogens will form a persistent defense against drugs, and it will become difficult to fight them.
Treatment of acute and chronic herpetic stomatitis
The acute form is treated with antiviral drugs that are effective against herpes. If the disease has become chronic, then additional immunomodulatory drugs will be required. To relieve the first acute symptoms, the doctor will prescribe an antipyretic, but only if the temperature is above 38.5°. At a lower temperature, you need to give the baby’s immune system the opportunity to work - the immunity will be stronger.
The main drug used to combat viruses in the oral cavity in dental and pediatric practice is Acyclovir. It successfully destroys herpes, but only at the first stage, when a vesicular rash forms. From the moment the ulcers form, ointments and gels are used for local treatment.
Viferon restores immunity well and destroys viral infection. Thanks to interferons and a vitamin complex in its composition, it quickly alleviates the condition of a sick child, especially if used in the first hours of illness. Available in convenient forms: candles are suitable for newborns and one-year-old babies, gel and for older children.
The third mandatory component of the treatment of stomatitis in children is frequent antiseptic rinsing. It is important that only the drug that is active against herpes viral infection will work. Miramistin is usually prescribed. There is no point in rinsing your mouth with herbal infusion.
It is good to treat ulcerated areas with Cholisal gel, which both heals and relieves pain for several hours. Sea buckthorn oil, Aekol, and wild rose (rose hip) oil have a strong healing effect. They are used topically, applied to the mucous membrane.
If the disease returns, that is, becomes chronic, then immunomodulatory drugs are included in the treatment regimen. You cannot use them on your own or violate the recommendations of the instructions: this is fraught not with an increase, but with an even greater decrease in immunity. Effective immunomodulators, for example, Immunal, Imudon, Amiksin.
Additionally, special pastes enriched with enzymes will enhance immunity in the mucosal area.
Signs of the disease
Symptoms of fungal stomatitis vary depending on the degree of inflammation, the characteristics of the patient’s body and his age.
Signs of candidal stomatitis in young children are presented in the form of white cheesy plaques in the mouth. Parents often confuse them with leftover dairy foods. When plaque is removed, ulcers and erosions appear on the child’s mucous membrane and tongue. As the disease progresses, additional signs appear:
- the mucous membrane swells - it is difficult for the child to swallow;
- eating causes pain and discomfort;
- the patient loses appetite;
- When the infection penetrates the intestines, abdominal pain and digestive problems appear.
Symptoms of oral thrush in adults begin with a burning sensation in the larynx. Then a yellowish film appears on the mucous membrane and tongue, and when removed independently, blood is released. The patient complains of loss of taste, metallic taste. With chronic inflammation, the patient has a dry mouth and pain when swallowing.
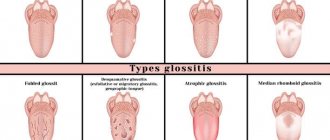
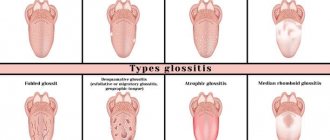
Externally, fungal stomatitis in adults and children can manifest itself as glossitis (infection of the tongue) or as candidiasis.
Treatment of thrush
Stomatitis or thrush in infants can cause a rapid increase in temperature and inflammation of the lymph nodes. Foci of thrush localization occur on the lips, cheeks, and tongue, but can also cover the pharynx.
The mucous membrane becomes covered with a cheesy, white coating. In the initial stages of the disease, it can be easily removed with a bandage soaked in a soda solution. All the mucous membrane underneath will be red and inflamed.
In case of mild illness, the temperature may not rise or be low-grade. A child who is bothered by thrush eats poorly and experiences pain.
Itching, dryness, burning, inflammation cause a lot of discomfort and trouble for the baby. Parents have a question: when can a child feel relief?
With normal care, following all doctor's recommendations and treating the oral cavity with soda solution, symptoms may disappear after 3-6 days.
In breastfed children, after each feeding, the mucous membrane in the mouth and the mother's peripapillary area should be treated with a soda solution.
Gel "Myconaz"
If necessary, your doctor may prescribe antifungal medications. Candide lotion and Miconaz gel have proven effectiveness; they are approved for use from birth.
A fungal infection lowers the pH level , and an acidic environment only promotes the development of fungi. To neutralize the acid and restore the alkaline environment, treatment with a 2% baking soda solution is necessary.
Types and forms of pathology
In practice, acute and chronic oral candidiasis occurs. The first develops rapidly, the second is characterized by a sluggish course and vague symptoms, periodic relapses and inflammation.
Acute fungal candidal stomatitis can be pseudomembranous (white plaque is easily removed and reveals reddened areas) and atrophic (there is no plaque, the mucosal surface dries, turns red and becomes painful).
Chronic thrush can be hyperplastic (white or grayish cheesy plaques form on the soft tissues) and atrophic (the oral mucosa dries out, becomes thinner, the patient complains of pain and discomfort).
How to treat fungal stomatitis?
In order not only to reduce inflammation of the mucous membrane, but also to prevent relapses, treatment of candidal (fungal) stomatitis in adults and children is carried out only in a comprehensive manner. Therapy involves taking several drugs at once:
- antimycotics – antifungal drugs for topical use;
- local antiseptic solutions for rinsing and irrigation (to prevent additional infection);
- antihistamines (recommended for the development of allergies to fungal activity);
- vitamin complexes (to eliminate deficiency of substances in the body).
To speed up recovery, the patient will have to follow a special diet. It is necessary to restore the mucous membranes of the oral cavity and pharynx.
Often sick patients are interested in how to treat candidal stomatitis at home, putting off going to the dentist. But it is impossible to cure candidiasis at home. Probably, it will only be possible to relieve the acute symptoms of the pathology, which will manifest itself again after a while. To prevent inflammation from becoming chronic, you should consult a doctor as soon as you notice the first symptoms of the disease.